Increasingly in recent years, women have experienced problems with conception, pregnancy and childbirth. There are many reasons for this: inflammatory diseases, age, poor health, and so on. In most cases, modern medicine still helps the fairer sex overcome her illness. However, after some treatment methods, scars appear on the uterus. You will learn from the article how they arise and what they threaten. It is worth mentioning separately how a scar on the uterus can be dangerous during pregnancy.
What is a scar?
A scar is tissue damage that has subsequently been repaired. Most often, the surgical method of suturing is used for this. Less commonly, cut areas are glued together using special adhesives and so-called glue. In simple cases, with minor injuries, the rupture heals on its own, forming a scar.
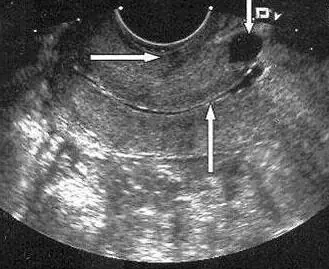
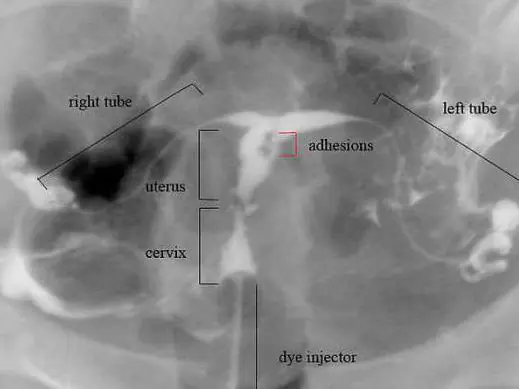
Such a formation can be located anywhere: on the human body or organs. For women, the scar on the uterus is of particular importance. A photo of this formation will be presented to you in the article. Damage can be diagnosed using ultrasound, palpation, and various types of tomography. Moreover, each method has its advantages. So, during an ultrasound, the doctor can assess the position of the scar, its size and thickness. Tomography helps to determine the relief of formation.

Reasons for appearance
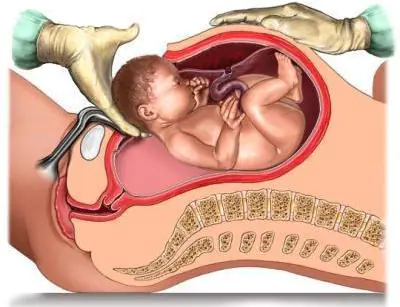
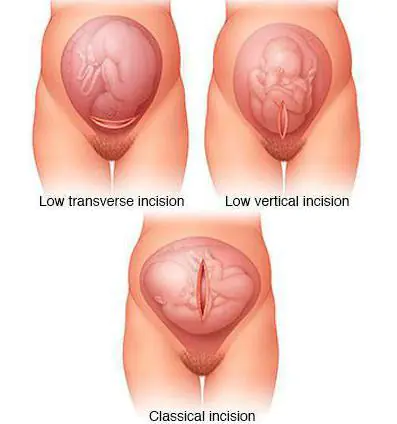
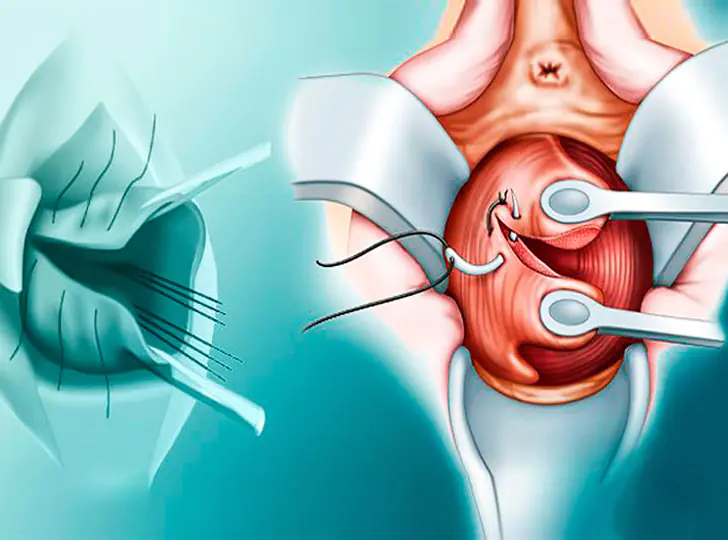
Why do some women develop scars on their uterus? Such damage becomes a consequence of medical interventions. This is usually a caesarean section. In this case, the type of operation plays an important role. It can be planned or emergency. During planned delivery, the uterus is incised in the lower segment of the abdominal cavity. After the fetus is removed, it is sutured layer-by-layer. This scar is called transverse. In an emergency caesarean section, a longitudinal incision is often made. In this case, the scar has the same name.
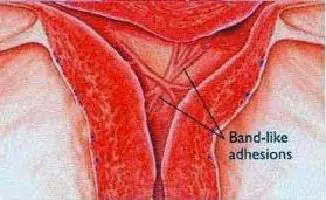
Fused lesions can result from perforation of the uterine wall during gynecological procedures: curettage, hysteroscopy, insertion of an IUD. Also, scars always remain after surgical removal of fibroids. In these cases, the position of the scar does not depend on specialists. It forms where the operation was performed.
Pregnancy and scar
If you have scars on your uterus, the possibility of having a baby depends on their condition. Before planning, you should definitely consult a gynecologist. The specialist will certainly conduct an ultrasound examination to determine the condition and position of the scar. You will also need to undergo some tests. Before planning begins, it is imperative to cure infections. Subsequently, they can cause problems with pregnancy.
If the scar is in the lower segment and has a transverse position, then problems usually do not arise. The fairer sex is examined and released to plan a pregnancy. In the case where the scar turns out to be insolvent, thinned and consisting mainly of connective tissue, pregnancy may be contraindicated. However, in some cases, the hands of surgeons work wonders. And a woman can still give birth.
Management of pregnancy and childbirth with a uterine scar
If you have a scar on the reproductive organ, then you need to inform the specialist who will manage your pregnancy about this. At the same time, you need to tell about the existing fact immediately, at the first visit, and not before the birth itself. Pregnancy management in women with a history of uterine injuries occurs somewhat differently. They get more attention. Also, this category of expectant mothers regularly have to visit an ultrasound diagnostic room. Such visits become especially frequent in the third trimester. Before childbirth, an ultrasound of the uterine scar is performed almost every two weeks. It is worth noting that other diagnostic methods are unacceptable during pregnancy. X-rays and tomography are contraindicated. The only exceptions are special, difficult situations when it comes not only to a woman’s health, but also to her life.
Delivery can be carried out by two methods: natural and operative. Most often, women themselves choose the second option. However, if the scar is intact and the expectant mother is in normal health, a natural birth is quite acceptable. To make the right choice, you need to consult with an experienced specialist. Also, during labor and increasing contractions, it is worth conducting periodic ultrasound monitoring of the condition of the scar and the uterus. Doctors also monitor the fetal heartbeat.
Damage to the cervix
As practice shows, some women who give birth on their own have a scar on the cervix. It occurs due to tissue rupture. During the process of childbirth, a woman feels painful contractions. Attempts begin behind them. If the cervix is not fully dilated at the moment, then they can lead to its rupture. This does not threaten anything for the child. However, the woman subsequently has a scar on her cervix. Of course, after delivery, all tissues are sutured. But in the future this may become a problem during the next birth.
Such a scar at the mouth of the cervical canal can also appear after other gynecological manipulations: cauterization of erosion, removal of a polyp, and so on. In all cases, the resulting scar appears to be connective tissue. During subsequent delivery, it simply does not stretch, leaving the area of the cervix undilated. Otherwise, the damage does not pose any danger to the mother and her unborn child. Let's try to find out why scars located on the reproductive organ can be dangerous.

Attachment of the fertilized egg and its growth
If there are scars on the uterus, then after fertilization a set of cells can attach to them. So, this happens in about two out of ten cases. At the same time, the forecasts turn out to be very dire. On the surface of the scar there is a mass of damaged vessels and capillaries. It is through them that the fertilized egg is nourished. Most often, such a pregnancy is terminated on its own during the first trimester. The consequence can be called not only unpleasant, but also dangerous. After all, a woman needs emergency medical care. Decaying fetal tissue can lead to sepsis.
Incorrect attachment of the placenta
A scar on the uterus after a cesarean section is dangerous because during the next pregnancy it can cause improper attachment of the baby's place. Often women are faced with the fact that the placenta is fixed close to the birth canal. Moreover, as pregnancy progresses, it migrates higher. The scar may prevent such movement.
The presence of a scar after damage to the reproductive organ often leads to placenta accreta. The baby's place is located precisely on the scar area. Doctors distinguish basal, muscular and complete placenta accreta. In the first case, the forecasts may be good. However, natural childbirth is no longer possible. If placenta accreta is complete, the uterus may need to be removed.
Fetal condition
A scar on the uterus can lead to poor circulation in the reproductive organ. At the same time, the unborn child does not receive enough oxygen and all the substances he needs. If such a pathology is detected in a timely manner, it can be treated and supported with appropriate medications. Otherwise, hypoxia occurs, which is fraught with intrauterine growth retardation. In particularly difficult situations, the child may remain disabled or even die.
Uterine growth
In a normal non-pregnant state, the thickness of the walls of the reproductive organ is about 3 centimeters. By the end of pregnancy they stretch up to 2 millimeters. At the same time, the scar also becomes thinner. As is known, fused damage is replaced by connective tissue. However, normally a large area of the scar is represented by a muscle layer. In this case, the scar is considered valid. If the damage thins down to 1 millimeter, this is not a very good sign. In most cases, experts prescribe bed rest and supportive medications to the expectant mother. Depending on the length of pregnancy and the thickness of the uterine scar, a decision may be made to deliver prematurely. This condition has dangerous consequences for the baby.
After childbirth…
Scarring on the uterus after childbirth can also be dangerous. Despite the fact that the baby has already been born, consequences may arise for his mother. Scars are damage to the mucous membrane. As you know, after childbirth, every woman experiences bleeding. The process of separation of mucus and remnants of membranes occurs. These secretions are called lochia. In some situations, mucus may linger on the scar area. This leads to an inflammatory process. The woman requires curettage, her body temperature rises, and her health worsens. In the absence of timely treatment, blood poisoning begins.
Aesthetic side
Often the presence of a scar on the uterus is a reason for a caesarean section. Many women are concerned about their subsequent appearance. An ugly scar remains on the stomach. However, much depends on the surgeon’s technique. Also, the possibilities of cosmetology do not stand still. If desired, you can do plastic surgery and hide the ugly seam.
Summarize
You learned about what a uterine scar is, in what situations it appears and why it is dangerous. Let us note that if you properly prepare for pregnancy and listen to the advice of an experienced doctor when managing it, then the outcome in most cases is good. The new mother and baby are discharged from the maternity ward in about a week. Don't be too upset if you have a uterine scar. Before you start planning, be sure to consult your doctor, undergo routine examinations, and take all tests. After this you can get pregnant.

Experts do not advise starting to plan a pregnancy earlier than two years after receiving such an injury. Also, don’t delay this. Doctors say that after 4-5 years it will be almost impossible to stretch the scar. This is when problems can begin during pregnancy and childbirth. All the best to you!
A cervical scar is a scar that appears at the site of a rupture during childbirth or during surgery. It is easier to get rid of a scar at an early stage of its occurrence - treatment is easier and faster, and the recovery process takes less time.
The classification of scars is divided depending on the type of tissue that was used to replace the damaged area. Experts distinguish two types:
- Wealthy scars are elastic areas that are characterized by the ability to narrow during contractions, resistance to stress and maintaining their normal shape in a normal state (do not stretch);
- Insolvent scars have completely the opposite characteristics: they are inelastic, there is no possibility of contraction during contractions, and they are susceptible to rupture under minor loads.
Important! The presence of an incompetent scar is dangerous for the female reproductive system - its presence can negatively affect the reproductive function of the body.
The definition of diagnosis depends on the location of its occurrence. The deformity may appear on the lower segment, body, cervix and area near the internal os of the uterus. The International Classification of Diseases, Tenth Revision (ICD-10), in turn, identifies the following conditions:
- scar on the uterus (code 034.2) - there is a connecting suture on the body, fundus, lateral surface or cervix, which either does not manifest itself at all or leads to the appearance of inflammatory processes, endometriosis. Occurs as a result of cesarean section, abortion, traumatic rupture, removal of benign tumors, and previous inflammatory diseases of the uterus.
- Obtained during a natural birth after a cesarean section (code 075.7) - the scar poses a danger during childbirth: tension in the muscle fibers of the uterus increases, and therefore it can subsequently rupture, bleeding and the fetus entering the abdominal cavity.
Pathology manifests itself depending on the cause of its occurrence. Clinical signs also depend on the location of the scar in the uterine cavity.
Symptoms
The scar on the cervix does not manifest itself in any way at first. There are no signs of pathology even with its congenital appearance. The late stage is characterized by the following symptoms:
- Pain during menstruation;
- Abundant, stretching, thick white discharge;
- Failure of the menstrual cycle;
- Discomfort, heaviness in the lower abdomen;
- Pain in the pelvis, radiating to the lower back;
- Pain during sexual intercourse.
You should consult a doctor the first time one of the above conditions occurs.
Causes
A scar on the cervix is a formation of connective cells. Appear in a woman under the following circumstances:
- after a difficult birth, during which the uterus ruptured;
- after caesarean section;
- after cauterization of erosion;
- after scraping;
- with artificial termination of pregnancy;
- Due to inflammatory processes, during the treatment of which the uterine tissue was damaged.
Important! In addition to occurring as a result of mechanical intervention, scars are inherited and can be a congenital pathology. In such a situation, symptoms most often do not appear, the scar does not bother you in any way, and its presence can only be determined at an appointment with a gynecologist.
Diagnosis and treatment depend on the period in which the scar was discovered: in normal conditions, general therapy is prescribed; during pregnancy, the doctor prescribes procedures based on the individual characteristics of the patient.
Complications and prognosis
Deformation of scar tissue leads to loss of the ability of epithelial cells to produce secretions. As a result, the formation of mucous membranes becomes more difficult, and the protection of internal organs is reduced. Against the background of all these processes, inflammatory diseases often develop:
- Atrophy of genital tissue;
- Endometritis and endocervicitis;
- Ectopia and erosion;
- Cervicitis.
The presence of scar tissue also leads to more serious consequences:
- Early birth;
- Constant bleeding;
- Amniotic fluid during pregnancy;
- Miscarriages;
- Infertility;
- Impossibility of spontaneous childbirth (caesarean section is prescribed).
Important! The prognosis for treatment is positive if pathology is detected at an early stage. An neglected diagnosis can result in the occurrence of cancers and malignant tumors, which, in turn, can cause removal of the uterus or lead to death.
Scar and pregnancy
A scar on the cervix during pregnancy puts tension on the genitals. Strong pressure leads to its rupture, which is dangerous with the following consequences:
- Internal bleeding;
- Stillbirth;
- Death of the mother (possible during natural childbirth, a caesarean section will help avoid this).
The presence of a scar does not affect the conception of a child in any way; it makes itself felt directly during childbirth. The ability to give birth to a baby without surgical intervention depends on the location of the scar: if the incision covers the opening of the cervix and was caused by a cesarean section, natural childbirth is prohibited; in other cases, the decision remains with the attending physician.
Diagnostics
The appearance of a scar at an early stage is not accompanied by symptoms, so its presence can only be determined at an appointment with a gynecologist. At the first signs of pathology, the doctor prescribes the following laboratory tests:
- Blood test for hormones;
- Analysis of vaginal secretions for microflora;
- Blood PCR.
Additional methods are prescribed when the deformity is not clearly expressed. The most common of them are:
- Colposcopy;
- Cytology;
- Hysterography;
- Hysteroscopy;
- Gynecological ultrasound.
The last three studies show the condition of the scar tissue. Based on the data obtained, the specialist prescribes appropriate treatment.
Treatment
Therapy is selected individually for each patient and depends on the following factors:
- Age;
- Presence of children (or absence thereof);
- Presence of concomitant diseases;
- General condition of the body.
Modern methods of treating scar deformity make it possible to remove pathology without blood. Experts divide these methods into two types:
The first implies direct removal of the scar. The following procedures are used for this:
- Cryodestruction is carried out using a cryoprobe (a special preparation) and liquid nitrogen. The scar disappears through a process of cooling and crystallization. Dead cell tissue is removed from the body within 2-3 months along with secretions.
- Radio wave destruction — the process takes place under local anesthesia (lidocaine, novocaine is administered) using the Surgitron apparatus. The device sends radiation at a certain frequency to the desired location, which eliminates scar tissue. The procedure lasts about 5 minutes; for the first time after its completion, dizziness and weakness may occur.
- Electrocoagulation - a drug for scar removal is selected depending on the nature of the defect. The procedure lasts from a few seconds to 10-15 minutes. After its completion, the area is lubricated with a potassium solution. The method is absolutely painless and removes formations without a trace.
- Vaporization is also called laser destruction or laser ablation. The laser affects only the scar, nearby tissues are not affected. The procedure is carried out from the 7th to the 16th day of the menstrual cycle phase. Tissue restoration and healing is quick and painless. You should completely abstain from sexual contact for a month.
- Reconstruction (surgical excision of scars) - used for severe deformation, depending on the severity of the scar.
The second type is the recovery of the body after surgical treatment. Experts prescribe medications based on the cause of the scar.
Important! Patients are not recommended to plan pregnancy for 6 months after therapy. Such caution will help avoid recurrence of the scar and complications.
Prevention
Cicatricial deformity of the cervix is a dangerous disease that is easier to prevent than to treat. To avoid the occurrence of pathology will help:
- Protection during sexual acts;
- Monitoring hormonal changes;
- Visiting a gynecologist (examination should be done twice a year);
- Regular sexual partner;
- Daily and high-quality hygiene of the intimate area.
Regular examination for predisposition to the occurrence of pathology should be carried out at least twice a year.
At the end of labor, many women are left with soft tissue ruptures. Surgical interventions also leave marks on the female reproductive system. A scar on the cervix indicates a rupture, incision, or other similar action. When the mother is not planning another conception, there is no danger.
What is a scar and the reasons for its appearance
The suture on the cervix is a connection of soft tissues that is formed at the sites of ruptures during the birth process and incisions during caesarean section. In other words, these are scars. Scars are benign formations made by the hands of a doctor. They do not cause any harm to the body. In everyday life, a woman does not experience discomfort. Negative consequences are felt only when planning a pregnancy. A mother who has undergone suturing of the cervix after childbirth is wary when deciding to conceive again.
Why scars appear:
- labor ending in torn tissue;
- C-section;
- cauterization of erosion;
- scraping;
- artificial termination of pregnancy;
- inflammation of internal organs.
A woman planning to conceive undergoes an examination. When a gynecologist notices the presence of a scar, he suggests a course of therapy or surgical removal of the scar. If the stitches are noticed later, already during the pregnancy, the doctor offers available options for treating scars on the cervix and methods of labor. Often the doctor advises cesarean section as the most successful method of solving the problem.
The danger of having sewn tissues is the possibility of their divergence during pregnancy. Rupture can lead to the loss of the child and the death of the mother. During pregnancy, there is a lot of pressure on the female reproductive system. The fabric has also lost its elasticity. She can't stand it, she breaks. Next, the flow of blood inside the body opens. The only salvation is an emergency caesarean section.
Cicatricial deformity of the cervix
The disorder is congenital, post-traumatic in nature. The symptoms are not pronounced. They manifest themselves as leucorrhoea, longer menstruation, and pain in the pelvic area. To make an accurate diagnosis, the gynecologist collects anamnesis, conducts a speculum examination, and sends the woman for laboratory tests.
The phenomenon often occurs in mothers who give birth for the first time after 30 years. The possibility of replacing healthy epithelium with scar tissue increases in individuals with cervicitis. If preventive measures and diagnosis are not carried out in a timely manner, the risk of developing infertility increases. Scar formation is encouraged by interventions during which the epithelium is injured.
Common reasons are:
- invasive procedures;
- pathological childbirth;
- errors during casting.
Sutures are made on the cervix after childbirth using obstetric forceps when the baby is large or incorrectly positioned. Also if the process went quickly and the disclosure was insufficient. Women over 30 are more likely to get damaged.
Abortions, endoscopic interventions, and therapeutic diagnostics are considered invasive procedures. The gynecologist inserts instruments through the cervical canal during surgery. The integrity of the epithelium is destroyed.
Errors may be made during suturing. Especially if the doctor is young and does not have enough experience. Cervical deformity in the form of a congenital scar is not common. In such cases, it is accompanied by a disease of a number of located organs.
Cicatricial deformity has 4 degrees. When dividing, the number, size, condition of the tissues and pharynx are taken into account.
At grade 1, the depth of the tears does not exceed 2 cm. The canal looks like a cone. The internal uterine os acts as the apex. The outer one opens to allow 1 finger of the gynecologist to pass through.
Grade 2 is characterized by a completely inverted endocervix. The neck of the reproductive organ is divided into the posterior and anterior lips. The ruptures extend to the beginning of the arches.
3rd degree. The external os is difficult to recognize. One of the lips is hypertrophied. The ruptures reach the vagina. Symptoms of inflammation are noticed.
4th degree. Dysfunction of the muscular parts of the pelvic floor. The discrepancies extend to the vagina. Epithelial dysplasia.
When the scar is deformed, the woman is bothered by discomfort in the lower abdomen. Copious mucous discharge appears. 15% of people report pain during intimacy.
Stitches on the cervix before labor
Sometimes carrying a child is at risk of miscarriage. Various diseases cause cervical insufficiency. To save the situation, the gynecologist suggests putting stitches on the cervix. The procedure is considered forced. It allows you to prolong pregnancy. After conception has occurred, the cervix becomes completely clogged.
In addition to holding the child, the suturing procedure faces the task of preventing the penetration of bacteria. Pathogenic microbes, getting inside, can infect the baby. Without the necessary protection, there is a risk of losing the baby before birth.
Indications for suturing are:
- threat of miscarriage, labor ahead of schedule;
- early cervical dilatation;
- the edges were sloppily sewn together, leaving questionable scars;
- destructive changes of any nature.
The gynecologist does not make a decision based only on an examination; he must obtain complete information about the cervix. Therefore, a biometric study is carried out, consisting of ultrasound diagnostics, colposcopy, and smear examination. Suturing is carried out if no problems are found other than organ weakness.
The manipulation is done at 14–21 weeks, when the baby is small. The walls and muscles are very stretched in the late period. They will not tolerate stitching and divergence will occur.
What does a scar on the cervix look like:
- tissue is collected through the entire thickness of the myometrium;
- Only part of the muscle layer is captured.
The operation is performed in a hospital and requires preparation. To make the procedure painless, epidural anesthesia is administered. The intervention lasts 15 minutes. One pharynx is sewn in. The technique is quite simple: the edges of the fabric are pulled together with strong surgical threads.
Suture treatment
Any lump in the scar is considered abnormal. Often the cause is the accumulation of lymphoid fluid. When microbes enter, inflammation develops. To prevent such phenomena from happening, you must follow the instructions of the gynecologist.
How long does it take for stitches on the cervix to heal after childbirth? Soreness and discomfort continue for 3–4 days. If natural suture threads were used, the duration of scarring is 13–15 days. Resorption will occur in a month. The synthetic material is removed after 6–7 days. It takes 3 – 5 weeks to heal.
How long the cervix takes to heal depends on the female body’s ability to regenerate and high-quality surface treatment. The recovery time increases if the wound becomes infected. A guarantee of quick scarring is proper care.
If tissue hyperplasia occurs during the healing stage, a granulation scar is formed on the cervical stump. The growths are typical for women with tears after a difficult birth. At first, significant discomfort is felt. Cases when granulation grows are dangerous. Blood may be released from the formation.
When thickening, coarsening, or increased keratinization occurs, a biopsy is performed. Indications for it are also changes in the mucous membrane, local growths. After a biopsy of the cervix, the nature of the formations is determined. Poor quality can be treated in the initial stages of detection.
How to remove cervical sutures before childbirth:
- An ultrasound is performed to determine the baby’s readiness for birth;
- the mother is examined and admitted to the hospital;
- the threads are removed.
The procedure is carried out at 37–38 weeks. It's always planned. It is unsafe to carry out any actions before.
Removing stitches from the cervix before childbirth can cause bleeding. Sometimes, after manipulation there is slight discharge. These processes are not considered an anomaly. The tone of the uterus increases from aggressive contact with instruments. To stop it, the gynecologist prescribes antispasmodic drugs.
Do not lift heavy objects after removing the suture from the cervix. Any stress or intimate relationships are prohibited. Swimming in a bathtub or pond is not advisable. For the first 24 hours, the nursing staff looks after the woman in labor.
Labor usually begins after 2 weeks after the stitches are removed from the cervix. The indicator is considered average. However, practice says that the baby can be born after 3 hours.
Norms and diagnostics of a suture on the uterus for natural childbirth
A scar appears after surgery. It is carried out for medical reasons. The degree of healing is of great importance. To plan subsequent conception, it is necessary to assess the condition of the postoperative scar on the uterus. Ultrasound examination is considered a reliable method. The procedure is carried out in the first weeks of pregnancy. During the manipulation, the width and length are measured, and possible defects are identified.
The thickness of the scar on the uterus during pregnancy is normally 6 - 7 mm or more. You can confirm the result using a vaginal sensor. The condition of the suture is assessed before and after conception.
The first option allows you to see deviations. The doctor pays attention to the structure and compaction of the wall where the stitching was performed. A scar thickness on the uterus of 1 mm indicates incompetence and is a bad signal.
An insolvent scar is noted when:
- thickness less than 3 mm;
- niches and unevenness are detected;
- discontinuity of the outer contour.
The stitching material also plays a role. Catgut often leads to the development of incompetent postoperative scar on the uterus. When using vicryl, tissues, on the contrary, heal well.
A seam is considered satisfactory if it has the following indicators:
- thickness 4 – 5 mm;
- a clear layer of myometrium along the entire length;
- no thinning areas.
How many mm should the uterine scar be for childbirth? Normally it is 5 mm. During pregnancy it becomes thinner. Therefore, at the end of gestation, even 2 - 3 mm is considered an acceptable parameter for the thickness of the uterine scar for natural childbirth.
The birth of a baby naturally is allowed when there is only 1 full scar. Cardiac monitoring is carried out throughout the entire process. Sensors are connected to the woman in labor. One reacts to the activity of contractions, the second records the baby’s heart rate. When the myometrium in the area of the uterine scar is normal, labor will proceed without complications or consequences. If a rupture or its threat occurs during the birth of a baby, surgical assistance should be provided in the next few minutes.
The normal thickness of the uterine scar by week is relative. Each woman in labor has her own parameters, according to the individual structural characteristics of the body. One of them has a scar of 11-15 mm on the uterus at week 12. The second one has a scar on the uterus at 17 - 8 - 9 mm. In the third, the 23rd week is marked by a 1.5 mm scar on the uterus.
If a thinning scar on the uterus is suspected, a woman in labor is admitted to the hospital at 34–35 weeks of gestation. Childbirth is carried out using the surgical method. Only the deadlines need to be determined.
Before the birth process and on time, constant monitoring of the condition of the seam is carried out. The normal indicator for the length of the uterine scar is 15 cm. The doctor palpates the stitched area. It should be smooth, with clear boundaries, despite the contractions. There is practically no pain. For an objective assessment, an ultrasound scan of the uterine scar is performed. The ratio of muscle and connective tissue is determined on MRI. Vomiting, nausea, weakening contractions are considered signs of the onset of a rupture. The obstetrician proceeds to delivery by cesarean section.
Causes of a suture on the uterus during childbirth
Damage to the organ can occur before the baby is born, during and after. Active early attempts when the cervix is not open enough lead to injury. Sluggish contractions are stimulated by special drugs, which also negatively affects integrity. If, after the natural process of giving birth to a child, the reproductive organ gradually returns to its original parameters, then at the end of the cesarean section, when the uterus is sewn up after childbirth, a mark in the form of a scar remains forever. The size of the scar during the second pregnancy will have to be kept under constant control.
- a consequence of perforation of the wall during abortion;
- the result of tube removal during ectopic pregnancy;
- C-section;
- cutting out fibroids;
- elimination of the intrauterine septum.
After giving birth to a child through surgery, you need to rest for 2 to 3 years. Only then is the next pregnancy allowed. Some people have three scars on the uterus, as a result of labor being performed surgically each time. To avoid the undesirable consequence of suture dehiscence, you need to rest for at least 2 years between births.
When planning to conceive, you should undergo an ultrasound. The gynecologist will check the normal thickness of the uterine scar in width and length. If there are no deviations, he will allow you to give birth to the baby. A well-healed suture will not manifest itself in any way during the next pregnancy.
How many mm should a wealthy uterine scar be? Stitching is complete if the fibers of the muscle sections are completely restored. The fabric is elastic, capable of shrinking and stretching. The normal size of a uterine scar is 2.5 mm at its narrowest extent. When it consists of connected sections, it belongs to the class of inferior.
How thin can a uterine scar become? The process is uncontrolled, not subject to treatment, and goes away gradually during pregnancy. The type of cut matters: longitudinal or transverse. The first one is more prone to failure; it is done in an emergency.
Treatment of a suture on the reproductive organ
If bearing a child and childbirth passed without consequences, the uterine scar does not require special therapy. When a thin scar on the uterus was observed during pregnancy, the obstetrician recommends abandoning the next conception to avoid complications. The normal thickness of the uterine scar at 38 weeks is 5 mm.
All injuries at the end of the birth process require mandatory treatment. It begins after the placenta is delivered. Minor stitching does not require anesthesia. When deep ruptures are detected, the woman in labor is given general anesthesia and the cavity of the reproductive organ is examined, studying the rupture. If epidural analgesia was used during labor, an analgesic is added to the already installed catheter.
Stitched areas after cesarean section cause discomfort for 2 – 3 weeks. In the first days, the woman in labor takes painkillers. The obstetrician does not recommend lying down. Moderate activity promotes contraction of the reproductive organ, healing occurs faster. If the scar itches, you just need to endure it.
A feeling of heaviness in the perineum after childbirth indicates the formation of a hematoma. It usually manifests itself in the hospital. Therefore, it is necessary to immediately inform the obstetrician. Dehiscence of sutures can occur in the hospital if the woman in labor does not follow the prescribed instructions: she begins to sit up early and moves abruptly. In such cases, re-suturing is done. The wound is treated with antiseptics.
A seal on the seam after childbirth indicates the need to visit a gynecologist. Often the thread of a self-absorbing suture is mistaken for a lump, then there is no need to worry. But the formation of an abscess signals continuous infection of the wound, perhaps the threads are rejected by the body.
Calcifications found on ultrasound in the area of the uterine scar are not a disease. They are detected when calcium salts are deposited in any part of the uterus, fibromatous node. The cause of formation is considered to be previous inflammation. Located in the muscular layer of the reproductive organ, they do not cause concern.
If the scar on the uterus itches at 38 weeks, this is a signal of a likely increase in temperature. An infection could have entered the body. The symptom cannot be ignored. At this stage, premature labor is caused; all the child’s systems are already developed and ready for independent functioning.
Is it possible to give birth with a thin uterine wall? In the early stages of pregnancy, the situation requires special monitoring by a gynecologist. Mandatory therapy is prescribed to prevent miscarriage from occurring at any moment. The IVF procedure for this pathology is undesirable. The chances of the embryo implanting in the uterus are very low.
A scar on the cervix and the reproductive organ itself occurs in many women after labor. It is not a tumor or pathogenic formation. But if you get pregnant again, it can cause some problems. The epithelium of healed tissue can rupture for a number of reasons and cause bleeding.



