Causes and signs of erysipelas. Diagnosis and methods of treatment of the disease: medicinal and folk. Prevention of infection and complications of erysipelas.
The content of the article:- Causes
- Signs of erysipelas development
- Forms and diagnosis
- Treatment methods
- Antibiotics
- Medicines
- External means
- Folk recipes
- Physiotherapy
- Complications
Erysipelas or erysipelas is an infectious disease of soft tissues that quickly spreads to the lymphatic vessels of the skin. Translated from Latin, the name of the disease sounds like “red skin.” Red skin is the main symptom of this disease. Erysipelas is characterized by a protracted course, often becomes chronic and occurs with periodic exacerbations, which often occur in summer and early autumn. Mostly adults, especially women, are affected, but erysipelas also occurs in newborns.
Causes of erysipelas

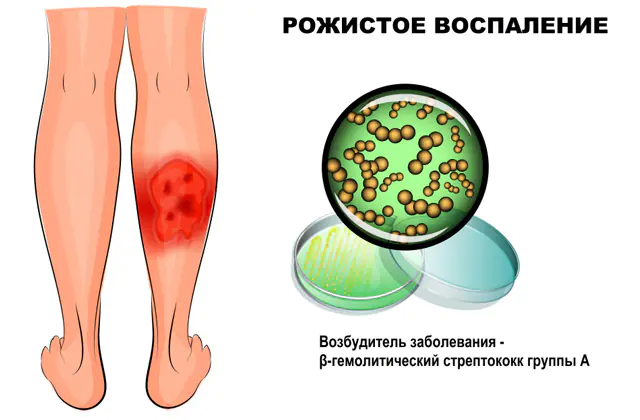
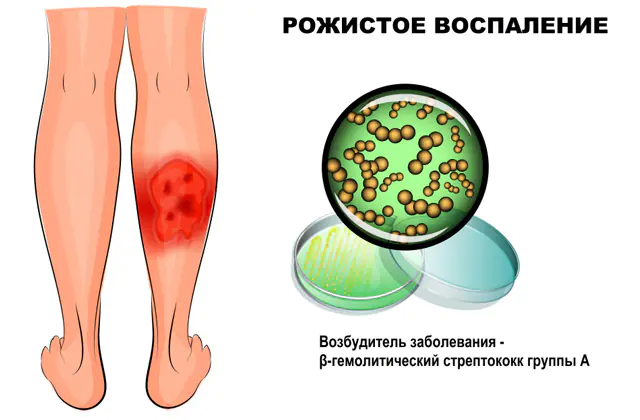
The photo shows erysipelas on the legs
Erysipelas is a disease caused by group A hemolytic streptococcus. This pathogen provokes most purulent infections not only of the skin, but also of other organs. Recently, doctors have discovered that erysipelas can also be caused by other pyogenic microbes (Staphylococcus aureus, Escherichia coli, Proteus). The source of infection is a patient infected with streptococcus.
Streptococcus penetrates the skin in the following ways:
- through microdamages - wounds, abrasions, scrapes, scratching, injections;
- through lymph - through lymphatic vessels from any infected organ;
- through the blood - if the infection causes sepsis (blood poisoning).
Erysipelas is also common, the causes of which are associated with errors during medical procedures, for example, when unsterile instruments are used.
However, not everyone who has been in contact with a person infected with erysipelas develops erysipelas. Some people do not have obvious symptoms of infection, but they are bacteria carriers, that is, the bacterium is constantly released into the external environment, but the person himself has no signs of infection. This situation occurs if the immune system is strong enough. In these cases, in order to survive, streptococcus penetrates the lymph nodes and transforms into the so-called L-form. It does not have a cell wall, so immune cells simply do not recognize streptococcus by sight. The pathogen detects the moment when the body’s defenses weaken, transforms back into bacteria and causes an exacerbation.
What causes erysipelas:
- Chronic streptococcal infections in the body. Tonsillitis (sore throat), rhinitis, pharyngitis, otitis media, dermatitis, pneumonia, inflammation of the eyes, ears, sinusitis, caries are often caused by hemolytic streptococcus.
- Genetic predisposition. Many women have a genetic predisposition to streptococcus.
- Age over 50. In many patients in this age group, immunity decreases, which is a favorable factor for the development of erysipelas.
- Taking hormonal anti-inflammatory drugs (corticosteroids). Hormones tend to sharply inhibit the activity of the body’s defense cells, as a result they have difficulty recognizing pathogenic microbes, including streptococcus.
- Some professions. If a person’s profession involves physical labor, constant friction, dirt and damage to the skin, then the risk of contracting a streptococcal infection is higher.
- Individual susceptibility to streptococcus. Susceptibility to streptococcus is especially high in newborns (premature babies), as well as in people who frequently suffer from infections.
- Poor hygienic conditions. Constant skin contamination reduces local immunity, causes frequent skin infections, which facilitate the work of streptococcus and provoke the appearance of erysipelas.
- Tendency to allergies. An allergic reaction in the body often develops after an infection, while streptococcus successfully disguises itself as the body’s cells, therefore, with frequent infections, the body begins to attack not so much the causative agent of erysipelas, but its own cells, which it mistakes for streptococcus.
- Chronic overstrain of the nervous system. Any overwork, especially chronic, stimulates the adrenal glands; they secrete the stress hormone cortisol, which sharply suppresses the human immune system.
Signs of the development of erysipelas

In the photo there is a mug on the face
After streptococcus penetrates the skin, the process of its reproduction begins. It chooses the lymphatic vessels of the skin as its place of reproduction. The most common variants of erysipelas are erysipelas on the leg (60-70%) and erysipelas on the face (20-30%). Other areas (arms, torso, mammary glands, perineum, genitals) are affected less frequently.
Erysipelas causes the following symptoms:
- Initial signs. The initial local symptoms of the disease include redness, swelling, wetness of the skin, pain, itching, and a feeling of tightness of the skin. All this corresponds to the development of regional lymphangitis. Further, the disease progresses, and a typical erysipelas plaque forms.
- Erysipelas. This element on the skin is a bright red spot with uneven contours resembling flames. The plaque rises above the surface of the skin due to pronounced swelling of the dermis and subcutaneous tissue. There is a marginal ridge between healthy and affected skin. This plaque is warm and dense to the touch. Pressure causes or increases pain. This variant of erysipelas is called erythematous (erythema - redness).
- Bubbles. As the disease progresses, the plaque begins to creep, and the infection enters the blood. At the site of the plaque, blisters form - from small to large. This condition is called the erythematous-bullous form (bulla - bubble). The blisters dry out and become crusty. The fluid inside the bubble may be colorless, cloudy, or bloody.
- Hemorrhages. They occur if, when the bubbles open, small skin vessels and capillaries burst. Hemorrhages from the wound can be small (in the form of dots) or extensive (large bleeding wound surface). If erysipelas is manifested by hemorrhage, it is called erythematous-hemorrhagic (hemorrhage - bleeding).
- General symptoms. The penetration of hemolytic streptococcus toxins into the blood causes general intoxication of the body, and complaints such as fatigue, general weakness, weakness, high body temperature, headaches, dizziness, muscle pain, and chills arise. General symptoms of erysipelas occur before local signs appear.
Erysipelas goes through several stages of inflammation. The initial stage lasts 1-2 days, the height of the disease is 10-20 hours after the first manifestations, and recovery lasts about a week.
Important! The disease lasts 1-2 weeks. After 15 days, local symptoms of erysipelas begin to gradually disappear, but for a long time residual effects such as swelling, thickening of the skin, and age spots may be observed.Forms and diagnosis of erysipelas

Erysipelas has a rather characteristic course, so all its variants are very accurately classified. If an erysipelatous plaque appears in the same place with each exacerbation, then this is a localized (local) form of the disease.
Sometimes it “wanders”, crawls, that is, moves from one area of the skin to another. This form is called common.
If a person simultaneously develops 2 or more erysipelas on different parts of the body, then this is a static version of the infection.
The following forms of erysipelas are distinguished, depending on the frequency of occurrence of infection:
- PrimaryThis is the first time you are infected with an infection. The disease begins from the face or lower extremities.
- Repeated- inflammation in an area of the skin that was not affected during primary erysipelas.
- Recurrent- inflammation subsides, and then arises with renewed vigor, and residual effects always remain after it. In the recurrent form, an allergy to the causative agent of erysipelas occurs in the body. This changes the course of the disease, so the recurrent form is characterized by mild general and local symptoms. A slight decrease in immunity can provoke an exacerbation.
Erysipelas, the symptoms of which are very specific, characteristic, visible to the eye, are diagnosed based on examination, and the diagnosis is confirmed using laboratory tests: a blood test for the streptolysin O titer, an analysis of saliva, blood and the contents of the vesicles for streptococcal secretions (bacterial and L-form) , coagulogram (analysis of the state of blood clotting).
Treatment methods for erysipelas
If erysipelas is diagnosed, treatment is carried out in a hospital or clinic, depending on the severity of the disease. Hospitalization is indicated if there is widespread skin lesions, severe general symptoms develop, frequent exacerbations, if the patient is over 50 years old and under 15. In addition, additional indications are severe concomitant diseases and the need for intravenous medication.
Antibiotics for the treatment of erysipelas
Considering that the cause of the disease is a bacterium, the main method of treatment is drug antibacterial therapy. Antibiotics must be taken for at least 10 days.

Your doctor may prescribe the following antibiotics for erysipelas:
- Benzylpenicillin. Analogues are Procaine, Novocin, Penicillin G. Tablets cost from 30 rubles (on average 22 hryvnia for 30 pieces), and ampoules - from 60 rubles (5-10 hryvnia) per piece.
- Spiramycin. Analogues - Spiramycin-Vero, Spiramisar, Rovamycin. The price for 10 tablets is 164-236 rubles (67-96 hryvnia).
- Azithromycin. Analogs include Azivok, Azitral, Zitrolide, Sumamed. The price for tablets is from 44 rubles (35 hryvnia).
- Roxithromycin. Analogues - Rulid, Elrox, Esparoxi. Tablets cost 170-700 rubles (70-300 hryvnia) for 10 pieces.
- Cefaclor. Analogs are Tsipromed, Floxal, Normax, Okomistin. Price - from 400 rubles (45 hryvnia) per pack of 10 tablets.
Medicines for the treatment of erysipelas
If antibiotics fight the causes of erysipelas, other medications eliminate the consequences of the inflammatory and allergic reaction, and also increase the ability of the immune system to resist infection.
If local signs of an inflammatory reaction are pronounced (severe swelling, redness), the prescription of non-steroidal anti-inflammatory drugs is indicated. The main condition is the absence of gastric and duodenal ulcers, as well as severe pathology of the kidneys and liver, and a tendency to hemorrhage.
For erysipelas, multivitamin preparations containing vitamins B, PP, A and C are necessarily prescribed. They are needed to increase the body's resistance and cell regeneration.

For erysipelas, the doctor usually prescribes the following medications:
- Ibuprofen -anti-inflammatory agent. Analogues are Diclofenac, Ketorol Airtal, Diclak. The price of tablets starts from 40 rubles (16 hryvnia). The course of treatment is 10-15 days.
- Complivit -multivitamin complex. Analogues - Centrum, Supradin. The price of tablets is 280 rubles (205 hryvnia). Course - 2-4 weeks.
- Pentoxyl -immunostimulant. Analogues are Retabolil, Methyluracil. The price of tablets is from 32 rubles.
- Reopoliglyukin —Detoxification treatment. Analogues - glucose solution, saline solution. The price of a solution for intravenous administration is 100-150 rubles (40-62 hryvnia).
External remedies for erysipelas
Local ointments used to treat erysipelas contain antibiotics, antiseptic, anti-inflammatory and wound-healing substances. They should not be used if there are open sores. But it can be used for chronic disease. Local treatment is prescribed for a period of 7 to 14 days.

The following medications can be used for the treatment of erysipelas:
- Erythromycin ointment- antibiotic. An analogue is tetracycline ointment. The price starts from 20 rubles (8 hryvnia).
- Furacilin solution- antiseptic. Analogue - Rivanol. Price - from 45 rubles (13 hryvnia). Used as a bandage when blisters form.
- Balm Vishnevsky- has anti-inflammatory and immunostimulating effects. Can be used after the blisters have dried. Analogs are ichthyol ointment, Solcoseryl. Packaging costs 30-40 rubles (6-7 hryvnia).
- Methyluracil ointment. There are no exact analogues. There are drugs with a similar effect (d-panthenol). Price - 44 rubles (18 hryvnia).
- Indomethacin ointment- has an anti-inflammatory effect. Analogues - Dicloran, Voltaren. Price - from 32 rubles (12 hryvnia).
Folk recipes against erysipelas

Traditional medicine suggests using topical treatments for erysipelas. You can use plantain leaves, lubricate the affected area with pork fat and propolis.
The following folk recipes have proven themselves well as a local treatment for erysipelas:
- Take 1 tablespoon each of sage leaves and chalk (in powder form). Mix them, then pour them onto a cloth (preferably cotton) and place it on the affected part.
- If an erysipelatous plaque appears on the face, then take clean chalk and rice starch, which need to be crushed. The resulting mixture is sifted on the wound. You can also sprinkle the sore spot with flour and bandage it.
- You need to take 2 tablespoons of dope (seeds), pour 250 ml of boiled water over them. Leave to brew for 30 minutes. Strain the resulting infusion and dilute with water so that the proportions are 1:1. This solution should be used to apply lotions on the affected part.
Physiotherapy for the treatment of erysipelas

Physiotherapeutic treatment of erysipelas is prescribed both during the acute period of the disease and after the symptoms subside. This therapy is especially indicated for recurrent illness. Physiotherapy is usually combined with local treatment. The effect is anti-inflammatory, wound healing and immunostimulating effect.
For erysipelas, the following types of physiotherapy can be used:
- Ural Federal District- ultraviolet irradiation is prescribed in the acute period. Local lymph nodes are irradiated.
- UHF- indicated for recurrent erysipelas, helps relieve residual effects.
- Laser therapy- effective for hemorrhage.
- Cryotherapy- freezing the affected area, which eliminates redness.
- Applications- use paraffin (on the face), naphthalan (on the shins), ozokerite.
- Electrophoresis- in a similar way, deep penetration of treatment drugs (lidase, calcium chloride) is achieved.
Complications of erysipelas

In less than 5% of cases, erysipelas may become complicated. The causes of complications may be a weakening of the body's defenses, the spread of infection, infection with other microbes that aggravate the course of the disease, as well as late consultation with a doctor for treatment.
Erysipelas can cause the following complications:
- Local- ulcers, abscesses (ulcers), phlegmon (subcutaneous unlimited purulent process);
- Thrombophlebitis- inflammation of the veins with the formation of blood clots in them;
- Lymphostasis- lymph stagnation, which occurs if there is an erysipelas on the leg, while the accumulated lymph (colorless tissue fluid containing immune cells) increases the volume of the affected limb and “elephantiasis” develops;
- Sepsis- develops if the immune system is weak, and the pathogen easily penetrates into the blood;
- Glomerulonephritis- this is an immune inflammation of the kidneys that develops if the body becomes too sensitive to streptococcus;
- Meningitis- inflammation of the meninges, which is observed mainly if erysipelas affects the soft tissues of the face;
- Cardiovascular failure- with erysipelas, inflammation of the heart muscle and valves may occur against the background of general intoxication of the body;
- Pulmonary embolism - this is a blockage of the branches of the pulmonary artery by a venous thrombus, which forms in the veins of the inflamed lower extremities when blood circulation is impaired.
Video about erysipelas - causes and treatment: