It's rare to see a person without small dark marks on their body. Is it worth paying attention to these points? Only a doctor will distinguish between dangerous and normal moles - malignant melanoma or harmless nevus - and give recommendations on what to do with them. Is it worth worrying about the appearance of new formations, when immediate contact with specialists is required, what are the signs of cancer development - the answers to these questions remain to be found out. No one is immune from disaster, and early diagnosis will protect you from severe consequences.
What is a mole
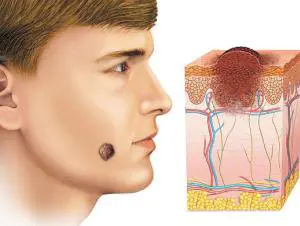
The first tiny spots may appear in children in infancy. A mole is a small formation on the skin - a nevus - that is considered benign and harmless. The basis for their appearance is melanocyte cells that accumulate the natural pigment melanin. Depending on its quantity, a difference in color is observed. Available colors:
The shape of the tumors depends on the location and concentration of melanin. They may have a stalk or be located under the skin, be flat and convex. The most common type is round, but there are exceptions. The development of neoplasms is provoked by ultraviolet radiation - natural from the sun, in a solarium. Hereditary factors cannot be excluded. A common cause of growth is hormonal imbalance, characteristic of periods:
- puberty;
- pregnancy;
- menopause.
What types of moles are there?
One person may discover very different tumors. Types of moles are classified according to several criteria. This helps in correct diagnosis in case of changes. They differ in:
- origin– congenital, newly acquired;
- structure– pigment, vascular;
- place of education – in depth, on the surface, in the boundary layer;
- raised above the skin – flat – even, protruding as a hemisphere, pedunculated, larger birthmarks;
- potential threats – dangerous, degenerating into melanoma, non-dangerous.

Safe moles
Those who have dark spots on their skin should be wary of their changes. In time, detected signs of degeneration into melanoma contribute to the timely removal of the formation and preservation of health. Safe moles are different:
- the presence of a stalk – it cannot be formed by malignant cells that grow randomly;
- long-term condition without changes.
Spots that appear soon after birth are not considered dangerous. It is important that they are small in size. Good – non-dangerous – signs of neoplasms include:
- flesh tone;
- unchanged pattern of the skin of the nevus and adjacent tissues;
- soft consistency;
- hair on the surface of the neoplasm - growing from the skin, indicates the absence of pathologies;
- diameter no more than 5 mm;
- symmetry;
- nevus in the form of a spot.
Which moles are dangerous?
Why do people with nevi on their bodies need to monitor their changes? There is always a threat of degeneration of non-dangerous tumors into a cancerous tumor. What moles are dangerous to health? Key signs you need to know:
- change in shades towards the dark side, the appearance of multi-color;
- rapid increase in size - exceeds two millimeters per year;
- occurrence of cracks;
- the formation of asymmetry due to uneven growth;
- lack of elasticity;
- the appearance of itching, burning;
- presence of discomfort.
The appearance of dangerous moles requires an immediate visit to a specialist to clarify the nature of the changes and the likelihood of developing skin cancer. Pathological transformations provoke:
- injury to the nevus due to negligence;
- self-removal;
- abuse of exposure to the sun, use of a solarium;
- location of the formation in places of frequent contact with clothing - on the neck, head, genitals, legs;
- placement in the hair, on the face, palms - where there is a high probability of injury;
- previously removed melanoma.

Why are moles dangerous?
Not a single person is protected from the sudden proliferation of cells of a harmless mole. Melanoma is an extremely serious disease. Changes not detected at the initial stage can result in death. The provoking factor is unsuccessful independent removal of tumors. Moles are dangerous because of their ability to:
- transform into an atypical – precancerous form;
- grow to large sizes;
- turn into cancerous;
- with minor external changes, metastases actively spread throughout the body through the circulatory and lymphatic channels.
How quickly does melanoma develop from a mole?
The transformation of a nevus into a cancerous formation can occur in different ways. The process depends on the stage of the disease and the type of tumor. Instant metastases are dangerous. Begins:
- growth of cancer (oncological) cells in the deep layers of the epidermis;
- their entry into the blood and lymph;
- penetration into the lungs, liver, kidneys;
- growth in these organs;
- complete damage to the body;
- death.
The growth phases of pigment cells are observed, along which melanoma develops from a mole. There are varieties:
- horizontal– damage to the upper layers of the skin occurs, lasting up to 10 years, but metastases do not appear;
- vertical– accompanied by the spread of cancer cells throughout the organs, can last two years, has an unfavorable prognosis;
- nodal – especially dangerous – characterized by deep spread within two months.

The first signs of melanoma
The patient can be assisted only when suspicious changes begin to be identified. The diagnosis, research, and referral for surgical treatment save a person’s life. The first signs of melanoma:
- increase in the height of the tumor;
- bleeding;
- the appearance of discharge;
- redness;
- burning, itching;
- swelling of tissues;
- softening of the nevus;
- the appearance of a crust;
- thickening;
- hair loss;
- expansion of pigmentation around the lesion.
With the further development of dangerous melanoma, the following are observed:
- significant change in size;
- the appearance of pain;
- enlarged lymph nodes;
- surface ulceration;
- formation of new foci;
- bleeding from places of pigmentation;
- liquid separation;
- skin thickening;
- the appearance of an earthy tint;
- signs of metastases are chronic cough, weight loss, cramps, headaches.
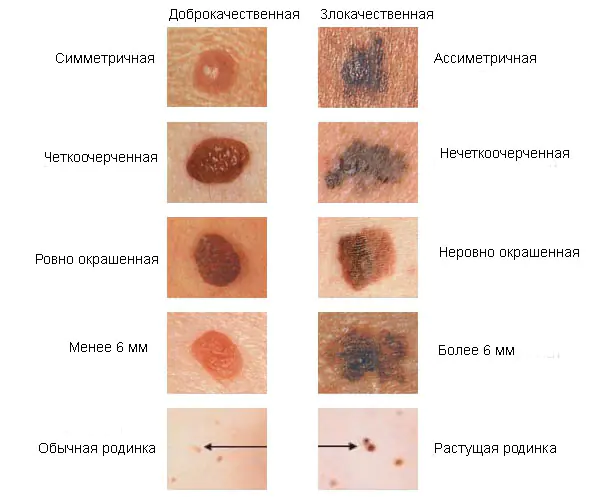
How to distinguish a mole from melanoma
To recognize which moles are dangerous and which are not dangerous, you need to know what they look like. A person with nevi, in order to avoid dire consequences, must constantly monitor the appearance of new formations and changes that occur. You can distinguish a mole from melanoma by its signs. Non-dangerous neoplasm:
- symmetrical;
- with smooth edges;
- uniform in color;
- with dimensions not exceeding 6 millimeters.
Features of dangerous melanoma that require seeking help from dermatologists:
- growth in a short time;
- pronounced asymmetry of shape;
- heterogeneity in color - the presence of inclusions of several shades;
- lack of clear boundaries - the contour line is blurred, jagged, and looks like a coastline on a geographical map;
- increased diameter over six millimeters;
- variability of any parameters - color, size, shape.

What dangerous moles look like
What do nevi that are subject to pathological changes look like? Only a doctor can correctly distinguish between non-dangerous tumors. Dangerous formations look like this:
- blue– compactions under the skin with clear boundaries, with dimensions no more than 10 mm;
- nodal– round, flat in shape, color – brown, black;
- cutaneous– often pale, convex;
- halo nevus – pigment surrounded by a light or white rim;
- spitz- looks like a dome-shaped tumor of pink shades, with the possible presence of a hole through which blood and liquid leak;
- connecting- connect individual entities into a whole.
Mole with jagged edges
One of the signs of a non-hazardous formation turning into a dangerous one is a change in contours. It often has blurred edges and scalloped borders. There are non-dangerous types of nevi - dysplastic. Only a specialist can make a correct diagnosis. A mole with uneven edges can be dangerous if there are additional signs of melanoma:
- accelerated changes in size;
- the presence of clearly defined asymmetry;
- the appearance of highly indented boundaries.
Rough mole
Such a neoplasm is harmless if its diameter is no more than 5 mm and remains constant in size. Often its appearance signals a lack of vitamins and nutritional disorders. Doctors advise coming for a consultation if it is discovered that:
- the smooth nevus turned into a rough one;
- bothered by burning, itching, tingling;
- irregularities and compactions appeared in the middle;
- areas with different shades formed;
- diameter has increased significantly.
A dangerous rough mole requires immediate examination if:
- the appearance of bleeding;
- development of the inflammatory process;
- rapid change in size;
- formation of asymmetry;
- formation of purulent discharge;
- the occurrence of painful sensations when touched;
- the emergence of an irregular shape, blurred boundaries, along the edges of the neoplasm.

Large moles
Large formations on the skin are pigment spots. When they remain unchanged and do not cause inconvenience, this is not a dangerous phenomenon. It is important to constantly monitor their appearance, color, and size. To eliminate worries, you need to consult a dermatologist. During the visit, the specialist will conduct a diagnosis and give a forecast of the risk of developing a malignant neoplasm. Large moles become dangerous if they:
- injured;
- thickened;
- started to itch;
- were unsuccessfully removed independently;
- changed in size, shape;
- are bleeding.
What moles can be removed
Often nevi cause trouble for women when they are in a visible place - the face, neck. Even if they do not bother you, using removal will be the right decision - the appearance will improve significantly. After the procedure, the doctor must necessarily send the tissue for histological analysis to decide whether the mole is malignant or not. If the neoplasm is not dangerous, does not bother you, and does not change in size, surgery is not required. What moles cannot be removed? Experts believe:
- there are no contraindications;
- It is important to choose the right excision technique.
You should be careful about skin growths; it is unacceptable to remove them yourself. Only the doctor will determine whether a nevus is dangerous or not and decide what to do with it. You can delete it if:
- injured from clothing - on the neck, in the groin area, under the armpits;
- cause pain when touched;
- are located under the hair on the head and can be damaged when combing or cutting;
- change color, shape, outline;
- significantly increase in size;
- characterized by the presence of burning, itching;
- accompanied by inflammation and bleeding.
Moles, birthmarks on the skin of newborns
A birthmark is a very familiar phenomenon to everyone. The name itself reflects its essence: what these different types of skin formations have in common is that they are found in a child immediately after birth or appear in the first year of his life. Should you worry if you see moles on your baby's skin?
Nevi (as birthmarks are called in scientific language) are focal changes in the skin, representing dysplasia (excessive development or, less commonly, underdevelopment) of one or more of its structural elements. As you know, the skin consists of the epidermis - the upper layer (cuticle), the dermis (a kind of base of connective tissue, which contains hair papillae, blood and lymph vessels, sebaceous, sweat glands, nerve endings) and subcutaneous tissue. Nevus can form from every layer of skin.
The following types of nevi are distinguished depending on the tissues from which they are formed: 1) melanocytic, 2) non-cellular, 3) organoid (from epithelium, from connective tissue, from blood vessels, from adipose tissue). In total, each type includes 20-30 different nevi; thus, there are more than a hundred varieties. Of course, the subject of our conversation will not be all, but only the most well-known and common types of birthmarks that can be found in a baby.

Dark spots
The first two types of nevi (melanocytic And noncellular) consist of melanocyte cells containing the pigment melanin, which protects a person from excess solar ultraviolet rays and thanks to which the skin acquires a pleasant tan color. When pigmentation is disturbed, melanocytes can form both areas of accumulation and areas of rarefaction. Accordingly, areas of accumulations will look darker than normal skin, and areas of rarefaction will appear lighter. Melanocytic and noncellular nevi are also called pigment spots; We will look at them in more detail.
The intensity of the color of such a spot depends on the depth of melanin in the skin and can be from blue to black, but more often moles, as is known, are brown. Pigment spots occur equally often in both boys and girls and can be present in a newborn baby or appear throughout a person’s life.
The number of spots can vary from a few to several hundred, and the size - from a few millimeters to 15-20 cm or more. They are painless to the touch and have no signs of inflammation (redness, swelling). The consistency of pigment spots can vary from very soft to very dense.
Giant pigmented nevus already occurs in newborns. It is located symmetrically on both sides of the body or on one side, occupying large surfaces of the body. A giant nevus can take the form of a “bathing suit” or “panties”, imitating the corresponding items of clothing in its appearance and location. It is often covered with a large amount of hair, which is why it received another name - pigmented hair nevus.
Blue nevus appears in infancy, its size is 0.5-2 cm, the color is gray-blue or blue, which is where its name comes from. Most often located on the face, upper extremities, less often on the torso.
Halo-nevus (from the Greek halos - “rim”) - one of the forms of pigmented nevus. It appears more often throughout life, but can also occur at birth. This nevus is a round or oval nodule, dark brown in color, 2-5 mm in diameter; it is surrounded by a wide rim of light skin (which is how it got its name). Most often, halo-nevus is located on the skin of the trunk and upper extremities.
Mongolian spot - a bluish-red, dark blue, blue-black or brown flat spot that looks like a bruise. It is usually located in the sacrum area, on the buttocks, and less often on the lateral surface of the thighs. More often (in 90% of cases) such a spot occurs in representatives of the Negroid and Asian races, less often (3-10%) - in representatives of the Caucasian race. In some cases, it disappears on its own by the age of 7 years.
What are hemangiomas
Nevi from vascular tissue (hemangiomas) are 2-3 times more common in girls than in boys. Hemangiomas are formed from a deeper layer of skin than pigmented birthmarks, so their formation sometimes involves not only blood vessels, but also nerve endings. In this regard, there may be some pain or increased sensitivity of certain types of hemangiomas. Hemangiomas form in a child inside the womb. Their size can range from a few square millimeters (the size of a pinhead) to 100 cm 2 and more. The color of hemangiomas can vary from pink to dark red or burgundy. There are a large number of their varieties; We will list just a few.
Flat hemangiomas - somewhat elevated surface spots, consisting of the smallest vessels (capillaries) and having a color from pink to red-violet. These hemangiomas account for up to 96% of all hemangiomas. Their size and shape can be very different.
Stellate angioma often observed in children on the skin of the face and neck in the form of a central ruby point, from which small arterial vessels spread in the form of star rays. May disappear spontaneously by 2 years of age.
Tuberous-cavernous, or cavernous, hemangioma - elastic, bluish-red with a brownish tint, sometimes warm to the touch. It rises above the surface of the skin and has an uneven, bumpy surface. It can be located deep in the skin and therefore have the color of normal skin. This hemangioma consists of blood-filled cavities delimited by connective tissue septa. Usually it is of considerable size, most often located on the face, scalp, less often on the limbs, buttocks, and sometimes on the mucous membrane of the mouth. It may be painful when pressed and gives a sensation of pulsation. Some tuberous-cavernous hemangiomas regress (gradually decrease and sometimes disappear) throughout life, but some require therapeutic or surgical treatment.
Strawberry hemangioma - flat, bright red formations with clear boundaries, most often found on the face. 70% of them resolve spontaneously by age 7.
If treatment is required.
The question of the need for treatment of hemangioma, as well as the timing and methods of such treatment, is decided by the oncologist on an individual basis. Its decision depends on the type of hemangioma, its location, size, the rate of its growth (if growth occurs), as well as on the condition of the child. Small hemangiomas are removed entirely surgically - on an outpatient basis and without any particular problems. Large hemangiomas and hemangiomas located on the face are also treated in non-surgical ways: exposure to low temperatures, injection of certain chemicals that cause the collapse of dilated vascular cavities. Laser treatment is also used. Cold exposure (cryotherapy) is usually prescribed for superficial hemangiomas on exposed areas of the body. After cryotherapy, an inflammatory reaction occurs at the site of freezing, which disappears by 7-12 days. By this time, the crust falls off and the surface covered with new epithelium becomes visible. Hemangiomas can be cured in this way in 93% of cases, and the scar formed after healing is almost invisible.
Hemangiomas themselves are fairly harmless and usually do not need treatment until age 2 unless they grow or change structure. But in some cases they are one of the manifestations of syndromes (a syndrome is a set of symptoms, knowing one of which one can suspect others). Syndromes are usually inherited.
There may be formations on the skin of a newborn that have little in common with “birthmarks,” but are similar in appearance.
Toxic exanthema is small areas of redness of the skin, most visible at 48 hours of life. They disappear on their own over time.
Telangiectasias are often a physiological phenomenon; they are rudimentary remains of embryonic vessels in the form of reddish-bluish spots located on the back of the nose, the border of the scalp, the back of the neck, the upper eyelids, and lips. They usually disappear by 1.5 years of age and do not require treatment.
Medial spots are found quite often in newborn babies. These are pinkish spots that do not rise above the skin, located along the midline of the forehead, on the back of the nose, on the eyelids and on the back of the head. When the baby is in a calm state, these spots are practically invisible - they appear only when screaming or crying. The appearance of the spots is similar to flat hemangiomas, with which they are often confused. Medial spots, which are located on the face, usually disappear at 10-12 months of age.
Isn't this dangerous?
The small pigment spots that most of us have are only minor cosmetic defects and are not dangerous. But those who have large pigment spots measuring more than 5-10 mm should not actively sunbathe or go to the solarium. This applies more to those with multiple spots. Pigment spots, as mentioned above, are accumulations of melanocytes, and a hemangioma, despite its benign quality, is still a neoplasm, therefore it is extremely undesirable to expose both pigment spots and hemangiomas to ultraviolet irradiation (under the sun or in a solarium), since increased insolation can provoke malignant degeneration of benign neoplasms. Pigment spots with intense irradiation, in addition to producing melanin and darkening, can also begin to actively divide, thus degenerating into a malignant tumor - melanoma. True, it is rare in young children.
be careful
If any formation is detected on the skin of a newborn, parents need to bring it to the attention of the attending pediatrician, and if there is a noticeable growth or change in the structure of the birthmark, the appearance of inflammation, additional rashes around it, or an increase in the intensity of the color, they should definitely contact a pediatric oncologist. The doctor will be able to determine which of the above formations this birthmark resembles and whether it is a manifestation of any disease or syndrome. In any case, it is advisable to trace the detected formation on tracing paper immediately after birth and monitor its further growth.
Mom should also pay attention to ensuring that the birthmark is not constantly irritated by tight-fitting clothing, which can lead to its growth or damage with subsequent infection.
Moles in medical terminology they are called nevi.
They can be found on the body of any person in the form of small round dots, small spherical formations that rise above the surface of the body, and large pigmented areas of the skin.
What it is?
Moles consist of specialized cells of the epidermis - melanocytes, responsible for the production of melanin in the body (a pigment that colors the skin in various shades of brown). Under the influence of external or internal factors, an excess amount of them accumulates in certain places of the skin - this is why moles appear on the body of an adult, child or elderly person.

In some people, nevi remain unchanged on the skin all their lives, in others they disappear, in others they grow or change their shape and color. The latter become dangerous and can degenerate into malignant formations.
- Common moles have a rounded symmetrical shape, depending on the concentration of melanin in them, nevi are colored beige, brown or black.
- Meet and red dots on the body as moles, for the most part this phenomenon is associated with impaired skin pigmentation due to hepatic or endocrine pathology, as well as natural age-related changes (i.e. as a result of aging).

The difference between these spots and moles is that they usually appear in groups on a limited area of the skin. When metabolic processes are restored, the red spots disappear.
In adults, the appearance of nevi is associated with hormonal crises due to illness, menopause or nervous exhaustion. The appearance of moles in them can be observed constantly or appear spontaneously, in response to a certain stimulus. In childhood, science has noted the wavy growth of nevi.
Periods when moles appear in children:
- 6 months - six months, at this moment the child’s endocrine system adapts to external conditions;
- 5-7 years, the stage of active growth of the skeletal system and skeletal muscles, requiring rapid metabolic reactions;
- 12-16 years, puberty with significant changes in the functions of the whole organism.
Why do they appear?
Nevi are essentially benign skin formations.
Some people get scared when they see many moles on their body. What does this mean for a specialist? Only that the patient’s body is prone to accumulation (accumulation) of melanin in the surface layers of the epidermis.

The reasons for the appearance of numerous or single nevi are varied.:
- exposure to ultraviolet radiation, one of the most common factors in the formation of moles due to increased melanin levels during tanning;
- traumatic damage to the epidermis, systematic violations of the integrity of the skin contribute to the appearance of pathological changes in it;
- exposure to radiation, which rapidly changes normal skin cells;
- consumption of harmful products (GMOs, fast food, alcohol) and smoking, these habits negatively affect metabolic processes in the body.
- endocrine disorders and diseases, any changes in hormonal levels can cause the appearance of skin pathologies, pigmentation, moles;
- hereditary predisposition, the presence of various nevi in the family.
Classification and photo
1. A flat nevus or birthmark is a pigmented island of skin with clearly defined boundaries. It can take the form of lentigo - multiple brown or brownish formations in the upper layers of the epidermis.

2. Convex nevus or mole. It has a diameter of up to a centimeter, a smooth or lumpy surface and rises above the level of the skin. Its color varies from beige to black, and a hair is usually located in the center of such a formation.

3. Blue nevus or blue mole. It looks like a smooth hemisphere, slightly raised above the skin, sometimes reaching a size of 2 cm. The color of this benign formation ranges from blue to dark blue.
4. Giant nevus. It is a large spot on the body, gray, bright beige (sometimes brick), black or brown.
Dangerous and non-dangerous moles
Ordinary nevi do not cause any discomfort to their carriers; sometimes they even disappear without a trace. Their shape is stable, size and color remain unchanged.
But benign moles are sometimes removed to prevent their degeneration if they are of rather large size (pedunculated) and are located in areas of the body where a person constantly injures them (during vigorous activity or parts of clothing).

Remember dangerous moles in the photo and be vigilant!
If nevi degenerate into cancerous moles, this is dangerous, since such neoplasms quickly metastasize to other organs.
Therefore, it is very important to see signs of malignancy in time.:
1. The shape of the mole changes, it loses its symmetry and begins to grow in one direction.
2. The edges of the nevus become uneven (“cut up”, “torn”).
3. The color of the mole is uneven and contains yellow, red or black inclusions.
4. The nevus grows or “shrinks”, its size changes quickly.
5. The texture of the mole becomes different, smooth becomes rough, bumpy becomes flat, etc.
6. Loss of hair growing from the nevus.
7. Itching, peeling and burning in the mole area.
There are several reasons why a nevus itches:
– pathological cells multiply;
– there are active processes of death of healthy tissues;
– the area around the formation becomes inflamed and swollen.
8. The appearance of microcracks and ulcerations.
9. Bleeding and soreness of the mole.

Cancerous moles (melanomas): photo
What happens if you rip off a mole?
You cannot remove a nevus yourself.
Firstly, it is dangerous, and secondly, it is simply ineffective. If the mole is located close to blood vessels, prolonged bleeding may develop. Often such self-medication leads to re-formation of the nevus, its growth or malignancy.

Therefore, it is difficult to predict what will happen if a mole is torn off. It may have no consequences, or it may cause serious complications for the health and life of patients.
Doctors warn that any trauma to the nevus is extremely undesirable, but pedunculated moles or small convex formations can be accidentally removed with nails or hard items of clothing.
What to do if you rip off a mole:
- cauterize the wound with an alcohol solution;
- stop the bleeding by applying a gauze bandage;
- come to see a specialist.

In cases of partial removal of a mole, do not touch the remaining formation, do not cut it off or tear it off.
Sometimes such pigmentation appears before the disappearance of a mole (as a sign of depigmentation), and in other cases it may signal its degeneration.
White spots around the mole appear as a characteristic sign of Setton's nevus. This formation is considered harmless in terms of degeneration into a more malignant form, however, melonomas (aggressive cancerous formations) can also have such a white rim, so the appearance of white spots is a reason to contact a medical specialist.
Diagnostics
Dermatologists and oncologists are involved in determining the type of nevus.
Using a dermatoscope, the doctor examines the formation and determines its nature (benign or malignant). Sometimes a histological examination (scraping method) is required.
Biopsy (tissue sampling) for nevi is not used due to their trauma during this procedure. And as you know, it’s better not to touch moles again!
Removal
Many people want to get rid of birthmarks and nevi not only in cases of malignancy (pathological change), but also to correct a cosmetic defect.


However, removal is carried out at the oncology center for people with malignant tumors and with a high probability of degeneration of nevi.
Often the indication for surgery is the localization of moles on the body: on the scalp, on the neck, on the chin, in the area of the shoulder blades.
Methods for removing nevi (with information on how much it costs to remove them):
- surgical, using local anesthesia and a scalpel (in municipal surgical hospitals, according to indications - free of charge, in medical centers from 300-500 rubles)
- cryofreezing with liquid nitrogen (1000-1500 rubles);
- electrocoagulation - cauterization with electric current (600-1300 rubles);
- photodynamic - ultraviolet irradiation (1000-1200 rubles);
- laser - removal of moles with a beam (800-2000 rubles);
- radio wave, destruction of nevi by shock radio wave (RUB 700-1400)
The choice of method for removing moles is made by the doctor; prices for these procedures depend on the size and type of nevus.
Prevention of malignancy
Preventive methods for reducing the risk of malignancy of moles include:
- limited sunbathing, cancellation of visits to the solarium;
- minimizing skin trauma;
- maintaining a healthy lifestyle (healthy eating and avoiding bad habits).



