Under the influence of various unfavorable factors, the process of death of heart cells can begin. As a result, they are replaced by scar tissue, characterized by a high content of protein and collagen. In medicine, the pathology is usually called cardiosclerosis. It is important to understand that a scar on the heart is a condition that poses a danger not only to the health, but also to the life of the patient. In this regard, when the first alarming signs occur, you should contact a cardiologist. The specialist will issue a referral for comprehensive diagnostics, based on the results of which he will create the most effective treatment regimen. Therapy may include both conservative and surgical techniques.
Pathogenesis
It is important to understand that a scar on the heart is a protective reaction of the body that occurs when necrotic foci form. In most cases, death of heart muscle cells occurs after a heart attack.
As soon as the process of cell death begins, connective tissue begins to form in this area. In this way, the body tries to prevent an increase in the area of necrosis. However, the scar on the heart after a heart attack cannot perform the functions of the organ. That is why the formation of connective tissue is only a temporary solution to the problem, which often leads to the development of life-threatening pathologies.
It is important to understand that a scar on the heart is a condition that prevents the development of acute myocardial failure and death. But it also delays the development of all kinds of complications. This is due to the fact that heart failure takes on a chronic form, characterized by constant alternation between periods of remission and relapse.
Etiology
A scar always forms in the area of muscle fiber rupture or in areas of necrosis. The body starts the synthesis of fibrin protein, which quickly fills the damage.
Causes of scars on the heart:
- Thrombosis and embolism of blood vessels. According to statistics, half of the world's population aged 40 years and older suffer from pathological changes. For example, a combination of increased blood clotting and even the initial stage of atherosclerosis leads to thrombosis. The resulting clot of liquid connective tissue partially narrows the lumen of the vessel. As a result, heart cells do not receive the required amount of nutrients and oxygen and begin to die. This situation is life-threatening, so fibrotic changes occur very quickly.
- Myocarditis. One of the most common causes of heart scars. Under the influence of unfavorable factors (allergy, infection, etc.), the myocardial muscle tissue becomes inflamed. As a result, dilatation develops, causing the heart to wear out and become damaged. Microtraumas are subsequently replaced by connective tissue.
- Cardiac ischemia. This term refers to a pathological condition characterized by chronic oxygen starvation of the myocardium. As a result, the process of degenerative-dystrophic changes is launched.
- Heart attack. A scar on the heart appears after it most often. The danger is that sometimes a heart attack is asymptomatic, and changes are detected only on an ECG.
Doctors identify myocardial dystrophy as a separate cause of scar formation. This is a pathological condition in which atrophic changes are noticeable in the heart, that is, the tissue is weaker and thinner than it should be.
- Vitamin deficiency in the body.
- Lack of magnesium, calcium and potassium.
- Excess body weight.
- Frequent and high-intensity physical activity.
Doctors say that if at least one close relative has a heart scar after a heart attack, it is necessary to visit a cardiologist annually for prevention.
Types of scars
Against the background of various pathologies, fibrosis of one of three types can form:
- Focal. It has clear boundaries and a specific location. For example, the scar may be on the back wall of the heart muscle.
- Diffuse. It differs in that it affects all tissues.
- Diffuse-focal. This form is mixed. It is characterized by the presence of small pathological foci that are evenly distributed over the entire surface of the heart. Sometimes scars grow together.
Cardiologists say that scars on the heart are a pathology, the treatment of which is not only complex, but also lengthy. In most cases, doctors create a treatment plan aimed at maintaining the functioning of the organ.
Clinical manifestations
Symptoms and their severity directly depend on what disease caused the damage to muscle tissue. Cardiologists say that scars on the heart after a heart attack (a photo of the affected organ is shown schematically below) can form over several years. In this case, the process is often asymptomatic.
The absence of clinical manifestations is due to the fact that the organ manages to maintain contractility and compensate for the volume of normal tissue. When it is no longer able to function fully, the following symptoms appear:
- Painful sensations in the chest.
- Severe shortness of breath.
- Swelling of the face and limbs.
- Severe fatigue even after minor physical exertion.
- Increased degree of fatigue.
Over time, the fingertips on both the upper and lower extremities acquire a bluish tint. This is a specific sign of severe heart failure. At this stage, doctors take measures to prevent further damage to the heart. Often the only way to save the patient’s life is surgery.
Diagnostics
If the first alarming signs occur, you should contact a cardiologist as soon as possible. The specialist will collect anamnesis, conduct a physical examination and issue a referral for a comprehensive diagnosis, including the following studies:
- ECG.
- Dopplerography.
- EchoCG.
- X-ray.
- Coronary angiography.
Based on the diagnostic results, the doctor draws up the most effective treatment regimen. In severe cases, he evaluates the feasibility of surgical intervention.
Drug treatment
Conservative therapy involves taking medications whose active components help maintain heart function. In addition, patients need to follow the principles of a healthy lifestyle.
The choice of medications is made by the attending physician based on the diagnostic results. The cardiologist prescribes medications that improve heart function by accelerating metabolic processes and restoring the circulation of fluid connective tissue.
An effective method is stem cell treatment. Against the background of their use, natural processes of restoration of affected tissues are launched in the body. They are noticeable soon after the introduction of a cardiomyoblast (a specific cellular element). During treatment, the contractility of the organ is restored and blood circulation improves. In addition, atherosclerotic plaques dissolve, vessel walls are strengthened and necrosis is prevented.
If a heart attack develops as a result of ischemic disease, urgent medical treatment is indicated, which involves taking or intravenously administering the following drugs:
- Beta blockers.
- Diuretics.
- Metabolites.
- Nitrates.
- Acetylsalicylic acid.
If a scar on the heart was discovered during an ECG, you need to be prepared for the fact that it will increase in size for several more months. This information is also relevant for patients who have already undergone treatment. If your health suddenly deteriorates, you must call an ambulance. It is possible that emergency surgery will be required.
Self-medication is strictly prohibited. The wrong choice of drug can be fatal.
Installation of a pacemaker
This is a type of surgical treatment during which the surgeon implants a device in the patient whose task is to maintain normal heart conduction and rhythm. Installation of a pacemaker has no contraindications. In other words, the operation can be performed even on children.
In rare cases, the device is rejected by the body. Typically, this occurs in 2-8% of elderly patients.
Donor organ transplantation
This is a radical operation, which is performed only if it is impossible to save the patient’s life using other methods. Donor organ transplantation is performed only on persons under 65 years of age.
Contraindications are serious pathologies of internal organs, which in practice is very rare, since, for example, both atherosclerosis and ischemia are on the list of restrictions.
Bypass surgery
The essence of the operation is to expand the lumen of the affected blood vessels. As a rule, this type of surgical intervention is prescribed for severe atherosclerosis. This is a disease in which plaques consisting of “bad” cholesterol settle on the walls of blood vessels. They narrow the lumen, as a result of which the heart does not receive the required amount of oxygen and nutritional components. The natural consequence is tissue necrosis.
If the lumen is completely blocked by plaques, the surgeon creates a new vessel to bypass the affected one. This can significantly improve tissue nutrition and, accordingly, heart function.
Aneurysm removal
This is a specific bulge that most often forms in the area of the left ventricle or the posterior wall. After the aneurysm is removed, the blood stops stagnating, and the heart muscle again receives the necessary amount of nutrients and oxygen.
Why are scars dangerous?
Many patients are interested in how long they live with a scar on the heart. It is important to understand that the prognosis depends not only on the underlying disease, but also on the timeliness of seeing a doctor. What is it, the causes of scars on the heart, how to treat the pathology - the cardiologist provides all information regarding the disease during the appointment.
The most unfavorable prognosis is considered if the scar has formed in the area of the left ventricle. This area is subject to the greatest load, which means its damage will invariably lead to the development of heart failure. In addition, other organs (including the brain) will begin to suffer from hypoxia, not receiving the required amount of oxygen.
A condition in which both the left ventricle and the mitral valve are affected is also a life-threatening condition. In this case, a life-threatening pathology develops - aortic stenosis.
If you consult a doctor in a timely manner and follow all recommendations, the patient has every chance of living a very long time.
Prevention
Cardiosclerosis is a disease of the cardiovascular system. In this regard, both primary and secondary prevention consists of observing the following rules:
- Balanced diet.
- Regular but moderate physical activity.
- Quitting smoking and drinking alcoholic beverages.
- Avoiding getting into stressful situations.
- Frequent walks.
- Spa treatment.
In addition, it is necessary to be examined annually by a cardiologist in order to prevent pathologies of the cardiovascular system.
Finally
Sometimes, based on research results, the doctor diagnoses a “scar on the heart.” What does this concept mean? A heart scar is a pathological condition that is a kind of protective reaction of the body to myocardial damage. The formation of dense connective tissue is triggered when the integrity of the muscle is damaged or when areas of necrosis appear on it. Despite this, the pathology needs treatment. It is important to understand that scar tissue cannot perform the functions of the heart, which means that sooner or later it will cause the development of other diseases. The doctor draws up a treatment regimen based on the results of instrumental diagnostics. The treatment plan may include both conservative and surgical methods.
A scar after a heart attack always appears in place of dead tissue. Connective tissue fills certain areas of the myocardium. It is not as elastic as heart tissue and cannot contract, so it significantly disrupts its function. To eliminate the problem, surgical and alternative treatment methods are used.
Why is it formed
A scar is the connective tissue that fills the space that formed at the site of damage to part of the myocardium. This process occurs as a result of inflammatory diseases or after a heart attack. Such damage to the heart muscle is often associated with atherosclerotic changes in the blood vessels.
If oxygen does not reach the tissues of the heart and the cells begin to die, a scar will subsequently form at this site. The problem can also occur when:
- cardiac form of rheumatism. The pathology is characterized by inflammation of the myocardium and cardiac membranes. The disease develops as a result of infections caused by infection with streptococcus. In this case, the epicardium is affected, subsequently it becomes scarred and thickened. This allows you to maintain normal heart function;
- coronary heart disease. It leads to death in 90% of cases. It develops as a result of scarring or may be the cause of it, causing a heart attack;
- myocardial infarction. If a person survives an attack and undergoes a course of treatment, then gradually the wound formed due to necrosis scars. This disease most often causes an increase in the amount of connective tissue in the heart.

Scars appear not only due to pathologies of the heart and blood vessels.
If a person does not eat properly, is constantly exposed to stress, and suffers from endocrine system disorders, then he has every chance of developing cardiosclerosis.
Replacement of muscle fibers and valve deformation occur under the influence of:
- diabetes mellitus;
- anemia;
- amyloidosis;
- overweight;
- metabolic disorders;
- excessive physical activity, which causes the heart to wear out faster;
- hemosiderosis.
Rarely, pathology is detected in newborns, which is associated with congenital heart defects.
It happens that people suffer a heart attack without noticing. If the symptoms are mild, then the attack is confused with tachycardia or angina.
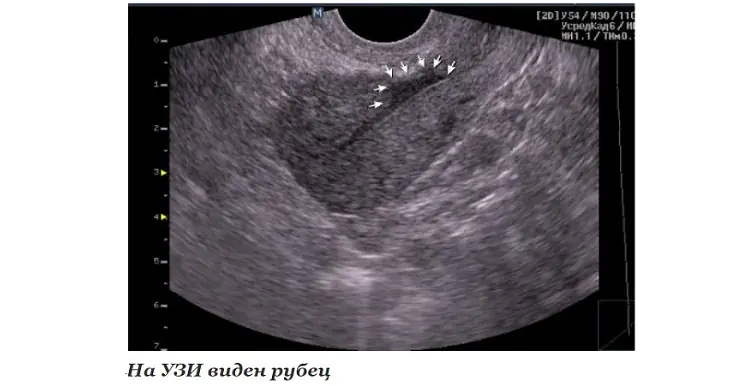
Some people with a suffocating cough go to a therapist, who prescribes a comprehensive examination. Studies in the form of ultrasound or electrocardiography reveal cardiosclerosis.
The disease requires treatment, which is carried out after identifying the main cause of the disorders.
Why is pathology dangerous?
A scar on the heart after a heart attack is dangerous for the development of serious complications. The consequences depend on the amount of connective tissue in the myocardium. Based on this, cardiosclerosis is divided into the following forms:
- diffuse. In this case, the walls of the heart muscle thicken evenly, and pinpoint foci of connective tissue appear on them. Large scars do not appear in this case;
- large-focal. This is the most dangerous form of cardiosclerosis. With it, large affected areas are replaced by fibrous tissue, which loses its ability to contract. This is accompanied by disorders leading to the death of the patient;
- small-focal. With such a diagnosis, you can count on a favorable prognosis if the treatment is carried out on time and correctly. The disease develops after microinfarctions. After an attack, one small scar is formed that does not affect the functions of the organ.
If the scar is small, then a person may not even notice its appearance. The problem is discovered during a routine examination. It is advisable to make the diagnosis at an early stage, before the scar has yet hardened and can be eliminated.
What to do if a scar is found
There are certain symptoms that indicate the presence of cardiosclerosis. With pathology, the patient complains of:
- shortness of breath;
- rapid heartbeat;
- increased fatigue;
- coldness and numbness of the extremities;
- swelling of the face;
- decreased performance. Physical activity is very difficult to bear;
- blue skin on fingertips.
If there are scars on the heart, a person will notice paroxysmal pain in the chest, paleness of the skin due to insufficient blood supply to the tissues due to decreased functionality of the heart.
If a scar is discovered, you need to visit a cardiologist and undergo additional examinations. This will allow you to identify or exclude concomitant diseases. Cardiosclerosis rarely develops independently. This is usually a consequence of other pathologies.
During the examination, the condition of the blood vessels will be assessed and the number of areas of damage will be determined. If blood clots and cholesterol plaques are detected, medications will be prescribed to thin the blood, speed up metabolism and lower blood pressure.
It is possible to stop the necrosis of heart tissue, but it is impossible to reverse the changes that have occurred. Therefore, the patient will have to be examined every six months in order to notice a deterioration in time.
Treatment is aimed at stopping the development of the pathological process.
Therapy
The scar caused by myocardial infarction is treated comprehensively. First, medications are prescribed to restore heart function, improve blood circulation, and speed up metabolism. Medicines are selected individually.
It is difficult to say exactly when scarring begins after a heart attack. This is a long process that can be stopped with timely diagnosis.
In severe cases, surgery cannot be avoided. In this case, a pacemaker or cardioverter-defibrillator is installed to maintain normal cardiac conduction and rhythm. For cardiosclerosis, they can also do:
- Living heart transplantation. The operation is expensive and is performed up to 65 years of age in the absence of serious diseases of the internal organs. A heart transplant carries a high risk that the donor's heart will not survive.
- Shunting. The lumen of narrowed coronary arteries is widened using shunts. The procedure is performed for atherosclerosis.
- Removal of the aneurysm. It most often forms in the area of the left ventricle, its posterior wall. During treatment, the bulging portion of the heart muscle is excised.
The scar remains after surgical treatment, but compared to fibrosis, it does not pose a health hazard.

Medicine has made great strides in treating pathology. Thus, today stem cells are used to eliminate post-infarction scars. The problem can be successfully solved if you apply this technique a week after a heart attack.
Stem cells help replace damaged cells and successfully eliminate cardiosclerotic changes.
Thanks to the introduction of stem cells, it is possible to replace the scar with primary cardiac muscle cells called cardiomyoblasts. This partially or completely restores the contractility of the heart.
Timely stem cell therapy will allow:
- restore vascular tissue naturally;
- cleanse the vessels of deposits and expand their lumen;
- increase vascular elasticity;
- improve blood flow to all organs and tissues.
This technique allows you to develop a network of collateral vessels. They will increase the filling of the heart with blood and eliminate the signs of a heart attack. New strong and healthy vessels will saturate the heart with the components necessary for normal functioning.
To restore myocardial function, the patient must also eat properly, mainly plant foods, give up bad habits, take all medications prescribed by the doctor and undergo regular examinations. This will avoid worsening the situation and developing complications.
When a person develops a myocardial infarction, blood flow in one or more coronary vessels is disrupted. This leads to an imbalance between the need of myocardiocytes for oxygen and its supply. Changes in metabolism due to lack of nutrients aggravate the condition of the affected tissue. As a result, cardiac muscle cells begin to necrotize and die. In place of the dead tissue, a scar forms. In this article I want to talk about the mechanism and possible consequences of such a “replacement”.
Development mechanism
At the time of development of an acute infarction, a sharp disruption of the blood supply to the myocardium occurs for the following reasons:
- Rupture of an atherosclerotic plaque under the influence of a sharp jump in pressure, increased heart rate and acceleration, and accelerated blood flow through the coronary vessels.
- Blockage of blood vessels due to blood thickening (acceleration of platelet aggregation, activation of the coagulation system, decreased rate of blood clot lysis).
- Spasm of the coronary artery (vasoconstriction).
I often observed patients in whom several factors were identified as the cause of the disease with myocardial damage. In young patients, vasospasm is often the basis of pathological disorders, which is not possible to determine after the start of treatment.
Expert advice
I strongly recommend starting treatment in a hospital immediately after an acute attack, since only in this case is it possible to limit the further spread of necrosis and minimize irreversible changes in the myocardium.
The study of histological samples confirms the destruction of the cardiac myocyte 20 minutes after the development of ischemia. After 2-3 hours of lack of oxygen, their glycogen reserves are depleted, which marks their irreversible death. Replacement of myocarditis with granulation tissue occurs within 1-2 months.
As my practice and the observations of colleagues show, the scar on the heart is finally consolidated after six months from the moment the first symptoms of acute infarction appear and is a section of coarse collagen fibers.
Classification
Heart scars can be classified according to their location and extent of distribution.
They can be located along the coronary vessels:
- Impairment of blood flow in the anterior interventricular artery leads to ischemia with the subsequent appearance of a scar in the area of the septum between the ventricles, involving the papillae and lateral wall, as well as on the anterior surface and apex of the left ventricle.
- The infero-posterior and lateral part is affected when the left circumflex coronary artery is blocked.
- Problems with the blood supply to the myocardium in the right artery results in irreversible changes in the right ventricle and can affect the posterior inferior part of the left ventricle and the septum. But such a violation is extremely rare.
According to the type of distribution, scars can be local (focal), which can be compared to a scar on the body, or diffuse (multiple). Experts call the second option dystrophic changes in the myocardium.
How does a scar manifest itself?
The acute period of a heart attack is characterized by a variety of clinical manifestations. The main symptom is pain, which can be relieved exclusively with narcotic analgesics and can last from an hour to 2-3 days. Then the pain syndrome disappears and the formation of an area of necrosis begins, which takes another 2-3 days. Then comes a period of replacing the affected area with loose connective tissue fibers.
If the correct treatment tactics are used, the following symptoms are noted:
- development of compensatory hypertrophy;
- rhythm disturbance (which often accompanies the acute period) is eliminated;
- tolerance to stress gradually increases.
If a scar that appears on the heart crosses the conduction paths along which the impulse travels, a conduction disorder is recorded, such as a complete or partial blockade.
In the case of successful recovery after a primary small-focal infarction, I did not notice any significant disturbances associated with the functioning of the heart in my patients.
If patients have formed a large scar or many small ones, the following deviations are observed:
- dyspnea;
- increased heart rate;
- the appearance of edema;
- enlargement of the left chambers of the heart;
- pressure fluctuations.
How dangerous is this?
The most dangerous is the development of a scar as a result of large-focal or transmural infarctions, as well as several repeated violations in different basins of the coronary vessels with diffuse multiple lesions.
In the case of a large area of damage or widespread cardiosclerosis, the remaining healthy cells cannot fully compensate for the work of damaged cardiomyocytes. The frequency and strength of contractions increases in order to provide organs and tissues with oxygen and necessary substances.
As a result, tachycardia develops; with its appearance, the load on the heart becomes even greater, which leads to dilatation of the left ventricle and atrium. As it progresses, blood stagnation appears in the right side with the development of heart failure.
I also observed another type of complication: a scar on the heart after a heart attack with extensive and deep damage to all layers of the organ caused the formation of an aneurysm due to the thinning of its wall.
The reasons for the appearance of such a defect are:
- transmural lesion;
- increased blood pressure;
- increased blood pressure inside the ventricle;
- excessive physical activity of the patient, refusal to comply with the regimen.
An aneurysm leads to the rapid development of heart failure, the formation of a parietal thrombus, and pronounced stagnation in the systemic circulation. Often complicated by severe rhythm disturbances leading to death (paroxysmal tachycardia and ventricular fibrillation).
Diagnostics
In order to establish a diagnosis, I conduct a survey and study the medical history (mainly, it includes ischemic heart disease with a history of heart attack). External examination usually reveals increased respiratory rate, weakening of heart sounds during auscultation, the presence of edema, and various rhythm disturbances. I will definitely take a blood pressure measurement.
Then I send you to the following research:
- general and biochemical blood test, coagulogram (will help establish concomitant diseases, cholesterol levels and clotting time);
- EchoCG or ultrasound of the heart helps to establish the presence of localized or diffuse areas of connective tissue, allows you to clarify the location and extent of distribution;
- MRI helps to visualize and reliably assess the affected area;
- scintigraphy is required to determine dysfunctional areas of the myocardium.
With the help of an ECG after a transmural and large-focal infarction, it is possible to clarify where the scar is located on the diseased heart.
It is determined by the presence of a Q wave in different leads, as can be seen in the table.
Localization of post-infarction scar in the left ventricle



