A chemical eye burn is an emergency that requires immediate medical attention. It is important to properly cleanse the mucous membrane of the irritant in order to achieve complete healing in the future. You need to know how to properly provide first aid for an eye burn with chemicals, so as not to worsen the damage.

How can you burn your eyes?
Most often, chemical burns to the eyes occur at work. You can injure the mucous membrane at home if you do not follow safety precautions when using household chemicals, lime, and ammonia. Even if a small amount of the substance is used, gloves and special safety glasses must be worn. Regular glasses do not adhere to the skin and leave pathways for irritants to enter.
Eye burns can occur during eyelash extensions. The glue used in the salon is a strong irritant. Contact with it causes swelling, itching, burning, redness and pain.
Chemical burns to the eye are a common consequence of using a gas spray for self-defense. Upon contact with an irritant, blepharospasm may occur, that is, the eye will close abruptly and will not open. Usually the spasm lasts for an hour if the eye is not washed out in time. It is recommended to blink for 5 minutes after rinsing to restore muscle function.
Degree of eye burn
Almost all chemicals can irritate the mucous membranes of the eye, but serious damage occurs upon contact with strong alkalis and acids. Alkali burns occur most often, but they are also the most dangerous, especially with bilateral damage. Often such injuries result in visual impairment.
The severity of a chemical burn will depend on the volume, temperature and concentration of the irritant, duration of exposure and degree of penetration. In some circumstances, the person's age is also important: in general, children tend to have more severe burns.
There are four degrees of eye burn, but the mechanism of damage by alkalis and acids is different. The initial assessment of burn severity is based on the degree of corneal transparency and the severity of ischemia (blanching).
Degree of eye burn:
- First degree (favorable prognosis). It is characterized by the absence of ischemia and the transparent state of the cornea.
- Second degree (good prognosis). Ischemia affects a third of the limbus, there is clouding of the cornea, but details of the iris are visible.
- Third degree (ambiguous prognosis). There is clouding of the corneal stroma, the epithelium is completely lost, ischemia from a third to half of the limbus masks the details of the iris.
- Fourth degree (poor prognosis). Ischemia affects most of the limbus, and there is total opacification of the cornea.
Additionally, the filling of limbal vessels is considered. When determining the degree, the extent of destruction of the corneal epithelium, the presence of symptoms of conjunctivitis, the condition of the lens and iris, as well as indicators of intraocular pressure are also taken into account.

Features of burns with acids and alkalis
Eye burns from sulfuric acid are not as dangerous as from alkali. This is due to the fact that a film of coagulated protein forms on the eye when the irritant reacts with the mucous membrane. The film does not allow acid to penetrate deep into the eye, protecting the eye from deep damage. However, coagulation does not protect against complications if a concentrate of nitric and hydrofluoric acids gets into the eyes. An acid burn is characterized by severe pain, and sometimes even painful shock.
It is noteworthy that when the eye is damaged by alcohol, a person experiences severe pain, but minimal damage is noted. However, alcohol can absorb moisture from the lubricating fluid and the eyeball, penetrating deep into and damaging the cornea and lens. If washed in a timely manner, there will be no consequences for vision.
The most dangerous are alkali burns. In this case, there is severe dehydration and cell destruction. Alkalies provoke the decomposition of protein structures, wet necrosis develops, and when the irritant gets into the intraocular fluid, the deep structures of the eye are affected. Alkali can reach the corneal stroma and trabecular meshwork. As a result, the cornea becomes cloudy and intraocular pressure increases.
Common symptoms of a chemical burn
- Deterioration of vision. The initial decrease in visual acuity is caused by epithelial defects, increased lacrimation, clouding and discomfort. Even with moderate to severe burns, vision may be preserved if the corneal clouding is minor, but severe deterioration will occur over time.
- Fragments of the irritant in the arches of the outer shell. Residues of foreign matter are visible when plaster and other solid irritants enter the eye. The fragments must be removed immediately, otherwise they will continue to release toxins and worsen the damage. Only after cleansing the eye does the natural recovery process begin. Carbide and lime are the most dangerous because they dissolve in the tear and cause severe damage. If these substances come into contact, do not delay cleansing.
- Increased intraocular pressure. A sharp increase in pressure occurs due to deformation and contraction of collagen fibers in the anterior part of the eyeball. Subsequently, the increase is associated with inflammation.
- Inflammatory process in the conjunctiva. Even with mild damage, swelling and redness of the mucous membrane is noted. Sometimes when a burn occurs, the color of the conjunctiva changes (brown when affected by chromic acid, yellowish when exposed to nitric acid).
- Perilimbal ischemia. Based on the degree of blanching, one can make a prediction about the restoration of the cornea, because limbal sprout cells restore the epithelium. Severe ischemia indicates an unfavorable course of the process.
- Cloudiness. If the cornea is transparent, a zero degree of damage is determined, and if the cornea is completely clouded, the fifth degree is determined. Complete stromal opacification makes it impossible to examine the anterior chamber of the eye.
- Defects of the corneal epithelium. Damage to the cornea can be expressed as diffuse punctate keratitis or complete absence of the epithelium. In the latter case, the defect is poorly stained with fluorescein and may not be diagnosed. If the epithelial defect is not visible during the initial examination, prompt re-examination is recommended.
- Corneal perforation. The symptom appears a few days after a severe eye burn, when the cornea's ability to regenerate decreases.
- Inflammation in the anterior region. The reaction may affect single cells or have a pronounced fibrinoid form. Inflammation is more pronounced when alkali gets into the eye, since these substances can penetrate deep into the structures.
- Scarring or other damage to the conjunctiva and eyelids. The symptom may be a problem if scarring prevents the palpebral fissure from closing.

What to do if you have a chemical burn to the eye
Before providing first aid, you need to transfer the victim to a dark room to minimize the effect of light on the eyes and relieve pain. Folk remedies for chemical eye burns are ineffective, and some can be dangerous. Do not wash your eyes with tea or herbal infusion. It is not recommended to refuse the help of doctors in favor of traditional medicine.
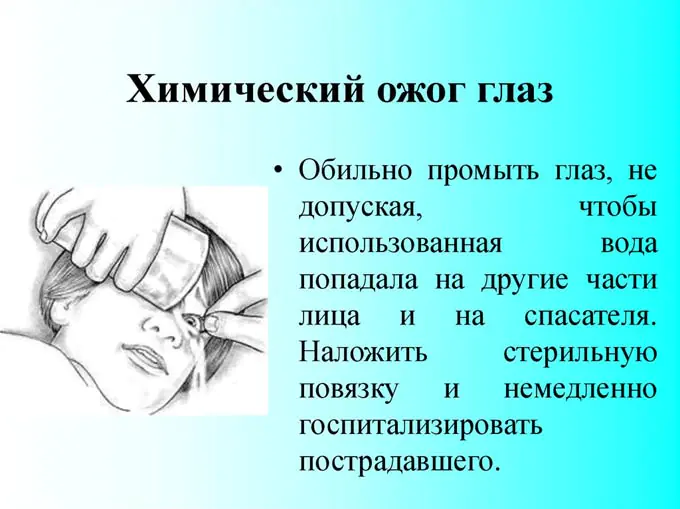
First aid for a chemical burn to the eye:
- Remains of the substance are removed from the eyelids with a cotton swab.
- The eyes are rinsed generously under running water for 15 minutes. It is recommended to additionally wash alkaline burns with a 2% boric acid solution, and acid burns with a soda solution.
- If there is severe pain, the patient should be given an effective pain reliever.
- Instill a 4% solution of novocaine or lidocaine, or a 0.2% solution of chloramphenicol.
- Use a disinfectant (0.25% Levomycetin, Sebizone, Albucid-sodium, Acetopt, Ophthalmite, Gentamicin drops).
Rinsing should last more than 15 minutes. You can use clean water, sodium chloride solution (0.9%) or a weak solution of potassium permanganate. If it is not possible to use a special solution, tap water can be used. Potential infection in the long term is not as dangerous as long-term poisoning from the remnants of the irritant.
Treatment of chemical burns to the eye
The entire process of treating a chemical burn can include both conservative and surgical methods. The main thing is to preserve vision. Patients with severe burns need to be hospitalized immediately. In case of damage to degrees I and II, it is advisable to consult a doctor after providing first aid and follow all recommendations at home.
Stages of treatment for chemical eye damage:
- Removing the irritant. The most important step in emergency care for chemical burns is copious rinsing. If possible, the eye should be anesthetized before rinsing. Local anesthesia reduces pain and blepharospasm. It is advisable to use a sterile buffer solution (normal saline or Ringer's solution).
- Control of the inflammatory process. At the time of damage, inflammatory mediators are released, which provoke necrosis. This process inhibits re-epithelialization and increases the risk of ulcers and corneal perforation. You can interrupt the inflammation with the help of local steroids; citrate or ascorbic acid is additionally prescribed. To inhibit collagenosis and prevent ulcers, 10% or 20% Acetylcysteine is sometimes used.
- Acceleration of regeneration. Full epithelization begins only after the irritant is removed from the eye. Chemical damage causes a temporary increase in tear production and a decrease in future tear production, so it is important to use moisturizers for healing. Ascorbic acid helps restore collagen structure and accelerate corneal regeneration. In some cases, wearing therapeutic bandage lenses is recommended.
Since chemical burns to the eyes are accompanied by severe pain, the victim is prescribed powerful anesthetics. Additionally, anti-inflammatory drugs and drugs that prevent the formation of adhesions are used. Treatment of burns usually begins with tetanus vaccination.
Glucocorticosteroids
If severe inflammation develops during a burn, doctors prescribe glucocorticosteroids:
- Dicaine. Eye drops with leocaine and sodium chloride have a local anesthetic effect, relieve pain and prepare the cavity before surgery. The dosage is determined by the degree of burn.
- Ciprofloxacin. The ophthalmic drug is available in the form of drops or ointment, but in case of a burn, the use of a solution is recommended. Ciprofloxacin has antibacterial and anti-inflammatory effects. The drug is instilled every 15 minutes for the first 6 hours, then every half hour the next day. On days 3-14, the interval is increased to 4 hours. Ciprofloxacin is only allowed in patients over 1 year of age.
- Atropine. For chemical burns to the eyes, this remedy helps reduce pain and prevent adhesions. The active ingredient is atropine sulfate. The drug is instilled three times a day, 1-2 drops.
- Diacarb. The drug in tablet form is prescribed for increased intraocular pressure. The effectiveness of Diacarb is due to the content of acetazolamide, magnesium stearate, povidone, croscarmellose sodium and other substances. Usually prescribed one tablet 3-4 times a day. Diacarb is contraindicated in diabetes mellitus, acute liver and kidney failure, uremia, hyponatremia, metabolic acidosis, hypokalemia, in the first trimester of pregnancy and during lactation. The drug is prescribed to patients over 3 years of age.
- Prednisolone. This glucocorticosteroid is taken only with the permission of a doctor. Usually prescribed one tablet per day. Prednisolone is contraindicated for fungal infections.
Although chemical burns require emergency treatment, the prognosis is often good. If the damage did not affect the deep structures of the eye, and the appropriate measures were carried out in a timely and correct manner, the preservation of vision will be ensured. In some cases, even immediate help does not prevent the formation of an eyesore. Even after successful treatment, scars may remain and affect the quality of vision.
Relieving pain from eye burns
A serious chemical burn does not occur without prolonged and severe pain. At the initial stage, oral analgesics are most often used. The spam of the ciliary muscle can be weakened with the help of cycloplegic drugs.

Prevention of secondary infection
If the burn has severely damaged the corneal epithelium, the risk of infection increases. At the initial stage of therapy, antibiotics are prescribed for prophylaxis. Minor, deep corneal injuries can be treated with cyanoacrylate eye glue.
Monitoring intraocular pressure
If elevated pressure levels are observed during a burn, blockers of the production of intraocular fluid are prescribed. Such drugs are indicated both at the initial stage of treatment and during late rehabilitation therapy. When elevated intraocular pressure persists even with the use of antihypertensive agents, surgical intervention (penetrating antiglaucoma or surgery with shunt or valve devices) is required.
Surgical treatment of eye burns and possible complications
If conservative methods are ineffective, surgical treatment of the consequences of the burn is performed. Depending on the complications, a variety of techniques are used.
Surgical treatment for an eye burn may include:
- partial removal of areas of necrosis of the conjunctiva or corneal surface;
- temporary covering with amniotic membrane;
- transplantation of limbal cells or cultured corneal epithelial cells;
- removal of the fusion of the conjunctiva of the eyelids with the eyeball (symblepharon).
To speed up rehabilitation, penetrating or partial keratoplasty and keratoprosthesis are used. If a cataract occurs, it is extracted.
Primary complications of a chemical burn include conjunctivitis, corneal erosion, swelling or clouding, acute increase in intraocular pressure, and melting of the cornea. Secondary complications are usually more varied.
Possible consequences of a chemical burn to the eye:
- glaucoma;
- cataract;
- scarring of the conjunctiva;
- corneal ulcers;
- thinning and tearing of the cornea;
- destruction of the corneal surface;
- opacification and vascularization;
- subatrophy of the eye.
The main measure to prevent burns is to follow safety precautions when working with household chemicals and in production where chemicals are used. It is important to exercise caution and wear safety glasses.
Eye burns can occur in various situations, for example, when welding safety precautions are not followed. If damage to the mucous membrane of the eye occurs, patients complain of pain and a burning sensation. There is also redness of the cornea, decreased tissue transparency and deterioration in visual function.
If an injury is noted, the first step is to consult a doctor. After consultation with an ophthalmologist, the victim will be prescribed appropriate treatment for an eye burn. Most often, patients need to use several types of drops designed to disinfect and speed up recovery processes.
Review of eye drops for burn treatment

To avoid the consequences of eye burns, you must follow the course of treatment prescribed by your doctor. In most cases, several groups of drugs are prescribed. Each of them acts differently on the affected area. Some only disinfect the mucous membrane, others have an anti-inflammatory effect. Therefore, to eliminate unpleasant symptoms, not one, but several types of drops are usually prescribed. Depending on their functions, they can be divided into the following categories:
- medications that relieve tissue swelling and eliminate inflammatory processes. This includes drugs such as Visin, Octilia, Visoptic. It is required to instill them 1 drop up to three times a day for 2 – 3 days. With regular use, patients experience burning sensation, swelling, and redness;
- painkillers, for example, Lidocaine, Novocaine, Alcaine. They are used a little less often - up to 2 times a day. The duration of treatment should not exceed 2 days. During this time, the drops will cope with pain, as they act on the receptors of the mucous membrane. If after stopping use the pain returns, the attending physician can decide to continue the course;
- the next group is medications with an antibacterial effect, such as Levofloxacin, Gentamicin, etc. Duration of use reaches a week. At this time, it is necessary to apply the products up to 5 times daily. They primarily prevent infection from penetrating into the affected tissues, and also contribute to accelerated recovery and reduction of pain;
- The last category of drops is anti-inflammatory. Ophthalmologists in most cases prescribe Prenacid, Diclofenac, etc. The drugs help prevent complications and also accelerate tissue regeneration by eliminating inflammatory processes.
Let's consider several medications that are most often used in the treatment of burns of the mucous membranes, as well as to eliminate other ophthalmic pathologies:
- Visine. This is a topical remedy that effectively eliminates swelling and redness. Its action is based on the constriction of blood vessels, so the result after use occurs in the shortest possible time. Within a minute the patient notices an improvement in his condition. However, the effect does not last long - on average 6 hours, after which the drug will need to be instilled again. Visine should not be used for long periods of time as it may worsen the problem. Application can last 3–4 days, after which you need to take a break;
- Proculin is a solution with a wide range of applications. Its action is also based on the vasoconstrictor effect. By analogy with Visin, the medication allows you to quickly relieve pain and restore clarity of vision. However, the result is short-lived and the instillation will have to be repeated after a few hours. The course of treatment should not last longer than 3 days to avoid complications;
- Visoptic is another popular vasoconstrictor solution. The effect occurs a few minutes after instillation into the eyes and lasts up to 8 hours. The composition of the drops allows you to quickly eliminate swelling, get rid of redness and a burning sensation.
It is important to remember that vasoconstrictor drugs do not cure, but only relieve acute symptoms for a while. Therefore, they must be used in combination with other means.
Features of application
Only a doctor can prescribe suitable medications that do not damage retinal cells. The severity of the patient's eye damage determines the specific use of certain agents.
If a burn occurs, eye drops should be instilled onto the mucous membrane, slightly pulling the eyelid. Typically up to 2 drops are required for each eye. The mucous membrane needs to be treated 2 – 3 times a day. However, the specific method of application depends on the condition of the victim and the types of medications. Most often, drops are used for no more than 4 days. Your doctor may prescribe a different course of treatment.
A significant portion of drugs are contraindicated for use in children under 7 years of age. Other types of products are produced for them, the dosage of active ingredients in which is much lower.
At what stages of a burn can drops be used?
Doctors prescribe medications even in the most severe cases. They perform the functions of disinfection and tissue regeneration, including in cases of serious damage to the mucous membrane. However, there is no point in using drops for retinal burns at the very last, fourth, stage. In this case, the damage is so extensive that complex treatment is required.
The effectiveness of the drugs has been proven for stages 1 and 2 injuries. In these cases, they cope with the task. At stage 3, serious therapy is required and the victim cannot cope with the use of drops alone.
Medicines intended for instillation show good results for 1st and 2nd degree burns of the organs of vision. In the presence of more serious damage, their use is practically meaningless. Stages 3 and 4 will require an integrated approach. The course of medications must be chosen by the attending physician.
Eyes are the most sensitive human organs to external influences. Any aggressive contact of the delicate eye structures with chemicals, steam, hot objects, fire, ultraviolet radiation leads to severe damage and often to dire consequences. Therefore, it is important to know how to protect the organs of vision and how to provide first aid for various types of eye burns.

Causes and classification
Mostly, the eyes suffer from chemical and thermal burns, since almost all people daily interact with household chemicals, which include various chemicals. Careless handling of plumbing cleaners or laundry detergents can result in chemical burns. And thermal damage can easily occur during careless cooking. Drops of hot oil or fat or steam entering the mucous membrane of the eye cause a thermal burn. Radiation injury is much less common.

Depending on what caused the burn, the following types of lesions are distinguished:
- Thermal. They develop as a result of exposure to high temperatures due to hot splashes of fat entering the eye during cooking, exposure to steam, sparks from fireworks, etc. The skin of the eyelid, conjunctiva, and cornea are more often injured from thermal effects, and burns to deeper ocular structures are less likely to occur.
- Chemical. Similar damage is caused by alkalis and acids. Lead to the death of cells that are directly exposed. Among the acids that most often injure people's eyes, they are sulfuric, hydrochloric and acetic acids. They are part of many household chemicals. When affected by acid, the protein in the eye mucosa curls up and prevents the chemical from penetrating into the deeper layers. Alkalies penetrate into the ocular structures, destroy cells and contribute to the development of wet necrosis. They differ in the duration of action of the damaging substance. It gradually penetrates through the superficial tissues from the site of damage to the deeper layers. Among alkalis, burns are most often caused by potassium, magnesium, sodium hydroxide, lime, and ammonia.
- Radiation. Caused by prolonged or sudden exposure of the eyes to ultraviolet (short-wave) or infrared (long-wave) rays. The damage is called electroophthalmia. Ultraviolet light causes burns to the skin, cornea, and conjunctiva. Long waves easily penetrate the cornea and injure the retina. Ultraviolet burns can occur as a result of abruptly leaving the dark into a brightly lit place or while observing a solar eclipse without appropriate protection. Most often, long-wave rays injure the eyes of people working with welding.
Symptoms
When eye burns occur, tissue cells die, causing blood clots to appear in the capillaries, and plasma leaks into the surrounding tissues.
All types of burn injury are accompanied by similar symptoms:
- swelling of the cornea, conjunctiva;
- severe pain in the eye;
- redness of the skin of the eyelids and eyeball;
- photophobia;
- changes in visual fields;
- lacrimation;
- increase or decrease in eye pressure;
- decreased visual acuity;
- corneal clouding;
- blepharospasm, in which it is difficult to open the eyelids.

First aid
In case of eye burns, it is important to provide first aid to the person as quickly as possible. The preservation of vision often depends on this.
First aid boils down to the following:
- removing residual damaging substances using a sterile cotton swab;
- rinsing the eyes with clean water or saline solution from a large syringe for 15 minutes (if the burn is caused by an alkali, rinsing is carried out with a 2% boric acid solution. When exposed to acids, a soda solution is used for rinsing);
- instillation of a solution of novocaine, lidocaine (4%) or Levomycetin (0.2%). You can use Acetopt, Sofradex. It is better to perform the procedure in a darkened room, as instillation is very painful.

Drug groups
Therapeutic measures for all types of burns are quite similar, only the doses and duration of the therapeutic course differ depending on the degree of damage to the eye structures.
The main groups of drugs that are used for burn injuries to the eye are shown in the table.
| Drugs. | The action provided. |
| Anesthetics (Lidocaine, Novocaine). | Eliminate pain syndrome. |
| Local antibiotics (Levomycetin, Lincomycin drops, Sulfacyl). | Prevent inflammation. Help minimize the risk of infection of the affected organ. |
| Artificial tear preparations (Visine). | In case of a burn to the mucous membrane of the eye, these drops are necessary to moisturize and protect the damaged organ. |
| Hypotensive (Gunford, Dorzolamide, Betaxol). | Reduce eye pressure. |
| Mydriatics (Atropine, Ephedrine). | Needed for normal pupil dilation and normalization of the iris. |
| Cytoplegic (Scopolamine). | Designed to relieve pain symptoms and prevent adhesions. |
| Glucocorticoids. (Dexamethasone, Betamethasone, Cortisone). | Prescribed for extensive or deep burns to eliminate redness, burning, swelling and swelling of the eyelids. |
| Anti-inflammatory (Naklof or Diklo-F). | Such drops for eye burns are necessary for the regeneration of damaged tissues. |
It is mandatory to use drops containing D-panthenol. This component significantly accelerates the regenerative processes of damaged tissues, and therefore the recovery period takes less time. Preparations that contain panthenol are Korneregel, Vitaglycan.
Drops recommended for different types of burns
For any type of burn, it is important to relieve pain and prevent infection from entering the affected tissue.
For thermal burns
For thermal damage, the following drops can be used:
- Inocaine. The active substance is benoxynate hydrochloride. Local anesthetic that blocks nerve endings.
- Visoptician. Eliminate photophobia, itching, burning, lacrimation, swelling.
- Okomistin. An antiseptic that forms a protective film on injured tissues.
- Prokulin. Relieves swelling, pain, has a vasoconstrictor effect.

As part of complex therapy for burn damage to the eyes, Emoxipin is prescribed, which helps restore energy metabolism in tissues and accelerates their healing, strengthens blood vessels, restores blood circulation, and stimulates regeneration processes.

For radiation burns
Radiation burns are treated with the following drops:
- Corticosteroids. Hydrocortisone, Dexamethasone, which help eliminate local swelling.
- Lidocaine. The solution contains sodium chloride and benzalkonium, lidocaine hydrochloride. Prescribed for eye burns to reduce tissue sensitivity.
- Derinat. Drops with an immunomodulatory effect. They help quickly regenerate injured areas, preventing the appearance of scars.
- Phloxal. Drops with antibacterial action. Prevents infection of damaged tissues.
- Tsiprolet. Antimicrobial drops for a wide range of applications. In case of eye burns, they are instilled 5 times a day, 2 drops into each eye.
- Levomycetin (active ingredient chloramphenicol) acts against most gram-positive and gram-negative bacteria.
Drops for chemical burns

A 1% solution of Dicaine helps with eye burns of chemical origin. This is a local anesthetic that contains sodium chloride and leocaine, which reduces the sensitivity of sodium channels through which pain impulses are transmitted. Drops reduce pain and have a local anesthetic effect.
Atropine is used. The active ingredient of the drops is atropine sulfate. Helps relieve pain and prevent adhesions.
Ciprofloxacin also helps, which has anti-inflammatory and antibacterial effects.
Forecast
The prognosis for a person who has received an eye burn will depend on timely treatment. Most superficial burns disappear without a trace. Moderate and severe damage is fraught with scarring of the eyelids, the development of cataracts, and death of the eyeball. Radiation damage affecting the retina often leads to vision loss.




