Don’t rush to give up sandals: rough skin on your heels is a solvable problem. You will learn everything you need to do to put it in order from this article.
- Why does the skin on the heels become rough?
- How to get rid of rough skin on your heels
- How to remove rough skin at home
- Daily care rules
- Useful tips and tricks
Why does the skin on the heels become rough?
If you have rough skin on your heels, don't throw away your open-toed sandals. Yes, from an aesthetic point of view, the heels are not in the best shape now, but the problem can be solved quite easily. In addition, nature has provided for everything: there are practically no sebaceous glands on the skin of the sole, because this area does not need tenderness and smoothness.
Feet are what we stand on, our fulcrum. So thickening and roughening of the skin in this area is a natural functional reaction.
However, this does not mean that we should give up. Modern girls take care of every part of their body almost as actively as they take care of their face. And they do it right. You need to get rid of rough skin on your heels.
“In places of maximum pressure, the skin thickens, becomes denser, and blood circulation is impaired. And if the skin is not taken care of regularly, scabs and painful cracks can form.”
External and internal reasons
Hyperkeratosis (excessive thickening of the skin) of the feet can be caused by the following reasons:
excess body weight;
uncomfortable shoes, for example, rubber sneakers;
flat feet and improper weight distribution;
hormonal changes (for example, during menopause);
improper care or lack thereof.
How to get rid of rough skin on your heels
Cosmetology procedures
A pedicure in the salon is aimed, among other things, at exfoliating corns, as well as nourishing and restoring the skin of the feet. The heels are polished with files with abrasive attachments, and the overgrown layers of skin are removed using special blades or a cutter (during a hardware pedicure). After the procedure, the heels are generously treated with moisturizing cream. During a spa manicure, you can apply a nourishing mask and put special socks on your feet.
Cosmetical tools
At home, creams that contain moisturizing and exfoliating ingredients can ensure the smoothness of your heels.
Urea renews and moisturizes the skin.
Acids promote exfoliation.
Oils and vitamin E protect from drying out and restore.
Panthenol and allantoin promote recovery.
Foot baths
A useful procedure during which the skin is steamed, after which it is easier to remove it using abrasives.
Foot masks
Nutritious
For home remedies, we recommend natural oils, and solid ones:
After steaming and exfoliating, the oil is rubbed into the heels, then applied as an additional layer, and cotton socks are put on top. This mask can be done every evening before bed, after a shower. Fatty acids help restore and soften the skin. In addition, this mask has only one ingredient, and therefore the recipe is simple and not time-consuming.
You can flavor the mask with a drop of olive, avocado or jojoba oil. In the morning your heels will be like those of that same baby.
Exfoliating and moisturizing
Grind two cucumbers in a blender, mix with lemon juice and three tablespoons of olive oil. Divide the resulting composition into two parts, put each in a separate plastic bag and put these improvised “boots” on your feet, securing them with laces around the ankle. Rinse off with cool water after 10-15 minutes.
How to remove rough skin at home
Preparation
Cleansing. Wash your feet thoroughly, e.g. shower gel “Grapefruit” Bath and Shower Liquid Body Cleanser, Kiehl’s. It smells nice and gently removes dirt.
Steam bath. Fill a large container with warm water and add a couple of tablespoons of baking soda or Epsom salts to soften the skin on your heels. Immerse your feet in the bath for 15–20 minutes. You can add fragrant salt with essential oils or bath gel to the solution.
Get wet feet with a towel.
Exfoliation
This is the main part of the program - removing the layer of dead cells that make the heels rough and rough. There are several ways to cope with this task.
Scrub - a good option for weekly care, it works quite gently and does not injure the skin, but dealing with serious growths will require patience and several procedures. Try it body scrub “Precious Beauty Scrub”, Garnier with argan tree seed shell powder, which exfoliates the skin, and softening oils of almond, rose, macadamia and the same argan.
Pumice - a hardened volcanic mass - has long proven its effectiveness.
File - a special device with a rough surface - acts as a mechanical abrasive.
Final stage
Rinse your feet again to remove any flakes of exfoliated skin.
Apply cream or oil.
Any body cream or lipid-replenishing milk is suitable for foot care. But it is still better to use special products designed taking into account the characteristics of the skin of the heels.
Care for dry and rough skin Intensive Treatment and Moisturizer for Dry or Callused Areas, Kiehl’s based on a nourishing oil composition (avocado, shea butter, wheat germ) is aimed at restoring the skin of the heels.
Daily care rules
1. Cleansing and exfoliation
Water and cleanser are not only the basis of basic hygiene, but also the prevention of corns. And regular scrubbing will help you keep your heels soft and smooth. Any body scrub will do. You can make it homemade by mixing olive oil or sour cream with granules of sugar or sea salt. If you don’t want to strain yourself, use the ready-made formula. 2-in-1 soap interspersed with abrasives is very convenient to use.
Coriander Gently Exfoliating Body Scrub Soap, Kiehl’s Contains jojoba seed powder and glycerin, cleanses and exfoliates very thoroughly, but gently.
2. Moisturizing and nutrition
When it comes to foot care, the key to success is consistency. Foot baths and thorough exfoliation should be weekly (2-3 times a week) or course, but the cream should be applied every evening. Choose a product at your own discretion, the main thing is not to ignore care, your heels “overgrow” very quickly. Our recommendations:
Foot cream “Intensive care. Food", Garnier - An excellent remedy against dryness and cracks. Contains allantoin, which has a softening effect.
Useful tips and tricks
Reduce stress on your feet. No, we are not calling for a diet, but it is recommended to take care of comfortable shoes that fit the size, season and circumstances.
Drink more water to keep your skin hydrated.
If you like to walk around the house barefoot, do so in cotton socks - they will serve as a protective barrier.
Do not wear synthetic socks, which interfere with normal thermoregulation.
Do not use professional pedicure razors at home. Is it dangerous.
Give your feet a weekly spa session and moisturize them every night.
A growth on the heel can appear for various reasons in a person at any age. There are several varieties of it. Some make themselves felt immediately, others grow gradually and then cause significant discomfort. It is important to know what to do when such pathologies appear, which doctor to contact for qualified help.
Types of growths
There are many types of formations that can appear in the designated area.
Most often diagnosed:
- heel spur;
- Haglund's deformity;
- soft buds;
- leathery calluses.
Each pathology has its own clinical manifestations, but they have approximately the same trigger mechanisms.
Causes of growths
The main reason for the appearance of growths on the heel bone, soft bumps and leathery calluses is high load, leading to injury. Excess weight, frequent long walking, tight shoes, high heels, improper lifting - all this contributes to slow blood flow and impaired nutrition of the joints. As a result, the development of pathological processes that can lead a person to disability. They definitely need to be treated. But therapy without eliminating the main provoking factor demonstrates only a temporary effect.
Heel spur
A disease that causes an enlargement of the heel bone towards the sole. A similar defect is detected today in 10% of all bone pathologies. Most often it forms in women after forty years.
- patients with diabetes mellitus;
- obese people;
- patients with a history of pathologies, the development of which impairs blood circulation in the body;
- athletes who constantly injure their legs in the foot area;
- women who often wear very high heels;
- children with longitudinal flat feet;
- patients with a history of spinal diseases, rheumatoid arthritis, gout, osteoarthritis.

After fifty years, the fat pad in the heel often decreases. And this also leads to the appearance of heel spurs.
Symptoms and signs
In its development, the disease goes through several stages.
- At the first stage, a person experiences sharp pain when walking or running, which intensifies when resting on the heel. They appear in the form of lumbago, forcing a person to stop and raise his legs.
- At the second stage, the first pain subsides. They begin to appear in the morning, when a person tries to make the first movements after sleep, then decrease, and intensify in the evening.
- The third stage is diagnosed when the condition worsens, attacks of pain also occur during moments of rest. Trying to get rid of them, the patient unconsciously begins to limp.

If spurs grow on both heels at once, walking becomes possible only with the use of crutches.
Diagnostics
The disease is determined based on the patient's complaints. Painful shooting is the main diagnostic criterion, allowing identification of pathology in 90%. To confirm suspicions, during the examination the surgeon tries to press firmly on the middle of the patient’s heel and on the lateral area. Increased pain suggests that the assumptions are correct. Afterwards, the doctor assesses the mobility of the foot and determines the stage of the disease.
To carry out treatment, you need to know what size the heel spur is. X-rays help identify them. The pictures also show the exact location of the defect. If the thorn has a round shape, the first stage of the pathology is diagnosed; in advanced stages, the growth takes the shape of a bird's claw.
Sometimes the doctor may write a referral for an MRI. This examination allows you to assess the condition of the surrounding tissues. Ultrasound is often used in the treatment process. It is used to evaluate the results of therapy.
Sometimes it is necessary to differentiate a heel spur from a spine. A spur forms only on the heel bone and, as it grows, cuts through soft tissue. The spine can grow on both the palm and the foot. The pathology starts with infection with the human papillomavirus. Externally, the spine looks like a small nodule. This is not a bone formation.
Treatment
Heel spurs that grow on the side or back can be treated in a variety of ways. To relieve pain and improve metabolic processes in the initial stages, creams and ointments ("Medical Bile", "Dimexide") are used; in advanced forms, Novocaine injections are given directly into the heel twice a day. To reduce the level of calcifications and relieve inflammation, the patient is prescribed injections of Flosteron, Kenalog or Diprospan.

The following help enhance the effect of drug therapy:
- therapeutic baths (with mud, paraffin; with minerals);
- electrophoresis;
- magnetic therapy;
- massotherapy.
During treatment, the patient must wear an orthosis on his leg at night - a special device that helps fix the foot at a right angle. This position helps to reduce the load as much as possible and prevent the development of inflammatory processes.
If such treatment does not help, the doctor decides to use:
- laser therapy;
- shock wave procedure;
- electrophoresis;
- UHF.
Laser therapy does not remove the spur itself, but relieves swelling, reduces inflammation, and eliminates pain. The first course consists of ten procedures, they are carried out daily. Then a two-week rest, and treatment resumes again. Experts note that laser therapy enhances the effect of the medications used, speeds up the process of drug treatment, and speeds up recovery. She has absolutely no side effects, the procedures do not cause allergies. But laser therapy has a whole list of contraindications. It is prohibited to use if the patient has tumors of unknown etiology, problems with the heart, respiratory system, or hematopoietic organs. Patients with diabetes should not take this treatment.
During shock wave procedures, the heel spur is impacted by a low-frequency sound wave. It helps improve blood circulation, relieve swelling, pain, restore the structure of damaged tendons, and destroy cacinata.

Electrophoresis and UHF therapy also have similar effects. Therefore, the choice of the method of influence is made taking into account the technical capabilities of the institution in which heel spurs are treated and the patient’s finances.
In particularly severe cases, when it becomes clear that it is not possible to get rid of a heel spur using conservative methods, surgical treatment is prescribed. Today it is performed using endoscopic removal or mini-invasive surgery, which is performed under X-ray control.
When choosing the first design option, two small incisions are made in the heel area. A camera is inserted into one hole and an endoscopic instrument into the other. The surgeon cuts off the bone process while watching his manipulations on the monitor. Since the spur on the heel is a bone growth, it can only be removed using a microscopic cutter. The operation is performed under local anesthesia. The recovery period lasts two weeks.
Mini-invasive surgery involves making one incision (3 mm). The surgeon monitors his manipulations using x-rays. This method of surgical intervention is associated with minimal postoperative complications and has an even shorter recovery period. To avoid the development of embolism, thrombosis and infection, the patient must take a course of antibiotics during the recovery period.
Haglund deformity
With the development of this pathology, a bone growth grows on the back of the heel bone, above the place where the Achilles tendon attaches. It presses on the designated anatomical node. As a result, inflammation develops inside it. It causes the appearance of a “heel bubble” in the place where the heel of the shoe is adjacent to the foot. Upon palpation, the described area becomes soft. But gradually a bone growth forms.
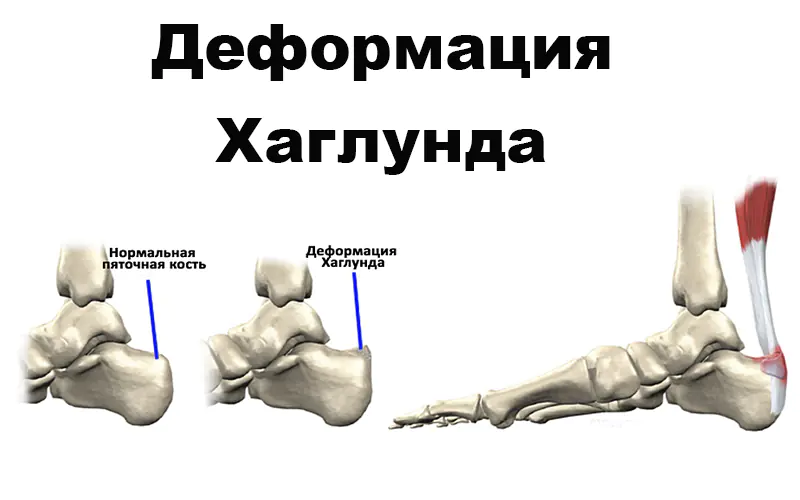
Scientists cannot yet explain the causes of Haglund's deformity. They suggest that heredity plays a large role. It has been noticed that among the patients there are many who have flat feet, in which the foot rolls inward. In this position, the tendon does not fit correctly onto the heel bone and is constantly injured during plantar flexion. Haglund's deformity also develops when the longitudinal arch of the foot is too high. Pathology forms on one or two legs at once. It is diagnosed using radiography.
Treatment
When drawing up a therapeutic regimen, the development of the clinical picture is taken into account. Sometimes the inflammation of the tendon bursa is mild, then a hard growth appears on the bone. You can only get rid of it through surgery. During this procedure, the bone growth is removed, the inflamed bursa is excised, and cysts developing inside the Achilles tendon are removed.
If inflammation of the bursa is predominant during the development of the clinical picture, the disease is treated conservatively.
- take anti-inflammatory drugs in tablet form;
- apply cold to the sore spot (ice wrapped in a towel);
- perform therapeutic exercises;
- reduce pressure on the heels of shoes and boots using a silicone patch;
- choose shoes with soft backs.
The use of an orthosis is considered useful - a special device that helps fix the position of the foot at an angle of 90 degrees and completely eliminate movement in the affected joint. Lack of load enhances the effect of drug therapy.
soft buds
The appearance of soft bumps on the heel of the feet is a common occurrence. Many of us do not attach importance to them, mistaking such changes for a cosmetic defect. A person turns to specialists for help only when the soft lumps begin to rapidly increase in size and become unbearably painful.

There are many reasons for the appearance of lumps on the feet.
Among them, the most common are:
- injuries in which the foot is bruised;
- inflammation of the lymph nodes;
- past infectious diseases;
- formation of a benign or malignant tumor;
- formation of fatty tissue;
- load caused by excess weight;
- allergic reaction;
- skin cysts.
It is difficult to give a general description of the soft bumps that form on the feet. The development of the clinical picture depends on what caused their appearance. If a pathology is detected, you must immediately consult a doctor and together with him identify the provoking factor. The effectiveness of treatment will depend on how accurately it is determined.
The therapeutic regimen consists of several positions:
- First of all, etiotropic therapy is carried out to eliminate the causes of the pathology.
- In parallel with this, local treatment of the affected areas is carried out.
- The patient is recommended to pay more attention to foot hygiene, to eliminate friction that occurs while wearing clothing and shoes.
Hemangiomas, lipomas, follicles, cysts, warts are subject to surgical removal.

Leather callus
Doctors call such formations “garbage heaps.” They accumulate dead dermal cells that have suffered from excessive pressure on them. In the early stages of development, such a pathology is only a cosmetic defect, in the later stages it is a serious illness that can provoke dangerous complications.
There are two types of calluses: leathery and bone. The first ones arise due to friction of shoes against the skin, the formation of excessive pressure on the feet. The latter are the result of bones that have not healed properly after fractures.
Leathery calluses, in turn, are divided into:
- Wet (soft). They are highly painful and can spontaneously rupture and become infected. If such a complication does not occur, over time the soft callus hardens and becomes horny.
- Dry (hard). They are not as painful as wet ones. The surface is covered with a thick horny layer.
- Corns. These are types of dry calluses. They are formed exclusively on the soles of the feet and are large in size. The reason for their appearance is incorrectly selected shoes.
- Rod. This is a type of dry callus, inside of which a growth has formed. It appears in the later stages of development. A hole first appears in the center, the walls of which harden over time. You cannot treat such a formation on your own.

Many people ignore the appearance of calluses, and only when they begin to hurt severely do they begin to look for a remedy that would help restore health to their feet. The use of incorrectly selected products often leads to skin infection. The “older” the growth, the more difficult it will be to get rid of the inflammation.
Old corns can deform the foot and provoke the development of flat feet. The appearance of skin calluses is considered especially dangerous in people suffering from diabetes. They develop more difficultly and become more easily infected.
Treatment
The disease is diagnosed based on an initial examination. To draw up a therapeutic regimen, the doctor must determine exactly what type of calluses have formed and what degree of neglect they have.
Wet calluses must be opened. To do this, the doctor first disinfects the affected area, picks up a sterile needle from a disposable syringe, and sticks it into the body of the callus where the skin has separated from the tissue. Then it allows the liquid to drain out on its own. This process cannot be pressed or accelerated. The surface of the fallen formation is re-treated with an antiseptic.
Fallen skin cannot be trimmed. You can lightly press it with a tampon. When it dries, it will turn into a lid that will reliably protect the wound from the penetration of pathogenic bacteria. Immediately after the puncture, a sterile bandage is applied over the sore area. You shouldn’t keep it on your leg for a long time: in order for the wound to heal quickly, the skin needs to be provided with air access. Therefore, it is better to remove the bandage while sleeping. When changing the dressing, a strong burning sensation appears in the area of the blister. You can remove it by applying a tampon soaked in cold milk to the wound for a few minutes.
Dry calluses are more difficult to deal with. The main emphasis during treatment is on their mitigation.
For these purposes, it is important to reproduce the following algorithm of actions daily:
- First, the feet are steamed in a bath (it is useful to add a few drops of tea tree oil or calendula tincture to the water first).
- When the stratum corneum of the steamed callus becomes soft, it needs to be cleaned with pumice.
- Afterwards, the feet are thoroughly dried with a soft towel, and any moisturizing cream is applied on top of the dry callus in a thick layer. Experts advise adding vitamin E to it before use (it is sold in pharmacies in ampoules). If you don’t have cream on hand, you can replace it with traditional medicine. An ointment prepared from an equal amount of melted lard and celandine juice helps a lot.
- At the final stage, you need to put woolen socks on your feet (heat will enhance the therapeutic effect of the products used).
Corns are also treated in a similar way. There are small adjustments that are useful to consider when conducting therapy at home. To steam your feet in water, in addition to tea tree oil, experts recommend adding apple cider vinegar. You can relieve pain with cold baths in which rock salt has been previously dissolved (a tablespoon per liter of water). At night, instead of moisturizing cream, it is better to use compresses with gruel made from grated onions.
Calluses with a core cannot be treated on your own. Only etching with aggressive acid will help get rid of it. This procedure is painful and must be performed with extreme caution. This should be done by an experienced doctor.
Aspirin tablets will help soften corns. Five pieces are ground into powder, a spoonful of lemon juice and water is added to it. The pulp is applied to the surface of the corns. The legs are covered with cellophane on top, and then wrapped in a warm towel. The application is removed after fifteen minutes, the hard skin is treated with pumice, and then any moisturizer is applied to it.
Pharmacy products
Pharmacies sell special medications that can replace traditional medicine and speed up recovery. What should you pay attention to?
- Corn patch. It is effective against fresh dry formations. During application, it is simply applied to the surface of the skin defect, left for several hours, and then peeled off. The top dry crust should come off along with it.
- Callus solution. It has a pronounced softening effect. During application, it is necessary to pipette the surface of the stratum corneum. As practice shows, it goes away in just a few doses of the drug.
- Salicylic ointment. It contains acid, which is found in callus fluid. The “working” layer of the plaster is impregnated with it.

It is necessary to use the products with extreme caution: when treating calluses, try not to touch adjacent healthy tissue.
Calluses can only be treated surgically. Radical therapy methods are used only if the formation causes severe pain.
Prevention
Knowing why the defects described above form on the heel, it is easy to understand what needs to be done to prevent their occurrence. First of all, it is useful to be careful when choosing shoes.
- Buy only what fits your foot (there should be a small free space between the toe of the shoe and the big toe).
- Wear shoes with soft backs more often.
- When wearing a pair, there should be no excessive pressure in the instep and sides.
- If you have to walk in high heels for a long time, you need to put a sponge pad in the sock.
- It is helpful to take off your shoes several times throughout the day and give your feet some rest.
- Carefully monitor foot hygiene; if there is excessive sweating, use special gels and sprays to reduce the intensity of sweat production.
- Eat a balanced diet.
- Give up bad habits.
It is also important to control your weight and monitor your immunity.
The appearance of a heel callus or growth causes a lot of unpleasant sensations to its owner. At the initial stages of development it is easily eliminated. At the same time, when the form is advanced, it often leads to various complications.
Causes of formations on the back of the foot

The appearance of calluses can be considered as a protective reaction of the body to increased load on the feet in the form of friction or pressure. Middle-aged and elderly people are most often affected. Possible reasons for the formation of growths on the heel:
- Wearing tight or new shoes. If shoes are not the right size, they will rub and lead to calluses.
- Great physical stress on the feet.
- Long walks.
- Frequent traumatization.
- Poor foot hygiene.
- Decreased elasticity of the Achilles tendon.
- Foot deformity or deviation of the heel bone.
In advanced cases, it is often impossible to do without the qualified assistance of a medical specialist.
Skin callus in the form of a lump
If your heels constantly rub against your shoes, you are guaranteed to develop a callus in the form of a bump. It is nothing more than hard, rough skin. There may be a combination of calluses appearing on the back and side of the foot. There are several types:
- Wet or watery. In appearance it resembles a convex bubble filled with transparent tissue fluid. After the blister ruptures, it leaves an open wound that can become infected.
- Dry. Develops at the site of a wet callus. Due to continued friction and pressure on the heel, the skin will become thick and rough.
- Rod. It looks like a plug inserted into the skin. If you press on it, it causes pain, but does not bleed.
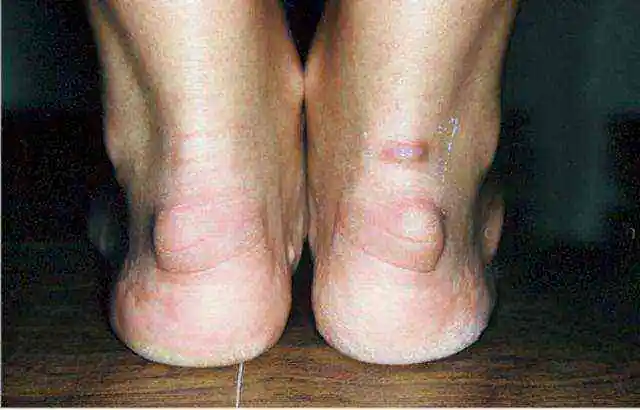
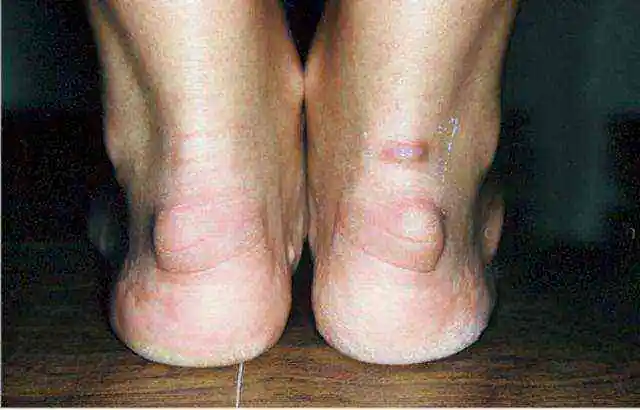
Haglund deformity
Calluses on the heel are not as bad as Haglund's deformity, which is characterized by the appearance of a bone growth (exostosis or osteophyte) on the heel bone. The pathology is named after the author who first described this disease. Haglund's deformity is a common cause of heel pain.
In some cases, there may be no pain or inflammatory symptoms of the disease. Only pathological growth is observed at the back of the heel. The functionality of the foot, as a rule, does not suffer. However, the vast majority of patients experience an inflammatory process in the joint capsule and Achilles tendon. The patient will experience quite severe pain while walking. Sometimes pain is present even at rest. It is pain that is the reason for going to the doctor. The deformity can occur on one or both feet.
Typical clinical manifestations characteristic of Haglund's disease:
- There is a bump on the back of the heel.
- I am concerned about pain at the insertion site of the Achilles tendon.
- In the area of the callus on the back surface of the heel bone, swelling is detected.
Folk remedies cannot always cope with growths on the heel. For Haglund's deformity they are not effective at all.
Treatment

For wet or watery calluses, the bladder is punctured to allow tissue fluid to drain out. The skin over the blister is not cut off; it covers the wound and protects against infection. The heel is treated with an antiseptic solution (for example, Chlorhexidine), a bactericidal patch is applied, or a bandage with ointment is applied.
With dry calluses, there is rough, thick skin that needs to be removed. First, steam the foot well, then use a pumice stone or a special pedicure grater to remove the rough skin. After the procedure, you can lubricate the surface of the heel with vegetable or olive oil. If it was not possible to eliminate the skin growth in one go, you can repeat the procedure.
The use of Anti-callus ointment, the active ingredients of which are lactic and salicylic acids, is considered effective. This is a classic keratolytic agent that helps remove the layer of keratinized epidermis. When used correctly, it successfully eliminates dry calluses. The ointment is applied to the callus once a day, then waxed paper is placed, which is secured with a plaster or bandage. The external remedy should be used until the callus softens for several days, so that it can be easily removed using a pumice stone or a pedicure grater.
In the initial stages of development of Haglund's deformity (a bone growth on the heel bone), it is possible to use conservative therapy, which is aimed at eliminating pain and inflammation. Some useful tips:
If wounds often appear in the area of the callus due to rubbing with shoes, this can lead to infection and the development of suppuration.
How to break a bone growth?

As mentioned earlier, a formed bone spur or Haglund’s deformity cannot be removed by conservative treatment methods. In such cases, you have to resort to surgical treatment. Removal of exostosis on the heel can be done using two methods:
- Open. First, the Achilles tendon is carefully pushed back using a special tool to avoid damage. Then, using a medical file, the bone growth is cut down.
- Endoscopic. The operation is performed with minimal trauma to healthy tissue. It is enough to make two small measurements of half a centimeter to remove a bone growth on the heel bone.
For the first 7 days after surgery for Haglund's deformity, independent movement is allowed, but with limited load on the lower limb that was operated on. If necessary, you can use crutches. At the beginning of the postoperative period, anti-inflammatory painkillers and antibacterial drugs are prescribed to prevent infection.
Dressing must be carried out until the healing process of the postoperative wound is completed. Physiotherapeutic procedures are used from the first days after surgery. Thanks to these methods, it is possible to reduce swelling and pain. As a rule, magnetic therapy and laser therapy are used. In most cases, the course consists of 10 sessions.
Typically, sutures should be removed within 10-12 days. Sometimes sutures are made intradermally using absorbable threads. In such situations, there is no need to remove anything. Complete recovery lasts 1-1.5 months.