Thermal burns are a common, but nevertheless dangerous situation that requires emergency measures. Of course, children most often suffer from burns - they spill boiling water on themselves, reach into a hot frying pan or oven with their hands, and get burned by tasting too hot food without parental supervision. Young children (no older than 3 years) most often experience burns from boiling water. A very common situation is when a child simply pulls off a pot of hot water and spills it on himself, while the lesion is very extensive, involving the skin of the chest, arms, abdomen, and sometimes the face and neck.
Much more severe burns occur when a child is immersed in water that is too hot for him. Parents often forget that the sensitivity of their skin and the skin of the baby differs significantly - after testing the water in the bath with one finger, they carelessly lower the child into it - as a result, the legs, thighs, calves, buttocks, and the entire lower part of the body as a whole are burned.
Burns that occur in older children are usually the result of playing with fire or improvised explosive devices. In this case, the flame usually affects the skin of the face, eyelids, nose, cheeks, chest, shoulders, and especially the hands. Burns of this type are characterized by seasonality - the largest number of them occur in the summer or spring, during the burning of dry grass and brushwood; cooking barbecue, etc.
Symptoms of a burn depend on the temperature of the agent acting on the skin, the duration of action and, in fact, the thickness of the skin in this area. So, if the skin temperature reaches 45 degrees, a painful reddened area appears on it - erythema. This corresponds to a first degree burn. As soon as the temperature rises to 55 degrees, a second (most often) degree burn occurs, and when the temperature rises above 60 degrees, the coagulation of skin proteins and its necrosis begins. Higher temperatures cause the fabric to char.
Depending on the depth of skin damage and the presence of certain clinical symptoms, all burns are usually divided into 4 degrees:

A first-degree burn is characterized by damage to only the uppermost layers of the epidermis. Clinically, this is manifested by persistent hyperemia, subsequently by erythema and swelling. A first-degree burn, although not particularly deep, is very painful - it is characterized by severe, almost unabated pain, which is only partially relieved by conventional analgesics. Healing of such a burn occurs within a week, no scar formation is observed.

The second degree of burn involves damage to the skin only to the deep layers of the epidermis - it peels off, and a bubble is formed filled with transparent or cloudy contents.

A third degree burn is divided into two more “subgrades”, depending on the depth of the injury: 3A and 3B. A 3A burn is characterized by only damage to the epidermis. Such burns take a much longer time to heal, but after complete epithelization of the surface, there may again be no scars. Degree 3B: here the epidermis is already damaged to a significant depth, including the germinal layer, so healing without a scar is impossible. A large bubble forms, the skin underneath is whitish. Epithalization for degree 3B burns occurs from the edges of the wound, as a result of which it lasts quite a long time.

A fourth degree burn is much more dangerous because... in this case, not only the skin can be affected, but also other tissues underlying it - muscles, tendons and bones. A fourth-degree burn looks like this: the skin is dry, with multiple areas of necrosis on its surface. It can be seen that it is affected down to the subcutaneous adipose tissue, in some cases to the muscles or bones. There is usually no pain with such deep burns, because... in fact, there is nothing to hurt - all the sensitive endings have burned out. Such a burn takes an extremely long time to heal and often requires plastic surgery with areas of skin from healthy areas. But, in any case, the result will be the same - the formation of extensive scars.
Unfortunately, it is not possible to immediately assess the size of the burned area, because It is difficult to say exactly which tissues, currently in a state of ischemia, will undergo necrosis and which will not. The area of the burn is traditionally assessed using the “rule of nines”, but in young children the body in relation to the limbs and head is not developed in the same proportions as in adults, so when determining the area of the burn they need to use either special tables, or simply compare the area of the hand a child with 1% of his body area.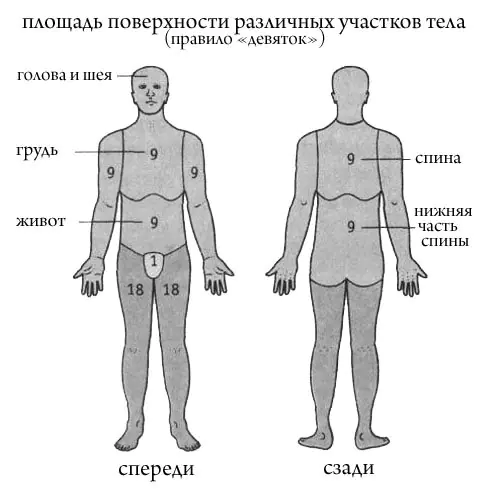
First aid for burns should be provided immediately. The very first thing to do is to stop the effect of high temperature on the skin, i.e. extinguish a flame, pull a person out of a hot liquid, etc. Then you need to cool the affected area. This can be done by removing clothes and placing the limb under running cold water, or by applying (through a clean, dry cloth) pieces of ice or snow to it for 20-30 minutes. If the clothes cannot be removed, then you cannot forcibly pull them off! This can lead to damage to the remaining living epidermis, pain and long, poorly healing wounds later.
Do not lubricate the burn surface with any oil or grease! This should not be done under any circumstances. Fat is an excellent environment and source of nutrition for microbes. After cooling the burn surface, it must be covered with a sterile (or at least clean) cloth to avoid contamination, and then the victim must be taken to any medical facility nearby: central district hospital, first aid station, city hospital; or simply call an ambulance. Treatment of burns in a hospital setting is always complex and is carried out in burn centers or in specialized departments.
Timely (and, of course, correct) assistance provided for a burn is a guarantee that the depth of skin damage will be minimal and the victim will quickly return to normal.
This idea about the discrepancy between the real meaning of companionship and the name “partnership” came to my mind at a meeting of our SNT. Further
So, almost six years have passed since the project was published. Have you given up on the idea? Who is implementing it now? Further
In our country, this holiday was renamed and lost its meaning. However, it is celebrated in 141 countries around the world. Further
Can digital thermometers serve as standards? How to normalize their error in the verification scheme? Further
In fact, consuming peppers is a form of sensation seeking, feeding our brain's desire for stimulation. This is what makes humans different from mammals. Further
Among the electric heaters that we use in everyday life, infrared heaters are now becoming the most popular. They are advertised very widely on the Internet and in newspapers. They are said to be much more efficient than oil radiators and fan heaters. They consume less energy, do not burn oxygen, etc. The main thing is that they are not harmful at all and do not have any negative effects on the human body. Further
One of my friends refuses to eat food that someone has heated in the microwave. It's all because of horror stories on the Internet. Further
This is true, although it sounds incredible, because during the freezing process, preheated water must pass the temperature of cold water. The paradox is known in the world as the “Mpemba Effect”. Further
When cooking raw meat, especially poultry, fish and eggs, remember that only heating to the proper temperature will kill harmful bacteria. Further
451 degrees Fahrenheit. This is the title of the famous book by Ray Bradbury. In the original language it reads like this: ‘Fahrenheit 451: The Temperature at which Book Paper Catches Fire, and Burns’. Do books really start to burn at this temperature? Further
Hot water in an apartment or house is no longer a luxury, but a common necessity. In our new apartment building, the hot water is sometimes not hot at all, but warm, which causes fair indignation among the residents and complaints to the Management Company. Hot water is more expensive, so it is more profitable for us to dilute it with cheaper cold water to obtain the same final temperature. But is it only worth fighting for economic gain? Let's figure out what the tap water temperature standards are based on.
The laws of many countries, including ours, establish safety standards for various services, including hot tap water.
The two main factors influencing the choice of water temperature are: bacterial growth and possible burns. These two factors act in opposite directions. On the one hand, the water temperature should be such that harmful bacteria are killed, on the other hand, the temperature of hot water should not lead to burns (especially in children's institutions and hospitals).
One of the most dangerous bacteria is Legionella. Legionella (Legionella bacteria) Is a gram-negative rod measuring up to 3 microns. The natural habitat of the bacterium is fresh, warm water.
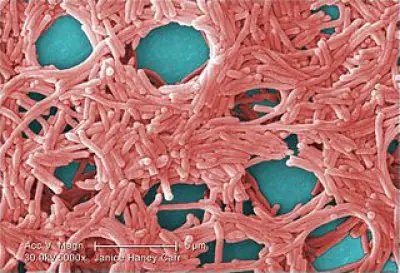
Very often, these bacteria are bred in air conditioning, heating, and humidification systems. Legionellosis is a disease of large cities in industrialized countries. The disease is very serious, leading to complications. An outbreak of Legionella pneumonia was recorded in the Middle Urals in July 2007 in Verkhnyaya Pyshma. The infection entered the apartments through the hot water supply system due to violation of the requirements for flushing pipes and draining water. More than 160 townspeople ended up in hospitals, 5 people died. Also, an outbreak of Legionella pneumonia was recorded between November 22, 2011 and May 22, 2012 among tourists vacationing at the Calp Hotel in Spain; 23 cases of Legionnaires' disease were recorded, 4 of which were fatal.
Effect of temperature on legionella bacteria
70°C – 80°C Disinfection area
66°C Legionella kills in 2 minutes
60°C Legionella kills in 32 minutes
55°C Legionella dies in 5-6 hours
20°C - 45°C Legionella multiplies rapidly
20°C and below Legionella does not reproduce
Based on the data presented, to neutralize water, it should be heated to a high temperature. However, tap water temperatures exceeding 50 °C can be obtained skin surface burns. At temperatures above 70 °C, a deep burn occurs.
Effect of water temperature on skin
65°C partial skin burn in 2 seconds
60°C partial skin burn in 5 seconds.
55°C partial skin burn in 15 seconds.
50°C partial skin burn in 90 seconds.
Thus, in tanks for heating and storing hot water, the temperature must be high in order to neutralize the water. At the same time, water should not be supplied to the consumer very hot, in order to prevent skin burns in case of accidental shutdown of cold water. The standards that are established for places of mass consumption of water (hotels, schools, hospitals, etc.) are approximately the following: shower 41°C, washbasin 41°C, bath 44°C. To ensure this, special thermostatic mixers are used. It should be noted, however, that most cases of legionellosis infection were observed in people who stayed in hotels.
Another option is not to use faucets, but to mix the water flowing from two taps (cold and hot) in the sink or bathtub. In this case, you can supply very hot water to the tap. Such systems can often be seen in English houses.

As a rule, in Russia, very high temperature water is supplied to residential buildings with a centralized water supply. But it is not uncommon, especially in new homes, for water pressure and temperature to decrease, which can certainly lead to the development of harmful bacteria in the pipes. Therefore, the problem with the temperature of hot water in our (and in other) houses is a serious problem that is associated not only with overpayments for housing and communal services, but also with the health of the residents of the house.
Articles similar in topic:
Burn (thermal)- local (local) damage to tissues when their temperature increases to 45–50 ° C and higher as a result of the action of flame, hot liquids, steam, heated solids.
There are four degrees of burns based on the depth of tissue damage:
1st degree - redness of the skin (erythema);
2nd degree - formation of bubbles;
FOR degree — partial or complete necrosis of the Malpighian (germ) layer of the skin;
ZB degree - complete necrosis of the skin throughout its thickness;
4th degree - necrosis of the skin and underlying tissues.
The mechanism of burns is associated with the development of an inflammatory reaction at the site of action of the thermal agent and coagulation of proteins, leading to cell death and tissue necrosis.
Burn disease- functional disorders of internal organs and systems caused by extensive (more than 10–15% of the body surface) and deep burns.
There are four periods of development of burn disease:
1. Burn shock - for extensive and deep burns, more than 15% of the body surface, and in children and elderly people - even for smaller areas. In the first 12–36 hours, capillary permeability sharply increases in the burn area, which leads to a significant release of fluid from the vessels into the tissue. At the site of injury, a large amount of edematous fluid evaporates, and the volume of circulating blood decreases. Leading pathogenetic factors: hypovolemia, pain irritation and increased vascular permeability.
2. General toxemia— develops as a result of autointoxication with tissue breakdown products at the burn site (denatured protein, biologically active amines, polypeptides, etc.) and the production of specific burn autoantibodies (burn autoantigens specific to this type of injury are detected in the skin);
3. Septicotoxemia(attachment of infection);
4. Convalescence(recovery).
Overheating (hyperthermia)- temporary increase in body temperature due to the accumulation of excess heat (with difficulty in heat transfer processes and the effect of high ambient temperatures).
Reasons for the development of overheating:
· environmental factors:
- high ambient temperature (at an ambient temperature of about 33°C, heat transfer from the surface of the body due to convection and thermal radiation stops; at higher temperatures, heat transfer is possible only due to the evaporation of sweat from the surface of the skin);
— high humidity (overheating may develop already at 33–34°C due to the cessation of sweat separation or evaporation);
- water deficiency in the body and due to its loss through sweat;
· the presence of agents that interfere with the implementation of the body’s heat transfer mechanisms;
· separation of oxidation and phosphorylation processes in mitochondria.
An increase in body temperature is accompanied by:
· a sharp increase in respiratory movements (irritation of the respiratory center with heated blood), thermal shortness of breath develops;
Increased heart rate and increased blood pressure;
· due to water loss through increased sweating, blood thickening occurs, electrolyte metabolism is disrupted, and hemolysis of red blood cells increases;
· damage to various tissues leads to the accumulation of toxic products of their breakdown;
· due to the destruction of VII, VIII, X and other plasma factors, blood clotting is impaired.
Overstrain of the thermoregulatory mechanisms leads to their exhaustion, followed by inhibition of the functions of the central nervous system, respiratory depression, cardiac function, decreased blood pressure and, as a consequence, deep hypoxia.
Heatstroke - acute overheating of the body with a rapid increase in body temperature or prolonged exposure to high ambient temperatures.
Death from heat stroke occurs from paralysis of the respiratory center.
The effect of low temperature can cause hypothermia, frostbite and, in case of chronic cold injury, cold neurovasculitis.
Hypothermia.Decrease in rectal temperature below 35°C.
The following phases are distinguished in pathogenesis
1. Compensation. Reactions are aimed at limiting heat transfer: reflex vasospasm, decreased sweating, slowed breathing. Increased heat production: muscle tremors (chills), increased glycogenolysis processes in the liver and muscles, increased blood glucose levels, increased basal metabolism.
2. Decompensation. With prolonged exposure to low temperatures. Body temperature decreases, muscle tremors stop, oxygen consumption and the intensity of metabolic processes decrease, and peripheral blood vessels dilate. As a result of inhibition of the functions of the cerebral cortex and inhibition of the subcortical and bulbar centers, blood pressure decreases, the heart rate slows down, and the frequency of respiratory movements progressively weakens and decreases. All vital functions gradually fade away. Death occurs from paralysis of the respiratory center.
The severity of hypothermia.
· Easy degree: rectal temperature 33–35°C. The skin is pale or moderately bluish, goose bumps, chills, and difficulty speaking appear. The pulse slows to 60–66 beats per minute. Blood pressure is normal or slightly elevated. Breathing is not impaired. Frostbite of I-II degrees is possible.
· Average degree: rectal temperature 31–33°C, characterized by severe drowsiness, depression of consciousness, and a blank look. The skin is pale, bluish, sometimes marbled, and cold to the touch. The pulse slows down to 50–60 beats per minute, weak filling. Blood pressure decreased slightly. Breathing is rare - up to 8-12 per minute, shallow. Frostbite of the face and extremities of I–IV degrees is possible.
· Severe degree: Rectal temperature below 31°C. There is no consciousness, convulsions and vomiting are observed. The skin is pale, bluish, and cold to the touch. The pulse slows down to 36 beats per minute, weak filling, and there is a pronounced decrease in blood pressure. Breathing is rare, shallow - up to 3-4 per minute. Severe and widespread frostbite up to glaciation is observed.
Hibernation - an artificial decrease in body temperature in medical practice, achieved under anesthesia using physical influences, is used to reduce the body's need for oxygen and prevent temporary cerebral ischemia.
Didn't find what you were looking for? Use the search:



