The main goal of microbiology is the study of living organisms that are not visible to the naked eye. Thanks to this field of science, a person has an understanding of fungi, bacteria, parasites and viruses, how they affect the environment and the human body. Over centuries of experiments and analyses, civilization has learned to use them for economic purposes, for example, for the preparation of fermented milk products, for industrial purposes - for the production of organic acids and alcohols, and for medicinal purposes. Despite this, the form of human interaction with the microscopic world is mutually beneficial. The best example of this is commensalism of the body and its contents - microflora.
In microbiology, extensive research, painstaking scientific work and careful experiments are devoted to the microflora of the human body. They are mainly aimed at studying the composition of certain organs, the influence of microorganisms on tissues, and the conditions for their reproduction. In qualifying works on the normal microflora of the human body, special attention is paid to diseases caused by microbes and the establishment of normal quantities at which they are as harmless as possible.

What it is?
The term “normal” microflora of the human body is most often used to refer to the set of microorganisms that live in a healthy body. Despite the botanical meaning of the word flora, the concept unites all the living creatures of the inner world. It is represented by a variety of bacteria, which are mainly concentrated on the skin and mucous membranes. Their features and action directly depend on their location in the body. And if an imbalance occurs in the microflora of the human body, this is due to a disruption in the functioning of a part of the body. The microscopic component greatly influences the anatomy, physiology, susceptibility to pathogens and morbidity of the host. This is the main role of the microflora of the human body.
The human body, containing about 10 13 cells, normally contains about 10 14 bacteria. Depending on the age stages of a person’s formation, the normal microflora of the body changes, but its components are relatively stable: certain bacteria inhabit the corresponding areas. When functioning normally, microorganisms help the host, but in some cases they pose a threat. Viruses and parasites are not considered members of the normal flora of the human body in microbiology because they are not commensals and do not benefit the host. They are classified as pathogenic microorganisms.
Normal microflora in the human body
Depending on age, health and environment, the normal microflora of the human body varies in definition. To better understand how it works, what causes it, and how it works, most studies are conducted on animals. Its components are microscopic organisms located throughout the body in certain areas. They find themselves in the right environment during the period of gestation and are formed thanks to the mother’s microflora and medications. After birth, bacteria enter the body in breast milk and formula. The microflora of the environment and the human body are also connected, so a favorable environment is the key to the development of normal microflora in a child. It is necessary to take into account the environment, the purity of drinking water, the quality of household and hygiene items, clothing and food. The microflora can be completely different in people leading a sedentary and active lifestyle. She adapts to external factors. For this reason, an entire nation may have some similarities. For example, the microflora of the Japanese contains an increased number of microbes that facilitate fish processing.
Its balance can be disrupted by antibiotics and other chemicals, leading to infections due to the spread of pathogenic bacteria. The microflora of the human body is subject to constant changes and instability, because external conditions change, and so does the body itself over time. In each area of the body it is represented by special species.

Germs spread depending on skin type. Its areas can be compared to regions of the Earth: the forearms with deserts, the scalp with cool forests, the crotch and armpits with jungles. The populations of predominant microorganisms depend on the conditions. Hard-to-reach areas of the body (armpits, crotch and fingers) contain more microorganisms than more exposed areas (legs, arms and torso). Their number also depends on other factors: the amount of moisture, temperature, and the concentration of lipids on the surface of the skin. Typically, the toes, armpits, and vagina are colonized with gram-negative bacteria more often than drier areas.
The microflora of human skin is relatively constant. The survival and reproduction of microorganisms depend partly on the interaction of the skin with the environment and partly on the characteristics of the skin. The specificity is that bacteria adhere better to certain epithelial surfaces. For example, when colonizing the nasal mucosa, staphylococci have an advantage over viridans streptococci, and, conversely, are inferior to them in colonizing the oral cavity.
Most microorganisms live on the surface layers and in the upper parts of the hair follicles. Some are deeper and not at risk from normal disinfection procedures. They are a kind of reservoir for recovery after removal of surface bacteria.
In general, the microflora of human skin is dominated by gram-positive organisms.
- Staphylococcus epidermidis. The most common, making up 90% of the resident aerobic microflora.
- Staphylococcus aureus. The nose and perineum are the most common sites of colonization. Its amount changes with age, being greater in newborns and smaller in adults. It is extremely common (80-100%) in the skin of patients with certain dermatological diseases such as atopic dermatitis. The reason for this phenomenon is still unclear.

Oral cavity
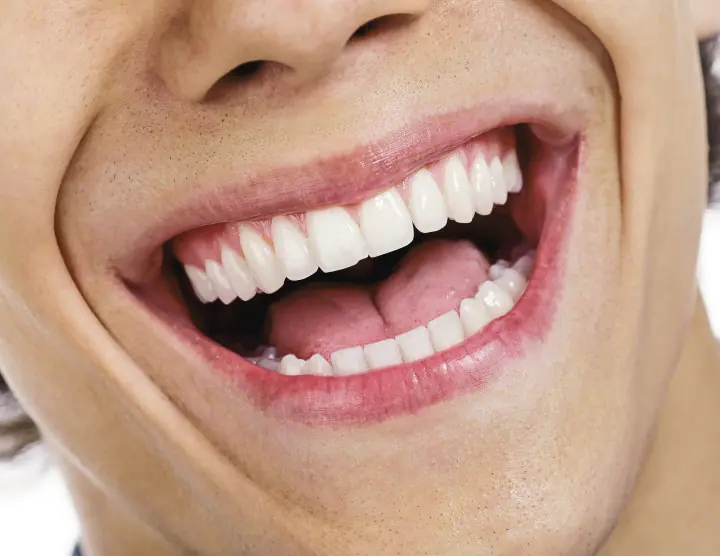
A variety of microbial flora develop here, and streptococcal anaerobes live in the crevices between the gums. The pharynx may be the site of entry and initial spread for Neisseria, Bordetella, and Streptococcus.
Oral flora directly influences dental caries and dental diseases, which affect about 80% of the population in the Western world. Anaerobes in the oral cavity are responsible for many of the brain, facial and lung infections and abscess formation. The airways (small bronchi and alveoli) are usually sterile because particles the size of bacteria do not reach them. In either case, they encounter host defense mechanisms such as alveolar macrophages, which are not found in the pharynx and oral cavity.
Gastrointestinal tract

Intestinal bacteria play an important role in the development of the immune system and are responsible for exogenous pathogenic microorganisms. The flora of the colon consists predominantly of anaerobes, which are involved in the processing of bile acids and vitamin K, and contribute to the production of ammonia in the intestines. They can cause abscesses and peritonitis.
The gastric microflora is often variable, and species populations do not grow due to the adverse effects of acid. Acidity reduces the number of bacteria, which increases after ingestion (103-106 organisms per gram of content) and remains low after digestion. Some types of Helicobacter are still able to inhabit the stomach and cause type B gastritis and peptic ulcers.
Rapid peristalsis and the presence of bile explain the paucity of organisms in the upper gastrointestinal tract. Further, along the small intestine and ileum, bacterial populations begin to increase, and in the area of the ileocecal valve they reach 106-108 organisms per milliliter. In this case, streptococci, lactobacilli, bacteroides and bifidobacteria predominate.
A concentration of 109-111 bacteria per gram of contents can be found in the colon and feces. Their rich flora consists of almost 400 species of microorganisms, 95-99% of which are anaerobes. For example, bacteroides, bifidobacteria, eubacteria, peptostreptococci and clostridia. In the absence of air, they multiply freely, occupy available niches and produce metabolic waste products such as acetic, butyric and lactic acids. Strict anaerobic conditions and bacterial waste are factors that inhibit the growth of other bacteria in the colon.
Although the microflora of the human body can resist pathogens, many of its representatives cause diseases in humans. Anaerobes in the intestinal tract are the primary agents of intra-abdominal abscesses and peritonitis. Intestinal ruptures caused by appendicitis, cancer, heart attack, surgery, or gunshot wounds almost always involve the abdominal cavity and adjacent organs via normal flora. Antibiotic treatment allows some anaerobic species to become dominant and cause problems. For example, Clostridia difficile that remains viable in a patient undergoing antimicrobial therapy can cause pseudomembranous colitis. Other pathological conditions of the intestine or surgery promote bacterial growth in the upper small part of the organ. Thus the disease progresses.
Vagina
Vaginal flora changes as a person ages and is regulated by vaginal pH and hormone levels. Transient microorganisms (eg, candida) often cause vaginitis. Lactobacilli predominate in girls during the first month of life (vaginal pH is approximately 5). Glycogen secretion appears to cease from about the first month before puberty. During this time, diphtheroids, epidermal staphylococci, streptococci and E. coli develop more actively (pH about 7). During puberty, glycogen secretion resumes, pH decreases, and women acquire “adult” flora, which contains more lactobacilli, corynebacteria, peptostreptococci, staphylococci, streptococci and bacteroides. After menopause, the pH rises again, and the composition of the microflora returns to what it was in adolescence.
Eyes
The microflora of the human body is almost absent in the eye area, although there are exceptions. Lysozyme released in tears can interfere with the formation of some bacteria. Research reveals rare staphylococci and streptococci, as well as hemophilus in 25% of samples.
What is the role of normal microflora in the human body?
The microscopic world directly affects the health of the owner. To study its influence, more fundamental research is needed than is currently being done. But the main functions of the microflora of the human body have already been identified: supporting the immune system and assisting in vital processes, such as food processing.
Microorganisms are a source of vitamins and microelements; moreover, they neutralize the effects of weak pathogens and poisons. For example, intestinal flora takes part in the biosynthesis of vitamin K and other products that break down bile acids and produce ammonia. Another role of normal microflora in the human body is to control the host’s appetite. It tells you what the body needs and what to consume to maintain balance. Bifidobacteria need protein foods, E. coli - vegetables and fruits. If a person himself does not know what he wants, this is a clear sign of a general deficiency in the microflora. Frequent changes in diets and eating habits can harm her, although she has the ability to adapt. The environment and the normal microflora of the human body are also closely related.
Common pathologies

Violation of the surface of the mucous membrane often leads to human infection and damage to the normal microflora of the human body. Cavities, periodontal disease, abscesses, foul odors and endocarditis are signs of infection. Deterioration of the host's condition (eg, due to heart failure or leukemia) may cause normal flora to fail to suppress transient pathogens. The microflora of the human body in normal and pathological conditions differs significantly; this is a decisive factor in determining the health of the owner.
Bacteria can cause many different infections of varying severity. For example, Helicobacter pylori is a potential pathogen of the stomach, as it plays a role in the formation of ulcers. Based on the principle of infection, bacteria can be divided into three main groups:
- Primary pathogens. They are causative agents of disorders when isolated from the patient (for example, when the cause of diarrheal disease lies in laboratory isolation and salmonella from feces).
- Opportunistic pathogens. They harm patients who are at risk due to predisposition to disease.
- Non-pathogenic agents (Lactobacillus acidophilus). However, their category may change due to the high adaptability and detrimental effects of modern radiation therapy, chemotherapy and immunotherapy. Some bacteria that were not previously considered pathogens now cause disease. For example, Serratia marcescens is a soil bacterium that causes pneumonia, urinary tract infections, and bacteremia in infected hosts.
A person is forced to live in an environment filled with a variety of microorganisms. Because of the magnitude of the infectious disease problem, the desire of physicians to understand the natural immune mechanisms of the host is well justified. Enormous research efforts are expended to identify and characterize the virulence factors of pathogenic bacteria. The availability of antibiotics and vaccines provides doctors with powerful tools to control or treat many infections. But, unfortunately, these drugs and vaccines have not yet completely eradicated bacterial diseases in humans or animals.
The basis of human health is the normal microflora of the human body, its function is to protect against pathogens and support the host’s immunity. But she herself needs care. There are several tips on how to ensure internal balance in the microflora and avoid troubles.
Prevention and treatment of dysbiosis

To maintain the microflora of the human body, microbiology and medicine advise adhering to the following basic rules:
- Maintain hygiene.
- Lead an active lifestyle and strengthen your body.
- Get vaccinated against infectious diseases and beware of antibiotics. Complications may occur (yeast infections, skin rashes, and allergic reactions)
- Eat right and add probiotics to your diet.
Probiotics are good bacteria in fermented foods and supplements. They strengthen friendly bacteria in the intestines. For relatively healthy people, it is always good to eat natural foods first and supplements second.
Prebiotics are another essential component of food. They are found in whole grains, onions, garlic, asparagus and chicory roots. Regular consumption reduces intestinal irritation and calms allergic reactions.
In addition, nutritionists advise avoiding fatty foods. According to studies conducted on mice, fats can damage the intestinal lining. As a result, unwanted chemicals released by bacteria enter the bloodstream and inflame nearby tissues. Moreover, some fats increase populations of unfriendly microorganisms.
Another useful skill is managing personal experiences and stress. Stress affects the functioning of the immune system - either suppressing or enhancing responses to pathogens. And in general, mental ill-being eventually turns into physical ailments. It is important to learn to identify the origins of problems before they cause irreparable harm to the health of the body.
Internal balance, normal microflora of the human body and the environment is the best that can be ensured for health.
With this publication we continue the series “Lecture notes. To help the student,” which includes the best lecture notes on disciplines studied in humanities universities. The material is brought into accordance with the curriculum of the “Medical Microbiology” course. Using this book in preparation for passing the exam, students will be able to systematize and concretize the knowledge acquired in the process of studying this discipline in an extremely short time; focus your attention on basic concepts, their characteristics and features; formulate an approximate structure (plan) of answers to possible exam questions. This book is not an alternative to textbooks for obtaining fundamental knowledge, but serves as a guide for successfully passing exams.
Table of contents
- Question 1. Fundamentals of microbiology. Classification of microorganisms
- Question 2. Features of the morphology of microorganisms
- Question 3. Optional structural components of a bacterial cell
- Question 4. Nutrition and metabolic features of bacteria
- Question 5. Features of protein and carbohydrate metabolism in bacteria
- Question 6. Growth and reproduction. Genetics of bacteria
- Question 7. Functional units of the genome. Variability of the bacterial cell
- Question 8. Normal microflora of the human body
- Question 9. Normal microflora of the skin and upper respiratory tract
- Question 10. Microbiocenosis of the upper gastrointestinal tract
- Question 11. Microbiocenosis of the middle and lower parts of the gastrointestinal tract
- Question 12. Microbiocenosis of the genitourinary system
- Question 13. Dysbacteriosis
- Question 14. Treatment of dysbiosis
- Question 15. The concept of chemotherapy
- Question 16. Classification of chemotherapy drugs by chemical structure
- Question 17. Classification of antibiotics
- Question 18. The mechanism of action of antibiotics. Complications of antimicrobial therapy
The given introductory fragment of the book Medical microbiology: lecture notes for universities (Alexander Sedov) provided by our book partner - liters company.
Question 9. Normal microflora of the skin and upper respiratory tract
1. Normal skin microflora
Due to constant contact with the external environment leather most often becomes a habitat transient microorganisms. However, there is a stable and well-studied permanent microflora, the composition of which varies in different anatomical zones depending on the oxygen content in the environment surrounding the bacteria (aerobes - anaerobes) and proximity to the mucous membranes (mouth, nose, perianal region), secretion characteristics, and even a person's clothes.
Particularly abundantly populated by microorganisms are those areas of the skin that protected from light and drying:
At the same time, the microorganisms of the skin are affected bactericidal factors of sebaceous and sweat glands.
IN The resident microflora of the skin and mucous membranes contains:
IN composition of the transient:
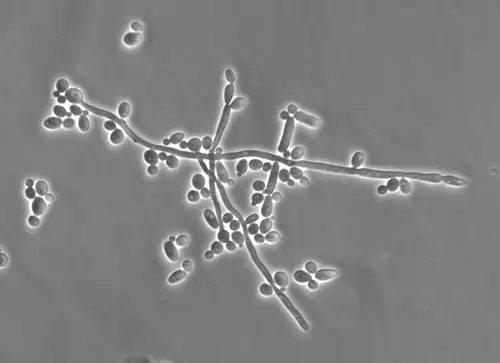
Candida albicans and many others.
In areas where there are accumulations of sebaceous glands (genitals, outer ear), acid-fast non-pathogenic mycobacteria are found. The most stable and at the same time very convenient for study is microflora forehead area.
The vast majority of microorganisms, including pathogenic ones, do not penetrate intact skin and die under the influence of bactericidal properties of skin. Among the factors that can have a significant impact on the removal of non-permanent microorganisms from the surface of the skin are: relate:
• acidic reaction of the environment,
• the presence of fatty acids in the secretions of the sebaceous glands and the presence of lysozyme.
Neither excessive sweating, nor washing or bathing can remove normal permanent microflora or significantly affect its composition, since microflora quickly is being restored due to the release of microorganisms from the sebaceous and sweat glands, even in cases where contact with other areas of the skin or with the external environment is completely stopped. That's why increase in contamination of a particular area of the skin as a result of a decrease in the bactericidal properties of the skin can serve as an indicator reducing the immunological reactivity of the macroorganism.
2. Normal microflora of the eye
IN normal microflora of the eye (conjunctiva) The dominant microorganisms on the mucous membranes of the eye are diphtheroids (coryneform bacteria), Neisseria and gram-negative bacteria, mainly of the genus Moraxella. Staphylococci and streptococci, mycoplasmas are often found. The quantity and composition of the conjunctival microflora is significantly influenced by the tear fluid, which contains lysozyme, which has antibacterial activity.
3. Normal microflora of the ear
Feature of normal ear microflora is that the middle ear normally does not contain microbes, since earwax has bactericidal properties. But they can still enter the middle ear through eustachian tube from the throat. In the external auditory canal there may be skin inhabitants:
• bacteria of the genus Pseudomonas are less common,
• fungi of the genus Candida.
4. Normal microflora of the respiratory tract
For normal microflora of the upper respiratory puThey are characterized by an almost complete absence of microorganisms from the external environment, since most of them linger in the nasal cavity, where they die after some time.
The nose's own microflora is represented by:
May be present as transient species:
Microbiocenosis of the pharynx is even more diverse, since the microflora of the oral cavity and airways mixes here. Representatives of the resident microflora are considered:
Predominant in the upper respiratory tract:
• streptococci and neisseria,
Mucous membrane of the larynx, trachea, bronchi and all underlying sections remains sterile due to the activity of their epithelium, macrophages, as well as the production of secretory immunoglobulin A. The imperfection of these protective mechanisms in premature infants, the disruption of their functioning as a result immunodeficient conditions or during inhalation anesthesia leads to the penetration of microorganisms deep into the bronchial tree and, accordingly, can be one of the causes of severe respiratory diseases.
5. Colonization of newborns by microorganisms
Several hundred species of microorganisms are currently described as part of the normal microflora of the oral cavity and digestive tract. Already during passage through the birth canal, contamination mucous membrane of the child's mouth and pharynx. 4-12 hours after birth, viridans (alpha-hemolytic) streptococci are found in the microflora of the oral cavity, which accompany a person throughout his life. In the child's body they probably enter from the mother's body or from service personnel. To these microorganisms are added already in early childhood:
• gram-negative diplococci (Neisseria),
• sometimes lactic acid bacteria (lactobacillus).
During teething, they settle on the mucous membranes:
More contribute to the rapid formation of normal intestinal microflora earlier breastfeeding and breast-feeding.
Table of contents
- Question 1. Fundamentals of microbiology. Classification of microorganisms
- Question 2. Features of the morphology of microorganisms
- Question 3. Optional structural components of a bacterial cell
- Question 4. Nutrition and metabolic features of bacteria
- Question 5. Features of protein and carbohydrate metabolism in bacteria
- Question 6. Growth and reproduction. Genetics of bacteria
- Question 7. Functional units of the genome. Variability of the bacterial cell
- Question 8. Normal microflora of the human body
- Question 9. Normal microflora of the skin and upper respiratory tract
- Question 10. Microbiocenosis of the upper gastrointestinal tract
- Question 11. Microbiocenosis of the middle and lower parts of the gastrointestinal tract
- Question 12. Microbiocenosis of the genitourinary system
- Question 13. Dysbacteriosis
- Question 14. Treatment of dysbiosis
- Question 15. The concept of chemotherapy
- Question 16. Classification of chemotherapy drugs by chemical structure
- Question 17. Classification of antibiotics
- Question 18. The mechanism of action of antibiotics. Complications of antimicrobial therapy
The given introductory fragment of the book Medical microbiology: lecture notes for universities (Alexander Sedov) provided by our book partner - liters company.
This textbook is intended for students of medical universities, students of medical colleges, as well as applicants. It contains information about the ultrastructure and physiology of bacteria, discusses issues of immunology and virology, describes in detail the structure and morphology of pathogens of various infections, and pays attention to the basics of medical biotechnology and genetic engineering.
Table of contents
- Topic 1. Introduction to microbiology
- Topic 2. Morphology and ultrastructure of bacteria
- Topic 3. Physiology of bacteria
- Topic 4. Genetics of microorganisms. Bacteriophages
- Topic 5. Distribution of microbes in nature and methods of microbiological control of soil, water and air
- Topic 6. Normal microflora of the human body
- Topic 7. Microflora of plant medicinal raw materials and microbiological control of medicines
- Topic 8. Fundamentals of medical biotechnology
- Topic 9. Genetic engineering and its scope in biotechnology
- Topic 10. Antibiotics and chemotherapy
The given introductory fragment of the book Full course in 3 days. Microbiology (Aurika Lukovkina, 2009) provided by our book partner - liters company.
Topic 6. Normal microflora of the human body
1. Normal human microflora
The human body and the microorganisms inhabiting it are a single ecosystem. The surfaces of the skin and mucous membranes of the human body are abundantly populated with bacteria. Moreover, the number of bacteria inhabiting the integumentary tissues (skin, mucous membranes) is many times greater than the number of the host’s own cells. Quantitative fluctuations of bacteria in a biocenosis can reach several orders of magnitude for some bacteria and, nevertheless, fit into accepted standards.
Normal human microflora is a collection of many microbiocenoses characterized by certain relationships and habitat.
In the human body, in accordance with living conditions, biotopes with certain microbiocenoses are formed. Any microbiocenosis is a community of microorganisms that exists as a single whole, connected by food chains and microecology.
Types of normal microflora:
1) resident – constant, characteristic of this species. The number of characteristic species is relatively small and relatively stable, although numerically they are always the most abundantly represented. Resident microflora is found in certain places of the human body, and an important factor is his age;
2) transient – temporarily introduced, not typical for a given biotope; it does not actively reproduce, therefore, although the species composition of transient microorganisms is diverse, they are not numerous. A characteristic feature of this type of microflora is that, as a rule, when it gets on the skin or mucous membranes from the environment, it does not cause diseases and does not live permanently on the surfaces of the human body. It is represented by saprophytic opportunistic microorganisms that live on the skin or mucous membranes for several hours, days or weeks. The presence of transient microflora is determined not only by the supply of microorganisms from the environment, but also by the state of the host’s immune system and the composition of the permanent normal microflora. The composition of transient microflora is not constant and depends on age, external environment, working conditions, diet, past diseases, injuries and stressful situations.
Normal microflora is formed from birth, and at this time its formation is influenced by the microflora of the mother and the hospital environment, and the nature of feeding. The colonization of the body by bacteria continues throughout its life. At the same time, the qualitative and quantitative composition of normal microflora is regulated by complex antagonistic and synergistic relationships between its individual representatives within biocenoses. Microbial contamination is typical for all systems that have contact with the environment. However, normally many tissues and organs of a healthy person are sterile, in particular blood, cerebrospinal fluid, joint fluid, pleural fluid, thoracic duct lymph, internal organs: heart, brain, parenchyma of the liver, kidneys, spleen, uterus, bladder, lung alveoli . Sterility in this case is ensured by nonspecific cellular and humoral immunity factors that prevent the penetration of microbes into these tissues and organs.
On all open surfaces and in all open cavities, a relatively stable microflora is formed, specific to a given organ, biotype or its area.
The highest contamination rates are characterized by:
1) colon. The normal microflora is dominated by anaerobic bacteria (96–99%) (bacteroides, anaerobic lactic acid bacteria, clostridia, anaerobic streptococci, fusobacteria, eubacteria, veillonella), aerobic and facultative anaerobic bacteria (1–4%) (gram-negative coliform bacteria - intestinal coli, enterococci, staphylococci, proteus, pseudomonads, lactobacilli, fungi of the genus Candida, certain types of spirochetes, mycobacteria, mycoplasmas, protozoa and viruses);
2) oral cavity. The normal microflora of different parts of the oral cavity is different and is determined by the biological characteristics of the species living there. Representatives of the oral microflora are divided into three categories:
a) streptococci, neisseria, veillonella;
b) staphylococci, lactobacilli, filamentous bacteria;
c) yeast-like fungi;
3) urinary system. The normal microflora of the external part of the urethra in men and women is represented by corynebacteria, mycobacteria, gram-negative bacteria of fecal origin and non-spore-forming anaerobes (these are peptococci, peptostreptococci, bacteroides). Mycobacteria smegma, staphylococci, mycoplasmas and saprophytic treponemas are localized on the external genitalia of men and women;
4) upper respiratory tract. The native microflora of the nose consists of corynebacteria, neisseria, coagulase-negative staphylococci and α-hemolytic streptococci; S. aureus, E. coli, and β-hemolytic streptococci may be present as transient species. The microflora of the pharynx is more diverse due to the mixing of the microflora of the oral cavity and airways and consists of: neisseria, diphtheroids, α- and β-hemolytic streptococci, enterococci, mycoplasmas, coagulase-negative staphylococci, moraxella, bacteroides, borrelia, treponemes and actinomycetes. Streptococci and Neisseria predominate in the upper respiratory tract; staphylococci, diphtheroids, Haemophilus influenzae, pneumococci, mycoplasmas, and bacteroides are found;
5) leather, especially its hairy part. Due to constant contact with the external environment, the skin is a habitat for transient microorganisms, while having a permanent microflora, the composition of which varies in different anatomical zones and depends on the oxygen content in the environment surrounding the bacteria, as well as on the proximity to the mucous membranes, secretion characteristics and others factors. The composition of the resident microflora of the skin and mucous membranes is characterized by the presence of Staphylococcus epidermidis, S. aureus, Micrococcus spp., Sarcinia spp., Propionibacterium spp., coryneform bacteria. The transient microflora includes: Streptococcus spp., Peptococcus cpp., Bacillus subtilis, Escherichia coli, Enterobacter spp., Acinebacter spp., Moraxella spp., Pseudomonadaceae, Lactobacillus spp., Nocardiodes spp., aspergillus spp., Candida albaicans.
The microorganisms that make up the normal microflora represent a clear morphological structure in the form of a biofilm - a polysaccharide framework consisting of polysaccharides of microbial cells and mucin. It contains microcolonies of normal microflora cells. Biofilm thickness is 0.1–0.5 mm. It contains from several hundred to several thousand microcolonies formed from both anaerobic and aerobic bacteria, the ratio of which in most biocenoses is 10:1–100:1.
The formation of a biofilm provides additional protection for bacteria. Inside a biofilm, bacteria are more resistant to chemical and physical factors.
Factors influencing the state of normal microflora:
a) secretory function of the body;
b) hormonal levels;
c) acid-base state;
2) exogenous: living conditions (climatic, household, environmental).
Stages of formation of normal microflora of the gastrointestinal tract (GIT):
1) accidental contamination of the mucous membrane. Lactobacilli, clostridia, bifidobacteria, micrococci, staphylococci, enterococci, E. coli, etc. enter the gastrointestinal tract;
2) formation of a network of tape bacteria on the surface of the villi. Mostly rod-shaped bacteria are fixed on it, and the process of biofilm formation is constantly underway.
2. Basic functions of normal microflora
Normal microflora is considered as an independent extracorporeal organ with a certain anatomical structure and the following functions.
1. Antagonistic function. Normal microflora provides colonization resistance, i.e., the resistance of the corresponding parts of the body (epitopes) to colonization by random, including pathogenic, microflora. This stability is ensured both by the release of substances that have a bactericidal and bacteriostatic effect, and by the competition of bacteria for nutrient substrates and ecological niches.
2. Immunogenic function. Bacteria, which are representatives of normal microflora, constantly maintain the immune system in proper condition with their antigens.
3. Digestive function. Normal microflora takes part in cavity digestion through its enzymes.
4. Metabolic function. Normal microflora participates in the metabolism of proteins, lipids, urates, oxalates, steroid hormones, and cholesterol through their enzymes.
5. Vitamin-forming function. As is known, in the process of metabolism, individual representatives of normal microflora form vitamins. Thus, bacteria of the large intestine synthesize biotin, riboflavin, pantothenic acid, vitamins K, E, B2, folic acid, which are not absorbed in the large intestine, so you should rely only on those that are formed in small quantities in the ileum.
6. Detoxification function. Normal microflora is capable of neutralizing toxic metabolic products formed in the body or organisms from the external environment through biosorption or transformation into non-toxic compounds.
7. Regulatory function. Normal microflora is involved in the regulation of gas, water-salt metabolism, and maintaining the pH of the environment.
8. Genetic function. Normal microflora in this case is an unlimited bank of genetic material, since the exchange of genetic material constantly occurs both between representatives of the normal microflora themselves and pathogenic species that fall into one or another ecological niche.
At the same time, normal intestinal microflora plays an important role in the conversion of bile pigments and bile acids, absorption of nutrients and their breakdown products. Its representatives produce ammonia and other products that can be adsorbed and participate in the development of hepatic coma.
Dysbacteriosis (dysbiosis) – these are any quantitative or qualitative changes in the normal human microflora typical for a given biotope, resulting from the impact of various unfavorable factors on a macro- or microorganism.
Microbiological indicators of dysbiosis are:
1) reduction in the number of one or more permanent species;
2) loss of certain characteristics by bacteria or acquisition of new ones;
3) increase in the number of transient species;
4) the emergence of new species not typical for a given biotope;
5) weakening of the antagonistic activity of normal microflora.
The causes of dysbacteriosis may be:
1) antibiotic and chemotherapy;
2) severe infections;
3) severe somatic diseases;
5) radiation exposure;
6) toxic factors;
7) vitamin deficiency.
Dysbacteriosis of different biotopes has different clinical manifestations. Intestinal dysbiosis can manifest itself in the form of diarrhea, nonspecific colitis, duodenitis, gastroenteritis, and chronic constipation. Dysbacteriosis of the respiratory system occurs in the form of bronchitis, bronchiolitis, and chronic lung diseases. The main manifestations of oral dysbiosis are gingivitis, stomatitis, and caries. Dysbacteriosis of the reproductive system in women occurs as vaginosis.
Depending on the severity of these manifestations, several phases of dysbacteriosis are distinguished:
1) compensated, when dysbiosis is not accompanied by any clinical manifestations;
2) subcompensated, when local inflammatory changes occur as a result of an imbalance of normal microflora;
3) decompensated, in which the process generalizes with the appearance of metastatic inflammatory foci.
The main method is bacteriological examination. At the same time, quantitative indicators prevail in assessing its results. Species identification is not carried out, but only to the genus.
An additional method is chromatography of the spectrum of fatty acids in the material under study. Each genus has its own spectrum of fatty acids.
1) eliminating the cause that caused the imbalance of normal microflora;
2) the use of eubiotics and probiotics.
Eubiotics – these are preparations containing live bactericinogenic strains of normal microflora (colibacterin, bifidumbacterin, bificol, etc.).
Probiotics – these are substances of non-microbial origin and food products containing additives that stimulate their own normal microflora. Stimulating substances - oligosaccharides, casein hydrolysate, mucin, whey, lactoferin, dietary fiber.
Table of contents
- Topic 1. Introduction to microbiology
- Topic 2. Morphology and ultrastructure of bacteria
- Topic 3. Physiology of bacteria
- Topic 4. Genetics of microorganisms. Bacteriophages
- Topic 5. Distribution of microbes in nature and methods of microbiological control of soil, water and air
- Topic 6. Normal microflora of the human body
- Topic 7. Microflora of plant medicinal raw materials and microbiological control of medicines
- Topic 8. Fundamentals of medical biotechnology
- Topic 9. Genetic engineering and its scope in biotechnology
- Topic 10. Antibiotics and chemotherapy
The given introductory fragment of the book Full course in 3 days. Microbiology (Aurika Lukovkina, 2009) provided by our book partner - liters company.



