Increasingly in recent years, women have experienced problems with conception, pregnancy and childbirth. There are many reasons for this: inflammatory diseases, age, poor health, and so on. In most cases, modern medicine still helps the fairer sex overcome her illness. However, after some treatment methods, scars appear on the uterus. You will learn from the article how they arise and what they threaten. It is worth mentioning separately how a scar on the uterus can be dangerous during pregnancy.
What is a scar?
A scar is tissue damage that has subsequently been repaired. Most often, the surgical method of suturing is used for this. Less commonly, cut areas are glued together using special adhesives and so-called glue. In simple cases, with minor injuries, the rupture heals on its own, forming a scar.
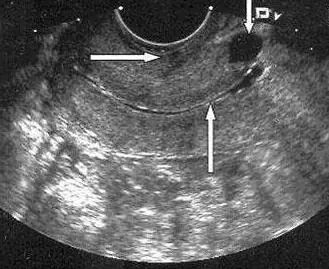
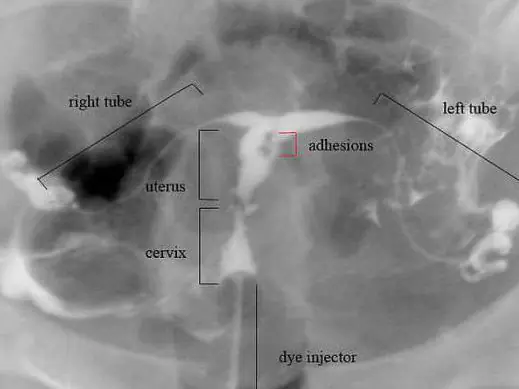
Such a formation can be located anywhere: on the human body or organs. For women, the scar on the uterus is of particular importance. A photo of this formation will be presented to you in the article. Damage can be diagnosed using ultrasound, palpation, and various types of tomography. Moreover, each method has its advantages. So, during an ultrasound, the doctor can assess the position of the scar, its size and thickness. Tomography helps to determine the relief of formation.

Reasons for appearance
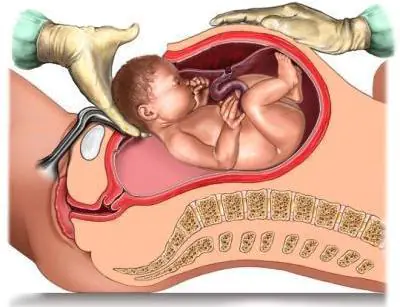
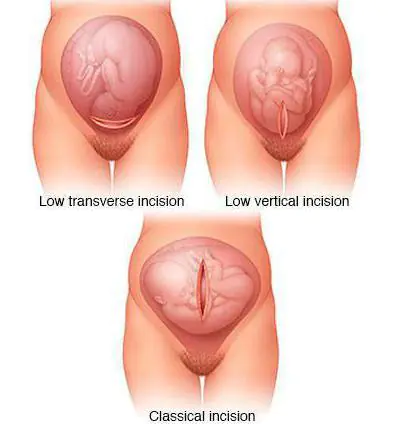
Why do some women develop scars on their uterus? Such damage becomes a consequence of medical interventions. This is usually a caesarean section. In this case, the type of operation plays an important role. It can be planned or emergency. During planned delivery, the uterus is incised in the lower segment of the abdominal cavity. After the fetus is removed, it is sutured layer-by-layer. This scar is called transverse. In an emergency caesarean section, a longitudinal incision is often made. In this case, the scar has the same name.
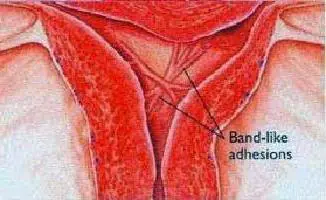
Fused lesions can result from perforation of the uterine wall during gynecological procedures: curettage, hysteroscopy, insertion of an IUD. Also, scars always remain after surgical removal of fibroids. In these cases, the position of the scar does not depend on specialists. It forms where the operation was performed.
Pregnancy and scar
If you have scars on your uterus, the possibility of having a baby depends on their condition. Before planning, you should definitely consult a gynecologist. The specialist will certainly conduct an ultrasound examination to determine the condition and position of the scar. You will also need to undergo some tests. Before planning begins, it is imperative to cure infections. Subsequently, they can cause problems with pregnancy.
If the scar is in the lower segment and has a transverse position, then problems usually do not arise. The fairer sex is examined and released to plan a pregnancy. In the case where the scar turns out to be insolvent, thinned and consisting mainly of connective tissue, pregnancy may be contraindicated. However, in some cases, the hands of surgeons work wonders. And a woman can still give birth.
Management of pregnancy and childbirth with a uterine scar
If you have a scar on the reproductive organ, then you need to inform the specialist who will manage your pregnancy about this. At the same time, you need to tell about the existing fact immediately, at the first visit, and not before the birth itself. Pregnancy management in women with a history of uterine injuries occurs somewhat differently. They get more attention. Also, this category of expectant mothers regularly have to visit an ultrasound diagnostic room. Such visits become especially frequent in the third trimester. Before childbirth, an ultrasound of the uterine scar is performed almost every two weeks. It is worth noting that other diagnostic methods are unacceptable during pregnancy. X-rays and tomography are contraindicated. The only exceptions are special, difficult situations when it comes not only to a woman’s health, but also to her life.
Delivery can be carried out by two methods: natural and operative. Most often, women themselves choose the second option. However, if the scar is intact and the expectant mother is in normal health, a natural birth is quite acceptable. To make the right choice, you need to consult with an experienced specialist. Also, during labor and increasing contractions, it is worth conducting periodic ultrasound monitoring of the condition of the scar and the uterus. Doctors also monitor the fetal heartbeat.
Damage to the cervix
As practice shows, some women who give birth on their own have a scar on the cervix. It occurs due to tissue rupture. During the process of childbirth, a woman feels painful contractions. Attempts begin behind them. If the cervix is not fully dilated at the moment, then they can lead to its rupture. This does not threaten anything for the child. However, the woman subsequently has a scar on her cervix. Of course, after delivery, all tissues are sutured. But in the future this may become a problem during the next birth.
Such a scar at the mouth of the cervical canal can also appear after other gynecological manipulations: cauterization of erosion, removal of a polyp, and so on. In all cases, the resulting scar appears to be connective tissue. During subsequent delivery, it simply does not stretch, leaving the area of the cervix undilated. Otherwise, the damage does not pose any danger to the mother and her unborn child. Let's try to find out why scars located on the reproductive organ can be dangerous.

Attachment of the fertilized egg and its growth
If there are scars on the uterus, then after fertilization a set of cells can attach to them. So, this happens in about two out of ten cases. At the same time, the forecasts turn out to be very dire. On the surface of the scar there is a mass of damaged vessels and capillaries. It is through them that the fertilized egg is nourished. Most often, such a pregnancy is terminated on its own during the first trimester. The consequence can be called not only unpleasant, but also dangerous. After all, a woman needs emergency medical care. Decaying fetal tissue can lead to sepsis.
Incorrect attachment of the placenta
A scar on the uterus after a cesarean section is dangerous because during the next pregnancy it can cause improper attachment of the baby's place. Often women are faced with the fact that the placenta is fixed close to the birth canal. Moreover, as pregnancy progresses, it migrates higher. The scar may prevent such movement.
The presence of a scar after damage to the reproductive organ often leads to placenta accreta. The baby's place is located precisely on the scar area. Doctors distinguish basal, muscular and complete placenta accreta. In the first case, the forecasts may be good. However, natural childbirth is no longer possible. If placenta accreta is complete, the uterus may need to be removed.
Fetal condition
A scar on the uterus can lead to poor circulation in the reproductive organ. At the same time, the unborn child does not receive enough oxygen and all the substances he needs. If such a pathology is detected in a timely manner, it can be treated and supported with appropriate medications. Otherwise, hypoxia occurs, which is fraught with intrauterine growth retardation. In particularly difficult situations, the child may remain disabled or even die.
Uterine growth
In a normal non-pregnant state, the thickness of the walls of the reproductive organ is about 3 centimeters. By the end of pregnancy they stretch up to 2 millimeters. At the same time, the scar also becomes thinner. As is known, fused damage is replaced by connective tissue. However, normally a large area of the scar is represented by a muscle layer. In this case, the scar is considered valid. If the damage thins down to 1 millimeter, this is not a very good sign. In most cases, experts prescribe bed rest and supportive medications to the expectant mother. Depending on the length of pregnancy and the thickness of the uterine scar, a decision may be made to deliver prematurely. This condition has dangerous consequences for the baby.
After childbirth…
Scarring on the uterus after childbirth can also be dangerous. Despite the fact that the baby has already been born, consequences may arise for his mother. Scars are damage to the mucous membrane. As you know, after childbirth, every woman experiences bleeding. The process of separation of mucus and remnants of membranes occurs. These secretions are called lochia. In some situations, mucus may linger on the scar area. This leads to an inflammatory process. The woman requires curettage, her body temperature rises, and her health worsens. In the absence of timely treatment, blood poisoning begins.
Aesthetic side
Often the presence of a scar on the uterus is a reason for a caesarean section. Many women are concerned about their subsequent appearance. An ugly scar remains on the stomach. However, much depends on the surgeon’s technique. Also, the possibilities of cosmetology do not stand still. If desired, you can do plastic surgery and hide the ugly seam.
Summarize
You learned about what a uterine scar is, in what situations it appears and why it is dangerous. Let us note that if you properly prepare for pregnancy and listen to the advice of an experienced doctor when managing it, then the outcome in most cases is good. The new mother and baby are discharged from the maternity ward in about a week. Don't be too upset if you have a uterine scar. Before you start planning, be sure to consult your doctor, undergo routine examinations, and take all tests. After this you can get pregnant.

Experts do not advise starting to plan a pregnancy earlier than two years after receiving such an injury. Also, don’t delay this. Doctors say that after 4-5 years it will be almost impossible to stretch the scar. This is when problems can begin during pregnancy and childbirth. All the best to you!
Symptoms of a scar on the uterus
- The presence of a scar on the uterus occurs without any symptoms.
- Uterine rupture along a scar is a serious complication of the presence of a scar on the uterus, which manifests itself with characteristic symptoms:
- pain in the middle and lower abdomen
- bloody discharge from the genital tract
- strong and irregular contractions (muscle contractions of the uterus)
- deterioration of the mother’s well-being: decreased blood pressure, frequent and barely perceptible pulse, pallor of the skin, nausea and vomiting.
Forms
Causes
- Caesarean section - Uterine rupture can occur at the site where the uterine wall was cut to remove the baby (most often the lower third of the uterus).
- Myomectomy (husking (removal) of fibroids (nodular benign formation of the muscular layer of the uterine wall)) – in the area of fibroids, the muscular layer of the uterine wall becomes significantly thinner.
- Perforation of the uterus (piercing the wall of the uterus) during an abortion or diagnostic curettage.
- Reconstructive operations on the uterus:
- after uterine rupture (violation of the integrity of its walls)
- removal of the rudimentary (residual) uterine horn (a congenital malformation of the uterus, in which the uterus has outgrowths resembling horns in shape - a bicornuate uterus).
An obstetrician-gynecologist will help in treating the disease
Diagnostics
Treatment of uterine scar
A scar on the uterus during pregnancy does not require specific treatment.
Childbirth in women with a uterine scar can occur either through the natural birth canal or through a cesarean section.
Vaginal birth in women with a scar on the uterus are possible with:
- one caesarean section in the past with a transverse scar on the uterus
- the absence of chronic diseases and obstetric complications in a woman (preeclampsia (severe pregnancy with increased blood pressure and impaired renal function), placental insufficiency (impaired placental function (baby place))
- scar consistency (complete restoration of muscle fibers in the area of the uterine scar)
- location of the placenta outside the scar area
- cephalic presentation of the fetus (position of the fetus with its head down towards the internal opening of the cervix)
- correspondence between the sizes of the pelvis of the mother and fetus.
Surgical delivery by caesarean section in case of presence of a scar on the uterus, it is indicated for:
- one caesarean section in the past with a longitudinal scar on the uterus
- the presence of two or more scars on the uterus
- failure of the scar (predominance of connective tissue in the area of the uterine scar)
- location of the placenta in the scar area
- placenta previa (low attachment of the placenta, in which it partially covers the internal opening of the cervix)
- discrepancy between the sizes of the pelvis of the mother and fetus (clinically narrow pelvis)
- scars after myomectomy (removal of fibroids (nodular benign formation of the muscular wall of the uterus) along the posterior wall of the uterus
- scars on the uterus after reconstructive operations (correction of congenital uterine defects, suturing of uterine ruptures (violation of the integrity of the layers of the uterine wall))
- scars on the uterus after cervical pregnancy (the embryo is attached to the wall of the cervix, outside the uterine cavity).
If a complication occurs – uterine rupture along the scar – an emergency cesarean section is indicated to quickly extract the fetus and save the life of the mother and child. The defect in the uterine wall is sutured after the baby is removed.
Surgery to remove the uterus is performed only when the defect in the walls of the uterus is extremely large and it is impossible to suturing it.
Complications and consequences
- Placental insufficiency (impaired functions of the placenta (baby place)).
- Fetal hypoxia (serious condition of the fetus caused by insufficient blood supply due to placental insufficiency).
- Anomalies (disturbances) in the location and attachment of the placenta:
- low location of the placenta (placenta location less than 6 cm from the internal os of the uterus (internal opening of the cervix))
- placenta previa (low attachment of the placenta, in which it partially covers the internal opening of the cervix)
- dense attachment of the placenta (attachment of the placenta in the basal layer of the uterine wall (a deeper layer of the uterine mucosa than the decidulum (where attachment should normally occur))
- placenta accreta (attachment of the placenta to the muscular layer of the uterine wall)
- placenta accreta (the placenta grows into the muscle layer by more than half its thickness)
- placenta germination (the placenta grows through the muscular layer and penetrates into the outermost layer of the uterus - serous).
- Threat of miscarriage (threat of miscarriage, premature birth).
- Uterine rupture (violation of the integrity of the walls of the uterus).
- Development of disseminated intravascular coagulation syndrome (severe disorder of the blood coagulation system with the occurrence of blood clots (intravascular blood clots) and bleeding).
- Hemorrhagic shock (progressive impairment of the vital functions of the nervous system, circulatory and respiratory systems due to the loss of a significant amount of blood).
Prevention of uterine scar
- Pregnancy planning and preparation for it (detection and treatment of a woman’s chronic diseases, exclusion of unwanted pregnancy). It is recommended to plan pregnancy no earlier than 2 years after uterine surgery.
- Timely registration of a pregnant woman at the antenatal clinic (up to 12 weeks of pregnancy).
- Regular visits to an obstetrician-gynecologist (once a month in the 1st trimester, once every 2-3 weeks in the 2nd trimester, once every 7-10 days in the 3rd trimester).
- Early identification of risk factors for uterine rupture by scar in a pregnant woman.
- Careful monitoring of the existing scar on the uterus using ultrasound (ultrasound) is a measure to prevent the threat of uterine rupture along the scar.
- Resolving the issue of planned caesarean section as a method of delivery in the presence of a scar on the uterus.
INFORMATION FOR REVIEW
Consultation with a doctor is required
- Authors
“Guide to outpatient care in obstetrics and gynecology,” edited by V.I. Kulakova. – M.: “GEOTAR-Media”, 2007
“Emergency care in obstetrics and gynecology: a brief guide,” ed. V.N. Serova. – M: “GEOTAR-Media”, 2011.
"Obstetrics: A National Guide", ed. E.K. Aylamazyan. – M.: “GEOTAR-Media”, 2013.
What to do with a uterine scar?
- Choose a suitable obstetrician-gynecologist
- Get tested
- Get a treatment plan from your doctor
- Follow all recommendations
Description
The name contains the whole meaning of the pathological condition. A scar can occur on the uterus as a result of cesarean section, various invasive interventions (removal of myomatous nodes, instrumental abortions, separate diagnostic curettage), uterine ruptures during complicated childbirth and as a result of abnormalities in the development of the uterus, when the blood supply to certain parts of the organ is disrupted. Depending on the amount of connective tissue, scars are divided into complete scars, in which muscle fibers are almost completely restored, they have elasticity, which means they can stretch during pregnancy and contract during childbirth, and defective, which consist almost entirely of connective tissue and are not able to stretch. and risk complications during pregnancy. Defective scars pose a danger, since when the uterus is overstretched during pregnancy and childbirth, a rupture along the scar is possible, which leads to bleeding and accompanying complications. Women who have a scar on the uterus during pregnancy more often than others suffer from complications such as: chronic placental insufficiency, chronic intrauterine fetal hypoxia, edema of pregnant women, polyhydramnios, anemia.
Symptoms
Outside of pregnancy, the scar on the uterus does not manifest itself in any way. It is not a contraindication to pregnancy, however, women with a uterine scar require special attention, since there are known cases of scar rupture before birth. It is advisable to hospitalize such women in labor 4-5 weeks before the expected birth (“for preservation”).
Diagnostics
When planning pregnancy in women with a uterine scar, it is necessary to determine what kind of scar it is: full or defective. When palpating the abdomen, the scar on the skin is moved to the side and the anterior wall of the uterus is massaged. This leads to contraction and hardening of the uterus. With a full-fledged scar, the wall of the uterus will be smooth, since all the tissue contracts evenly. But if there is a defective scar on it, then under the fingers it will be felt like a depression in the wall of the uterus.
The gold standard for diagnosis is ultrasound examination of the uterus and appendages. The result of an ultrasound with a defective scar will be a significant thinning in the lower part of the scar and the presence of connective tissue inclusions.
It is possible to perform hysteroscopy, which is performed on the 4th–6th day of the menstrual cycle. With it, the failure of a postoperative scar is determined when extensive whitish inclusions of various shapes are detected in the scar area, along with pronounced local retractions or thickenings, which are located at the level of the internal os of the uterus and above.
Since in the vast majority of cases a scar is formed after a cesarean section, some features of the postoperative period may indicate its inferiority: a prolonged increase in temperature, suppuration of the postoperative wound, pain in the wound area, and prolonged previous labor.
Treatment
As already mentioned, a scar on the uterus does not cause any discomfort in everyday life and requires attention only during pregnancy and childbirth. Therefore, treatment as such is most often not considered. With a full-fledged scar, complications during childbirth, in the form of uterine rupture, threaten no more than women in labor without a scar. In case of defective uterine scar, dynamic observation and timely assistance in case of complications development are important. Often, the reasons that led to a caesarean section during the first birth (narrow pelvis, weakness of labor, extragenital pathologies and others) do not disappear, and therefore a similar operation is resorted to in subsequent births. But even with a defective scar, independent childbirth is possible if the woman in labor does not have an anatomically or clinically narrow pelvis, there is only one scar and the contractility of the myometrium in the area of the scar is reduced, but not completely impaired. The decision to carry out a natural birth in each case is made individually, depending on the medical indications and wishes of the pregnant woman.
During pregnancy planning, if a woman wishes, it is possible to undergo metroplasty - an operation to restore the integrity of the uterus. In the case of uterine scars, during the operation the failed scar outside of pregnancy is excised and a full-fledged scar is achieved. The operation can be performed laparotomically (with dissection of the anterior abdominal wall), transvaginally or, less traumatically, laparoscopically (with the introduction of a camera and manipulator into the abdominal cavity through small holes). After surgery, contraception must be prescribed for 6 months to avoid pregnancy during scar formation.
Medicines
A uterine scar does not require any drug therapy outside of childbirth. In the vast majority of cases, if there is a scar on the uterus, a planned cesarean section is chosen as the method of delivery. Often, during a caesarean section, epidural anesthesia is used, which allows the woman in labor to remain conscious, but not experience pain. For epidural anesthesia, combinations of drugs Promedol + Seduxen + Drotaverine, Meperidine + Promethazine are used. The drugs are injected into the spinal canal at the level of 3-4 or 4-5 lumbar vertebrae, which causes complete anesthesia of the lower extremities, buttocks and lower third of the abdomen.
Medicines used during childbirth are prescribed based on current need. For pain relief during labor, depending on the stage of labor, tranquilizers (Seduxen, Trioxazine), antispasmodics (Drotaverine, Papaverine), narcotic analgesics (Tramadol, Promedol), inhaled analgesics (nitrous oxide, Methoxyflurane) are used. Prenatal psychological preparation has a very good effect women in labor who have undergone such training endure childbirth and the postpartum period much easier.
At any stage of labor, labor weakness may appear. To prepare the uterus for childbirth, Oxytocin, prostaglandin F2a, and prostaglandin E2 are used. They stimulate uterine contractions, and also make them communicated and symmetrical. If labor, on the contrary, is too violent and develops faster than the woman in labor and the fetus can bear, tocolytics (Partusisten, Bricanil) and antispasmodics are used.
Bleeding, as a complication of childbirth, can occur due to uterine rupture, placental abruption, damage and rupture of the soft tissues of the birth canal, and is a life-threatening condition that requires immediate action, which necessarily includes surgical measures. In this case, Oxytocin is also administered, since in the postpartum period it promotes rapid contraction of the uterus and a decrease in the lumen of the uterine vessels. Transfusion of blood components: red blood cells and platelets may well be required. Infusion therapy is required, to replenish the volume of circulating blood - solutions of Sodium chloride, Ringer, Glucose.
A scar on the uterus in no way means a mandatory encounter with the above-described complications of childbirth they depend on many factors, but, unfortunately, it can be one of the predisposing factors.
Folk remedies
Since a scar on the uterus requires observation only if pregnancy and childbirth are planned, folk remedies, as well as drug therapy, are not used in everyday life. If a woman had a caesarean section, the scar in the lower abdomen may cause some discomfort. In order to make it less noticeable, they resort to various folk remedies. But it should be remembered that scar tissue does not respond well to any kind of influence, and therefore you should not count on a rapid reduction or decrease in pigmentation.
For scars, the following folk recipes are used.
- Fresh juice onions rubbed into pre-steamed skin in the scar area several times a day at night, compresses with chopped onion are used. The procedure is repeated daily, for a long time.
- Compresses and lotions with decoctions medicinal herbs: sage, chamomile, parsley, plantain, kalanchoe, dandelion. Due to its fleshy leaves and abundant amount of gelatinous juice, Kalanchoe can be used without preparing a decoction.
- Suitable for daily rubbing natural honey And beeswax, which contain a lot of biologically active substances that promote skin regeneration.
- Essential oils lavender, rosemary, and sea buckthorn also promote healing quite effectively.
There are many modern methods for dealing with scars, but not all of them are painless and are prescribed depending on the type of scar, its age and size. To effectively get rid of a skin scar, you should consult a doctor to select a treatment method individually.



