
What is spondylitis, what causes inflammation of the spine? Types of the disease, symptoms and its possible consequences. Features of treatment of the spinal column with purulent inflammation of the vertebrae.
The content of the article:- Reasons for development
- Types of spondylitis
- Main symptoms
- Treatment methods
- Medicines
- Physiotherapy
- Folk remedies
Spondylitis is a rare inflammatory disease of the spine that causes the destruction of individual vertebrae with further impairment of the functionality of the spinal column. Making a diagnosis in the early stages is difficult due to the lack of specific symptoms, so very often the pathology has serious consequences. Characteristic symptoms appear at the stage when two or more vertebrae are already severely deformed. The following describes in detail the possible causes of the disease, classification by type, as well as a list of symptoms, consequences and treatment for long-term progression of the pathology.
Causes of spondylitis development
Spondylitis is not an independent disease, but a symptom and consequence of some other diseases that are not actually related to the spine. Damage to the vertebrae, which is purulent-inflammatory in nature, is, in fact, a complication that can also lead to even more serious consequences, often irreversible.
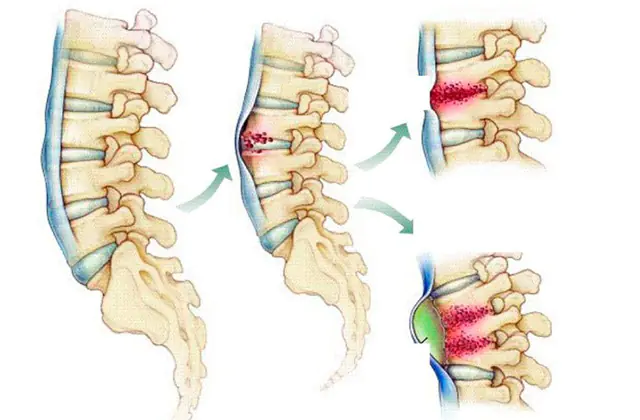
The mechanism of development of the pathology is simple: after the primary lesion, the process of decreasing bone tissue density, disruption of blood microcirculation and infection of tissues begins, followed by disruption of the functionality of the spinal column and the formation of purulent-inflammatory foci.
Reasons for the development of spinal spondylitis:
- Infection with pathogens. Inflammatory processes in the ridge can be triggered by Treponema pallidum, Koch's bacillus, Trichomonas, Brucella, gonorrheal gonococcus, streptococcus, Staphylococcus aureus, as well as pathogens of smallpox, plague, typhus and even various fungal infections. Along with the bloodstream, pathogenic microorganisms penetrate the spine and begin their parasitic activity there. Thus, tuberculosis, syphilis, brucellosis, gonorrhea, typhus, etc. can lead to the development of inflammatory processes in the spinal column.
- Spinal injury. Spondylitis can also occur as a result of various types of back injuries involving soft tissue. As a result of the injury, an inflammatory process develops, and an infection may develop.
- Immunological dysfunction. In some cases, signs of spondylitis arise as a result of increased autoaggression of immune cells that attack their own tissues and thereby cause inflammation. Such a negative reaction can develop after hypothermia or as a result of some infectious disease that affects the functioning of the immune system.
In modern studies devoted to the study of the etiology of inflammatory processes in the ridge, there is evidence that a genetic predisposition may be a provoking factor in the development of this disease. Its marker is the histocompatibility antigen HLA-B27.
Main types of spondylitis
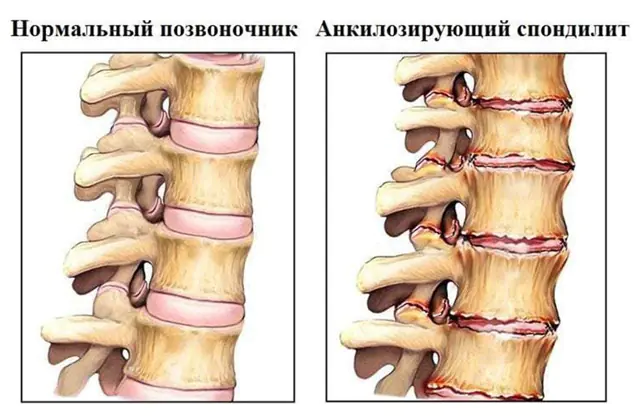
Pictured is ankylosing spondylitis
Spondylitis, to a large extent, is a generalized concept. The need for separation is dictated by the need to prescribe a specific treatment regimen, determined not only on the basis of the individual characteristics of the patient, but also based on the identified causes of the development of this inflammatory process in the spine.
A general classification of spondylitis according to the etiology of its occurrence has been adopted - specific and nonspecific.
Types of specific spondylitis:
- Tuberculosis. Another name is Pott's disease. This is the most common type of disease, when tuberculosis bacilli enter the spongy substance of the vertebrae through the bloodstream. Damage can be caused by back injuries, chronic deformities, and decreased immunity. Tuberculous spondylitis is considered a severe form, because. characterized by damage to a wide area. Causes the formation of cold-type purulent abscesses, i.e. without obvious signs of inflammation, namely without redness and fever. Inflammatory processes occur more often in the thoracic region, less often in the cervical and other regions. As the disease progresses, the vertebrae are destroyed and severely deformed, taking on a wedge shape. In the absence of proper therapy, serious consequences arise - spinal cord damage, ridge fracture, partial or complete irreversible paralysis of the upper limbs, and the formation of a pointed hump. And due to deformation of the chest, problems appear in the functioning of the cardiovascular and respiratory systems.
- Brucellosis. This disease is more common in men, and most often occurs between the ages of 25 and 40 years. Inflammation appears in the lumbar region, with virtually no abscesses occurring. Such a lesion causes thickening around the spine; on x-ray the picture is similar to small-focal destruction of bone tissue. According to the symptoms at the initial stage, spondylitis can be confused with radiculitis.
- Gonorrheal. It is a consequence of gonorrhea. The main symptoms are severe pain and a significant reduction in the mobility of the spinal column.
- Actinomycotic. Occurs with the chronic infectious disease actinomycosis, which provokes the formation of an abscess with fistulas. The thoracic region is most often affected as a result of the spread of infection from previously affected internal organs. The formation of fistulas in lumbar spondylitis is observed as a complication of intestinal actinomycosis.
- Syphilitic. One of the rarest types of this disease. Occurs against the background of syphilis in various organs. It is characterized by the rapid formation of tight mobility of the spine and night pain. Causes the formation of gummas - nodules, irreversible tissue destruction. The progressive course leads to flattening of the vertebral bodies with further damage to the spinal cord and nerve roots, which causes serious neurological disorders.
- Typhoid. Occurs against the background of 2-3 months of typhus development. The disease is accompanied by an increase in temperature and pronounced pain in places where the ridge is affected and multiple ulcers are formed. The progression is rapid. Adjacent vertebrae and the intervertebral disc that holds them together are affected. Bone growths form in the affected area, which quickly block the mobility of the back. The most common localization is the lumbosacral and thoracolumbar joints.
- Aseptic. Occurs against the background of a back injury. Diagnosis is difficult because During the recovery period after injury, the patient notes a noticeable improvement in physical condition. At the same time, pathological changes continue in the vertebrae, and gradually the disease becomes chronic. In this case, against the background of invisible necrosis of bone tissue, various postural disorders develop, for example, stooping, Scheuermann Mau kyphosis.
Nonspecific spondylitis is divided into two types:
- Hematogenous. Otherwise, this type is called spinal osteomyelitis. The causative agent is streptococcal or staphylococcal infection. The disease manifests itself as persistent necrosis of bone tissue with the formation of pus. Fistulas form in the cervical and lumbar regions. The periosteum, spongy substance, as well as bone marrow and surrounding soft tissue are affected. In this case, the patient experiences severe pain. The progression is rapid. Consequences: poor posture, formation of intervertebral hernias.
- Ankylosing. Another name is ankylosing spondylitis. The exact cause of the development of this pathology is unknown. It is generally accepted that ankylosing spondylitis occurs as a result of a malfunctioning immune system that attacks its own cells. The progression is sluggish, often asymptomatic, but constant. Symptoms may include aching pain and mild stiffness. Over time, ossification of cartilaginous tissue occurs, leading to fusion of the vertebrae into a single immovable bone. Possible consequences are severe impairment of motor activity, functioning of internal organs, ventilation of the lungs, as well as compression of nerve roots, blood vessels and soft tissues.
Main symptoms of spondylitis
Aching pain syndrome is the main clinical symptom of spondylitis. The pain can vary in intensity, from mild to severe, but is almost always localized in the area of the affected vertebrae. Some increase in pain occurs after physical exertion or prolonged stay in an uncomfortable position.
Other signs of spondylitis:
- Limited mobility. This symptom occurs at later stages of the disease. At first, difficulties appear with bending and turning the body. Next, the movement of the shoulders and hips is limited.
- Spinal deformity. Physiological curves gradually decrease; over time, the back can noticeably change shape.
- Disruption of internal organs. This is more likely not a symptom, but a consequence of curvature of the ridge and compression of organs. Sensory disturbances, skin numbness, paralysis, and spasms may occur. Sometimes difficulty breathing develops
- General symptoms. Deterioration of general condition, weakness, drowsiness, increased fatigue, fever, chills, local redness and swelling of soft tissues.
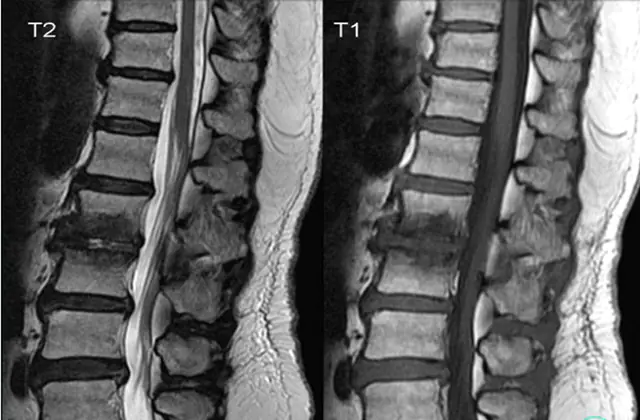
To prevent the progression of inflammatory processes in the spine, it is necessary to go to the hospital when characteristic symptoms appear. The list of necessary diagnostic procedures depends on the suspected type of spondylitis. First of all, biochemical and clinical blood tests, urine tests, and determination of blood sugar levels are indicative. Next, a proteinogram, rheumatic tests, and cytological analysis of the material released from the fistulas can be performed.
Also an integral procedure is the examination of the ridge using an X-ray machine, MRI or ultrasound machine. Next, in accordance with the results obtained, an accurate diagnosis is determined and appropriate treatment is prescribed, which is designed to eliminate the causes of the disease and restore the structure and functionality of the spinal column, as far as possible.
Methods for treating spondylitis
Treatment measures for spondylitis may vary depending on the stage of the disease. Thus, in the acute phase, bed rest is often recommended, during which the patient should be provided with a balanced diet and emotional calm. Corset therapy and some restriction of physical activity may also be prescribed. During this period, it is important to neutralize the inflammatory process and eliminate the root cause of the disease. For this purpose, drug treatment and physical procedures are used. In rare cases, when the condition is severely advanced, surgery is practiced to clear out ulcers or remove irreversibly damaged areas, followed by replacement with a special prosthesis. Let us consider in more detail the most effective methods of treating this pathology.
Medicines for spondylitis
Spondylitis is not an independent disease and occurs as a consequence of some other diseases. That is why the prescribed therapy must be comprehensive to eliminate the causes, symptoms and consequences of disease progression.
Drug treatment can be specific or nonspecific. Specific therapy is prescribed exclusively by the attending physician after diagnosing spondylitis. The selection of drugs is carried out on the basis of a large number of factors - the type of pathogen, the degree of progression of the pathology, the nature of the spinal injury, the presence of concomitant diseases, the individual characteristics of the patient, etc.
Nonspecific therapy uses medications to improve the patient's condition regardless of the etiology of the disease. This treatment option is largely concomitant and does not solve the main problem.

Drug treatment may include the following groups of drugs:
- Antibacterial therapy. Prescribed for spondylitis caused by infectious agents. Sometimes resistance testing may be required to determine the sensitivity of pathogens to a specific active substance. The list of drugs usually includes broad-spectrum antibiotics - cephalosporins and fluoroquinolones. The names of some drugs are Levofloxacin, Ceftriaxone, Ofloxacin, Cefixime, etc.
- Analgesics. Used to reduce the intensity of pain. Can be used without consulting a doctor, but in compliance with the daily dosage recommended by the manufacturer. Such medications only relieve pain and do not solve the underlying problem.
- Nonsteroidal anti-inflammatory drugs. This category of medications is prescribed to reduce the inflammatory process. In this case, there is an antipyretic and analgesic effect. The category is represented by a wide list of drugs - Diclofenac, Voltaren, Ibuprofen, Nimesulide, etc., but the most effective in the treatment of spondylitis are Ortofen and Indomethacin. The course of treatment is usually at least a month, and in some complex cases the treatment even lasts for several years.
- Corticosteroids. Sometimes prescribed in combination with non-steroidal anti-inflammatory drugs, because. help speed up the process of restoring the structure of damaged tissues and healing. They also relieve swelling, eliminate pain and restore metabolism at the cellular level. Most often, doctors prescribe Metypred or Prednisolone. This group of drugs should not be used without prescription, because they have a lot of contraindications and side effects.
- Immunomodulators. They allow you to simulate the functioning of the immune system to help the body cope with infection or suppress autoimmune reactions. The most effective and therefore popular drugs are Thymogen, Interferon, Timalin, Echinacea.
- Muscle relaxants. They relieve muscle spasm and vascular spasm. They have a relaxing effect and relieve some pain.
- Vitamins. B vitamins play a major role in maintaining the body during spondylitis, so they are most often prescribed in the form of injections to quickly obtain an effect. It will also be useful to replenish vitamin C and E reserves, which stimulate tissue regeneration and strengthen immunity.
In addition, in a hospital setting, the patient is given droppers with a solution of sodium chloride, glucose, or Ringer's solution. This procedure helps restore strength and quickly remove toxins and bacteria from the body.
Physiotherapy for the treatment of spondylitis

Physiotherapeutic treatment of spondylitis is often integral, because gives good results and significantly speeds up recovery. However, using it without drug therapy is completely unjustified. The course of treatment usually lasts from 10 to 15 days, but there are exceptions depending on the full clinical picture of the disease. If you are diagnosed with spondylitis, which is often characterized by a long course, additional courses of physical procedures may be required, prescribed after a 2-4 week break.
The most effective options for physiotherapeutic treatment are:
- Physiotherapy. It is carried out from the moment when the disease spondylitis goes into remission. Light physical exercises are aimed at maintaining the muscular frame of the back, allowing you to maintain normal blood circulation and restore metabolic processes. Exercise therapy helps correct posture and improve mobility. The selection of a set of exercises is made individually for each patient.
- Back massage. Allows you to speed up blood circulation, reduce increased muscle tone, and also reduce pain.
- Thermotherapy. Relieves pain, relaxes muscles and improves mobility to some extent.
- Phonophoresis. This procedure is performed with hydrocortisone. It eliminates swelling, slightly reduces inflammation and relieves pain in the affected areas.
- Other procedures. Swimming, various kinds of water procedures, moderate hardening of the body, acupuncture, reflexology, acupuncture, etc. are useful.
All this, in combination with drug treatment, helps to bypass the stage of exacerbation of spondylitis and transfer the disease into remission. Further, during the recovery period, sanatorium-resort treatment with mineral waters and mud therapy is indicated.
Folk remedies for spondylitis
In some cases, when the disease is in its initial stage, it is possible to maintain the body at home using traditional medicine. In general, with such a serious pathology, especially in advanced stages, self-medication is extremely contraindicated. Therefore, before you start using traditional recipes, consult your doctor.
Effective for this inflammatory disease of the spine are various herbal infusions, including lingonberries, chestnut leaves, birch, meadowsweet and linden flowers, parsley root, as well as elderberries, which are brewed and consumed orally.
Of the oils for the treatment of the musculoskeletal system in general and specifically for the diagnosis of spondylitis, coconut, flaxseed, and spruce are considered the most effective. When consumed with food, they help restore cartilage tissue, improve metabolism, relieve painful spasms, and stop or completely prevent destructive processes. Sometimes it is practiced to use a nettle broom. It is pre-steamed and slammed onto the problem area for 30-60 minutes.

Effective folk recipes for spondylitis:
- Cleansing bath with oils. Prepare the base first: add 3-4 drops of essential oils of lemon, sandalwood, cypress, thyme, grapefruit and juniper to 1 tablespoon of sea salt. After 5 minutes, pour in a small amount of warm water, dilute the salt and pour the resulting mass into a bathtub filled with warm water. Take a bath for 10-15 minutes.
- Massage lotion with oils. Commonly used essential oils are black pepper, ginger or marjoram. The selected oil in a few drops is combined with base oil for massage and used to treat problem areas. You can also apply a compress. Such remedies help relieve congestion and stimulate blood circulation well.
- Pain relief cream. It is prepared on the basis of any moisturizing cream, which is enriched with essential oils, for example, chamomile, rosemary, lavender. The ingredients are mixed and applied to areas with severe pain.
- Garlic infusion. Brew 4 cloves of garlic with hot water, leave for 10-15 minutes and drink 100 ml 3 times a day for 7 days. Simply eating this product will also be effective.
- Honey balm. This product helps simulate the functioning of the immune system and speed up recovery processes in the body. Ingredients - honey (100 ml) and crushed aloe leaf (50 g) - boil over low heat for 1 hour, cool. You need to take 1 tbsp. l. 3 times a day.
To prevent the disease from passing into the acute phase, it is necessary to lead a healthy lifestyle, eat right, maintain moderate physical activity, and monitor your posture. By adhering to these simple rules, you can avoid the need for surgery for spondylitis.
Video about spinal destruction - spondylitis and how to treat:



