Any surgical intervention is a big test for the patient’s body. This is due to the fact that all his organs and systems experience increased stress, no matter whether the operation is small or large. It especially affects the skin, blood and lymphatic vessels, and if the operation is performed under anesthesia, then the heart. Sometimes, after everything seems to be over, a person is diagnosed with “seroma of the postoperative suture.” Most patients do not know what it is, so many are frightened by unfamiliar terms. In fact, seroma is not as dangerous as, for example, sepsis, although it also does not bring anything good with it. Let's look at how it happens, why it is dangerous and how it should be treated.
What is it - postoperative suture seroma?
We all know that many surgeons perform “miracles” in the operating room, literally bringing a person back from the other world. But, unfortunately, not all doctors conscientiously perform their actions during the operation. There are cases when they forget cotton swabs in the patient’s body and do not fully ensure sterility. As a result, in the operated person, the suture becomes inflamed, begins to fester or separate.
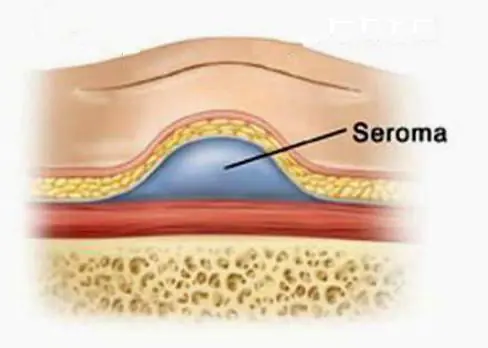
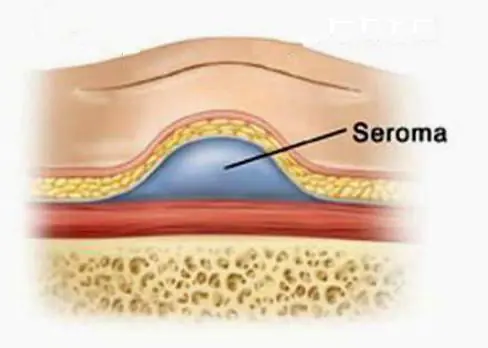
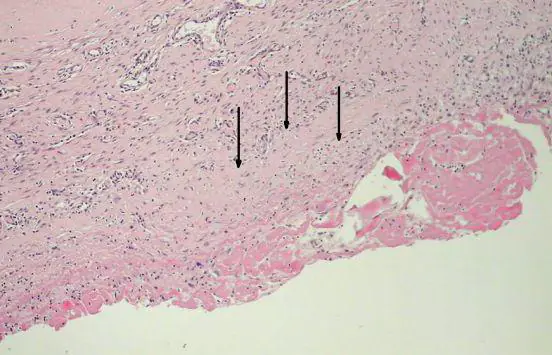
However, there are situations where problems with a stitch have nothing to do with medical negligence. That is, even if 100% sterility is observed during the operation, the patient suddenly accumulates liquid in the incision area that looks like ichor, or pus of a not very thick consistency. In such cases, they speak of seroma of the postoperative suture. What it is, in a nutshell, can be said this way: it is the formation of a cavity in the subcutaneous tissue in which serous effusion accumulates. Its consistency can vary from liquid to viscous, the color is usually straw-yellow, sometimes supplemented with blood streaks.
At-risk groups
Theoretically, seroma can occur after any violation of the integrity of lymph vessels, which do not “know how” to thrombose quickly, as blood vessels do. While they are healing, lymph continues to move through them for some time, flowing from the rupture sites into the resulting cavity. According to the ICD 10 classification system, seroma of the postoperative suture does not have a separate code. It is assigned depending on the type of operation performed and the reason that influenced the development of this complication. In practice, it most often occurs after such cardinal surgical interventions:
- abdominal plastic surgery;
- cesarean section (this postoperative suture seroma has ICD 10 code “O 86.0”, which means suppuration of the postoperative wound and/or infiltration in its area);
- mastectomy.
As you can see, it is mainly women who are at risk, and those who have solid subcutaneous fat deposits. Why is that? Because these deposits, when their integral structure is damaged, tend to peel off from the muscle layer. As a result, subcutaneous cavities are formed, in which fluid begins to collect from the lymph vessels torn during the operation.
The following patients are also at risk:
- those suffering from diabetes;
- elderly people (especially overweight);
- hypertensive patients.
Causes
To better understand what it is - postoperative suture seroma, you need to know why it forms. The main causes do not depend on the competence of the surgeon, but are a consequence of the body’s reaction to surgical intervention. These reasons are:
- Fat deposits. This has already been mentioned, but we will add that in overly obese people whose body fat is 50 mm or more, seroma appears in almost 100% of cases. Therefore, doctors, if the patient has time, recommend liposuction before the main operation.
- Large wound surface area. In such cases, too many lymph vessels are damaged, which, accordingly, release a lot of fluid and take longer to heal.
Increased tissue trauma
It was mentioned above that seroma of the postoperative suture depends little on the conscientiousness of the surgeon. But this complication directly depends on the skills of the surgeon and on the quality of his surgical instruments. The reason why seroma can occur is very simple: the work with the tissues was carried out too traumatically.
What does it mean? An experienced surgeon, when performing an operation, works with damaged tissues delicately, does not squeeze them unnecessarily with tweezers or clamps, does not grab them, does not twist them, and performs the incision quickly, in one precise movement. Of course, such jewelry work largely depends on the quality of the instrument. An inexperienced surgeon can create a so-called vinaigrette effect on the wound surface, which unnecessarily injures the tissue. In such cases, the ICD 10 code for seroma of the postoperative suture can be assigned as follows: “T 80”. This means “a complication of surgery not noted elsewhere in the classification system.”

Excessive electrocoagulation
This is another reason that causes suture gray after surgery and to some extent depends on the competence of the doctor. What is coagulation in medical practice? This is a surgical procedure performed not with a classic scalpel, but with a special coagulator that produces a high-frequency electric current. In essence, this is a targeted cauterization of blood vessels and/or cells by current. Coagulation is most often used in cosmetology. She has also proven herself excellent in surgery. But if it is performed by a physician without experience, he may incorrectly calculate the required amount of current or burn excess tissue. In this case, they undergo necrosis, and neighboring tissues become inflamed with the formation of exudate. In these cases, seroma of the postoperative suture is also assigned the code “T 80” in ICD 10, but in practice such complications are recorded very rarely.
Clinical manifestations of seroma of small sutures
If the surgical intervention was on a small area of skin, and the suture turned out to be small (accordingly, the doctor’s traumatic manipulations affected a small volume of tissue), the seroma, as a rule, does not manifest itself in any way. In medical practice, there are cases where patients did not even suspect it, but such a formation was discovered during instrumental studies. Only in isolated cases does a small seroma cause minor pain.
How to treat it and is it necessary to do it? The decision is made by the attending physician. If he deems it necessary, he may prescribe anti-inflammatory and painkillers. Also, for faster wound healing, the doctor may prescribe a number of physiotherapeutic procedures.

Clinical manifestations of seroma of large sutures
If the surgical intervention affected a large volume of the patient’s tissue or the suture was too large (the wound surface is extensive), the occurrence of seroma in patients is accompanied by a number of unpleasant sensations:
- redness of the skin in the suture area;
- nagging pain that gets worse when standing;
- during operations in the abdominal region, pain in the lower abdomen;
- swelling, bulging of part of the abdomen;
- temperature increase.
In addition, suppuration of both large and small seromas of the postoperative suture may occur. Treatment in such cases is very serious, including surgical intervention.
Diagnostics
We have already discussed why seroma of a postoperative suture can occur and what it is. Treatment methods for seroma, which we will consider below, largely depend on the stage of its development. In order not to start the process, this complication must be detected in time, which is especially important if it does not announce itself in any way. Diagnostics is carried out using the following methods:
Examination by the attending physician. After surgery, the doctor is required to examine his patient's wound daily. If undesirable skin reactions are detected (redness, swelling, suppuration of the suture), palpation is performed. If there is a seroma, the doctor should feel fluctuation (flow of liquid substrate) under the fingers.
Ultrasound. This analysis perfectly shows whether or not there is accumulation of liquid in the seam area.
In rare cases, a puncture is taken from the seroma to clarify the qualitative composition of the exudate and decide on further actions.

Conservative treatment
This type of therapy is most often practiced. In this case, patients are prescribed:
- antibiotics (to prevent possible further suppuration);
- anti-inflammatory medications (they relieve inflammation of the skin around the suture and reduce the amount of fluid released into the resulting subcutaneous cavity).
Nonsteroidal drugs such as Naproxen, Ketoprofen, and Meloxicam are more often prescribed.
In some cases, the doctor may prescribe steroidal anti-inflammatory drugs, such as Kenalog, Diprospan, which block inflammation as much as possible and accelerate healing.
Surgery
According to indications, including the size of the seroma and the nature of its manifestation, surgical treatment may be prescribed. It includes:
1. Punctures. In this case, the doctor removes the contents of the resulting cavity with a syringe. The positive aspects of such manipulations are as follows:
- can be performed on an outpatient basis;
- painlessness of the procedure.
The disadvantage is that the puncture will have to be done more than once, and not even twice, but up to 7 times. In some cases, it is necessary to perform up to 15 punctures before the tissue structure is restored.
2. Installation of drainage. This method is used for seromas that are too large in area. When drainage is placed, patients are simultaneously prescribed antibiotics.

Folk remedies
It is important to know that regardless of the reasons for the seroma of the postoperative suture, this complication is not treated with folk remedies.
But at home, you can perform a number of actions that promote healing of the suture and prevent suppuration. These include:
- lubricating the seam with antiseptic agents that do not contain alcohol (“Fukorcin”, “Betadine”);
- application of ointments (Levosin, Vulnuzan, Kontraktubeks and others);
- inclusion of vitamins in the diet.
If suppuration appears in the suture area, you need to treat it with antiseptic and alcohol-containing agents, for example, iodine. In addition, in these cases, antibiotics and anti-inflammatory drugs are prescribed.
In order to speed up the healing of stitches, traditional medicine recommends making compresses with an alcohol tincture of larkspur. Only the roots of this herb are suitable for its preparation. They are washed well from the soil, crushed in a meat grinder, put in a jar and filled with vodka. The tincture is ready for use after 15 days. For a compress, you need to dilute it with water 1:1 so that the skin does not get burned.
There are many folk remedies for healing wounds and scars after surgery. Among them are sea buckthorn oil, rosehip oil, mumiyo, beeswax, melted with olive oil. These products should be applied to gauze and applied to the scar or seam.
Postoperative suture seroma after cesarean section
Complications in women whose obstetrics were performed by caesarean section are common. One of the reasons for this phenomenon is the mother’s body, weakened by pregnancy, which is unable to ensure rapid regeneration of damaged tissues. In addition to seroma, a ligature fistula or keloid scar may occur, and in the worst case scenario, suppuration of the suture or sepsis. Seroma in women giving birth after a cesarean section is characterized by the fact that a small dense ball with exudate (lymph) inside appears on the suture. The reason for this is damaged blood vessels at the site of the incision. As a rule, it does not cause concern. Seroma of postoperative suture after cesarean does not require treatment.
The only thing a woman can do at home is to treat the scar with rosehip or sea buckthorn oil to speed up its healing.

Complications
Postoperative suture seroma does not always go away on its own and not in everyone. In many cases, without a course of therapy, it can fester. This complication can be provoked by chronic diseases (for example, tonsillitis or sinusitis), in which pathogenic microorganisms penetrate through the lymph vessels into the cavity formed after surgery. And the liquid that collects there is an ideal substrate for their reproduction.
Another unpleasant consequence of seroma, which was not paid attention to, is that the subcutaneous fatty tissue does not fuse with the muscle tissue, that is, the cavity is constantly present. This leads to abnormal skin mobility and tissue deformation. In such cases, repeated surgery must be used.
Prevention
On the part of the medical staff, preventive measures consist of strict adherence to the surgical rules of the operation. Doctors try to perform electrocoagulation more gently and injure less tissue.
On the part of patients, preventive measures should be as follows:
- Do not agree to surgery (unless there is an urgent need) until the thickness of the subcutaneous fat reaches 50 mm or more. This means that you first need to do liposuction, and after 3 months, surgery.
- After surgery, wear high-quality compression stockings.
- Avoid physical activity for at least 3 weeks after surgery.
Bubbles have appeared around the seam, liquid is leaking from them, the seam is getting wet, what should I do?
No. 23 760 Surgeon 08/30/2015
A herniated disc was removed 2 weeks ago. The seam was clean, on the 10th day the stitches were removed, but I was allergic to the eraser. Bandages, adhesive plaster. There was redness on the back. On the 5th day after removing the sutures, bubbles appeared around the suture, liquid flowed out of them, and the suture began to get wet. The seams were treated with chlorhexidine and brilliant green. When the seam began to get wet, the doctor prescribed bandages with levomekol, but it didn’t help.
ANSWERED: 08/30/2015 
18+ Online consultations are for informational purposes only and do not replace a face-to-face consultation with a doctor. Terms of use

Your personal data is securely protected. Payments and site operation are carried out using the secure SSL protocol.
Often, patients who have undergone surgery develop allergies after surgery? What is causing this problem? What symptoms does it accompany? Is it possible to get rid of it?
In fact, an allergic reaction is rarely directly related to surgery. After all, by and large, an allergy is a reaction of the nominal system to a particular substance. Therefore, disorders arise already in the postoperative period. But, of course, there are exceptions.
For example, some patients are allergic to latex, which is what surgical gloves are made from. In addition, an allergic reaction may result from tissue contact with certain metals used in surgical instruments. In addition, the immune system often rejects various implants or prostheses, which is accompanied not only by skin manifestations, but also by weakness, the development of an inflammatory process, suppuration and even sepsis.
But, as a rule, doctors manage to find out about the presence of such a specific form of allergy even before surgery, which makes it possible to select more suitable materials. This is why allergies rarely occur after surgery for the reasons described above.
In most cases, disorders are associated with a period of rehabilitation. It's no secret that after a major operation, patients must undergo a course of treatment with antibacterial agents - this is a reasonable measure of protection against possible infection. On the other hand, antibiotics are precisely those substances that often cause an allergic reaction. It is accompanied by the appearance of spots and rashes on the skin, itching, swelling, burning, peeling, etc.
In addition, antibiotics kill not only pathogenic microbes, but also beneficial intestinal microflora, which affects the functioning of the digestive and immune systems. Dysbacteriosis is usually accompanied by nausea, vomiting, problems with stool, abdominal pain, and accumulation of gases in the intestines. A deficiency of beneficial microorganisms also increases the likelihood of allergies.
In addition, immune system reactions may occur as a result of the use of other medications. For example, during ophthalmological operations, patients are prescribed eye drops, and skin sutures are often recommended to be treated with special ointments - any of these drugs can lead to the appearance of allergy symptoms. Moreover, some patients notice skin reactions even when wearing special compression garments.
In any case, if you have such disorders, you should immediately consult a doctor, preferably an allergist or immunologist.
(Female, 51 years old, Sterlitamak RB, RF)
Hello. Dad had an operation to remove a stone from the adenoma; in a month and a half the adenoma will be operated on. We inserted a tube, 2 weeks have passed since the operation and for a week now there has been severe redness of the skin all over the abdomen, itching and irritation we cannot do anything to remove. Sprinkle with baby powder. Irritation even with adhesive plaster. We fix the bandage with a gauze pad on the stomach, and an elastic bandage on top. Please tell me what can be done to bring the skin back to normal?
Try using ointments that contain steroid hormones (prednisolone, hydracortisone ointments, Flucinar ointment, Fluorocort ointment and many others.
(Guest) Elena 30.07.2013 23:27
Hello! After surgery on the leg (a plate was placed on a fracture of both bones), the leg is red, not the seam, and it burns. Tell me what to do?
(Guest) Elena 16.02.2014 10:36
My husband had surgery on his leg in January, lumps began to appear around the seam and fluid was leaking out, what should I do?
Contact your doctor and rule out osteomyelitis.
(Guest) Boris 03.02.2015 16:32
On the 20th day after surgery (total arthroplasty on the left hip joint), white liquid began to bubble out along the wound. The suture was removed on the 14th day after the operation, the wound was clean and dry, the first treatment was an iodine solution, on the second day, brilliant green, and then on the 20th day, white liquid began to appear in the form of bubbles along the wound itself and a red rash appeared around the wound . There is no fever, no pain in the suture area, general condition is good, I bandage my legs with an elastic bandage, I walk with the help of crutches without pain. Please advise how to eliminate this problem, I will be very grateful...
(Guest) Yuri 17.10.2015 21:59
On October 14, we had surgery to remove an umbilical hernia. Today I noticed redness around the navel. What could this be?
Anything, see your doctor.
(Female, 22 years old, Aleysk, Russia)
Good evening. After a cesarean section, a month later, the brilliant green started to fall off from the seam, I noticed blisters and liquid inside in this place. What could this be?
Zelenka has not been used by reputable establishments for a long time.
See an outpatient surgeon or dermatologist (only those who do not use brilliant green).
(Guest) Natalia 05.11.2016 17:20
CREATE NEW MESSAGE. But you are an unauthorized user.
If you have registered previously, then “log in” (login form in the upper right part of the site). If this is your first time here, please register.
If you register, you will be able to further track responses to your messages and continue the dialogue on interesting topics with other users and consultants. In addition, registration will allow you to conduct private correspondence with consultants and other users of the site.
Register Create a message without registration
Hello! My husband underwent surgery on March 18 - left eversion carotid endarterectomy. On March 25, his stitches were removed, the seam was treated with green paint and he was discharged home. By evening, redness and watery blisters appeared on the skin around the suture. Everything turned red and ran, the redness spread very quickly, the scale of the redness increased. I ran to see a surgeon and he prescribed Flucinar ointment mixed in half with baby cream. The redness gradually began to subside on the 3rd day, we did not touch the seam, it was treated only with furatsilin, and so the redness went away on the 5th day, the bubbles disappeared, but now the seam itself began to get wet and turned red. So my husband is allergic to green stuff, but what should we use to treat the seam? On the Internet they write everywhere: treat with peroxide, then with brilliant green, but we can’t smear it with brilliant green. Tell me, what should we do next?
«>