Symptoms of a heart attack. Treatment after a heart attack
It is possible to save a person who has had a myocardial infarction if doctors begin to restore the artery blocked by a thrombus within an hour and a half. What symptoms of a heart attack should you pay attention to? Which medications will help and which are useless? Cardiologist Anton Rodionov answers questions about this complication of angina.

How are atherosclerotic plaque and myocardial infarction related?
The problem of plaque in the coronary artery is not only a problem of angina. The larger the plaque, the more severe the angina. And if the plaque blocks the vessel by 90%, will there be a heart attack? Will not be. During this time, additional arteries (collaterals) will grow, which will supply blood to the heart.
But why are we then afraid of atherosclerotic plaque? The scary thing is not that it is growing, but that it may be unstable. Psychological stress, smoking, overeating, alcohol, even going out into the cold at the wrong time can cause this plaque to rupture.
The body perceives plaque rupture as injury. Then the universal damage control mechanism kicks in. Platelets form a primary thrombus, which suddenly blocks the blood flow. And the part of the myocardium that is behind the thrombus suddenly loses its blood supply and dies. This is called a heart attack.
At the time of myocardial infarction, a person, as a rule, experiences a sharp chest pain that radiates to the shoulders and neck. Quite often the pain is such that the patient can barely tolerate it. The patient becomes afraid and fears death. Nitroglycerin doesn't help at all.
It is a deep misconception that only heart patients suffer from heart attacks. Nothing of the kind, quite often myocardial infarction develops in completely “healthy” people just yesterday, like a bolt from the blue. Moreover, their prognosis is worse, since, unlike patients with angina, their hearts have not had time to adapt to the constant lack of oxygen and grow the necessary collateral vessels.
How to act in case of a heart attack?
If you have even the slightest thought that a person may be having a heart attack, you should immediately call an ambulance. The most important factor here is time. The faster we can get rid of the blood clot and open the affected artery, the smaller the area of necrosis and the less likely it is to develop heart failure in the future.
While you are waiting for the doctors, the patient should be given chew aspirin: either regular at a dose of 500 mg, or, if you only have low-dose cardiac, then 4 tablets. Do not swallow, but chew it, so that it works faster. For what? We have already said that aspirin prevents platelet aggregation, which means that it is necessary to ensure that at least new groups of platelets do not approach the infarction zone.
While you are waiting for the ambulance, prepare all available medical documents, it will be easier for colleagues to figure out what kind of patient is in front of them.
Don't be lazy meet the brigade. Do you think it’s easy to navigate your courtyards, barriers, entrances, iron doors, codes and intercoms? Time is ticking.
Is it possible to give nitroglycerin? This is a possible option, but, let's say, for experienced users. If we give nitroglycerin to a person with low blood pressure, we can make the situation worse: the pressure will drop even more, and the blood flow to the heart will deteriorate even more. If the patient has previously used nitroglycerin, if he tolerates it normally, if his blood pressure is not less than 120/80 mmHg. Art., then you can give nitroglycerin. However, do not expect much effect from nitroglycerin during a heart attack.
If you suspect a myocardial infarction, then stay where you are and wait for an ambulance. No need to drive, no need to try to get to the clinic or hospital on your own. Each extra load can increase the area of necrosis.
There is no need to think: now I’ll lie down for a while and everything will pass, there is no need to take alcohol “to dilate blood vessels.” Time is working against you.
How to open an artery during myocardial infarction
Then the fate of the patient is in the hands of the emergency doctors and those people who will continue to care for him. The most important task is to open the affected artery as quickly as possible. The faster the artery is opened, the better the prognosis.
There are two options for opening the artery. The first (best) is balloon angioplasty and stenting. A conductor with a balloon is installed into the lumen of the vessel. The balloon is inflated, the plaque is crushed and the vessel is expanded. Then a stent is placed in this place - a special metal structure that will keep the vessel open. The optimal time that should pass from the onset of pain to the installation of a stent is no more than 90 minutes. In large cities this is possible; medical resources make it possible to immediately hospitalize the patient in a hospital where there is a 24-hour coronary service.
The second way to open the artery is to dissolve the blood clot (thrombolysis). However, it is not suitable for all heart attacks. If the hospital is very far away, some ambulance teams can administer a thrombolytic even in the car on the way to the hospital. But again, thrombolysis will only work in the first 12 hours, or better yet, in the first 6 hours.
What treatment is needed after myocardial infarction?
A patient who has suffered a myocardial infarction should be treated in the same way as a patient with angina pectoris, but much more responsibly, since the heart is not infinite: each new heart attack brings us closer to the end of life.
Let's start with medications.
- Aspirin - constantly.
- Clopidogrel or ticagrelor - 1 year after any heart attack
- High dose statins - constantly. The drugs are prescribed regardless of cholesterol levels. The goal here is not to reduce cholesterol, but to stabilize plaques.
- Beta blockers - constantly. In this case, they are prescribed not so much to prevent angina attacks, but to prevent heart failure from developing.
- ACE inhibitors - constantly, especially if there is arterial hypertension.
Position number 2 on this list is one of the few situations in cardiology (you can count them on one hand) when some medicine is prescribed for a course of 1 year. In all remaining cases, all our drugs are taken indefinitely (read: for life), until one of the doctors reasonably cancels them, replaces them with another, etc.

Can there be a heart attack without symptoms?
Happens. There are heart attacks with few symptoms, there are heart attacks with atypical symptoms, and there are heart attacks that are completely painless.
By the way, about atypical symptoms. If you remember anatomy in general terms, then it will not be a discovery for you that the heart in the chest “lies” on the diaphragm. So, quite often, when the lower wall of the left ventricle, the one adjacent to the diaphragm, is damaged, symptoms appear that resemble a disease of the gastrointestinal tract. Sometimes even such patients are taken by ambulance to surgery or infection.
Silent myocardial infarctions often occur in patients with diabetes mellitus. The fact is that with severe diabetes mellitus, the nervous system is naturally affected, and the transmission of pain impulses is disrupted. The patient does not feel pain. But that doesn't make it any easier.
But it often happens that the patient’s ECG shows some changes that can be regarded as a heart attack. And if the patient claims that he did not have an obvious heart attack (i.e., pain attack, hospitalization, resuscitation), then in such a situation it is necessary to do clarifying studies, primarily echocardiography.
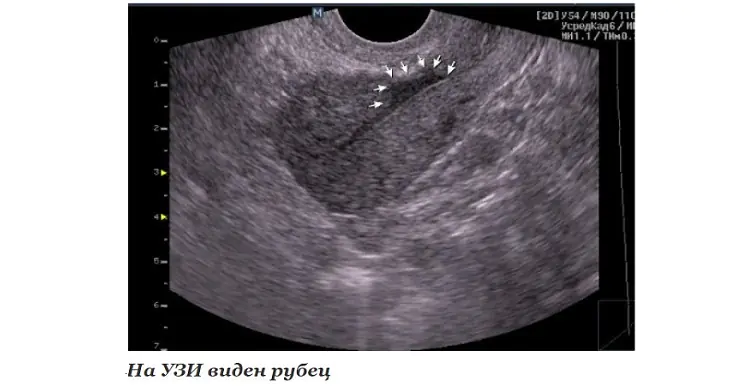
A scar is a section of connective tissue that is usually clearly visible by ultrasound as a section of the heart that does not contract at all or contracts much weaker than the rest of the myocardium.
Can a scar after a heart attack resolve?
Readers of the older generation remember how in the late 80s the main charlatan of the entire USSR, the unforgettable Anatoly Kashpirovsky, gave television “simultaneous game sessions”, and the enthusiastic public reported tens of thousands of letters about cures for all imaginable and inconceivable diseases.
At the same time, grateful viewers also reported “resorption of scars after a heart attack.” In those years, it seems, I had no intention of going to medical school, but the phrase stuck in my memory.
Let's send greetings to TV viewers of the 1980s from the 2010s: the scar cannot resolve, even attempts to treat a heart attack with stem cells in the 21st century have not led to significant success. But the electrocardiographic trace from a heart attack, if it was not very large, can indeed sometimes be “erased.” However, this does not mean that the patient has become healthy again. No, the scar in the heart still remains (it can be seen with ultrasound), and the need for treatment still exists.
What is a microinfarction?
Don't know. In world medicine such a term does not exist. Sometimes “microinfarction” is understood as unstable angina. This is an intermediate condition between myocardial infarction and an acute attack of angina. With unstable angina, a small zone of thrombosis occurs, but the vessel is not completely blocked, blood flow is maintained, which means the myocardium does not die. However, unstable angina can rightfully be called a “pre-infarction state”, and therefore, the treatment of such patients includes almost the entire complex that we discussed for patients with a heart attack, including mandatory coronary angiography and often the installation of a stent.
Author 
Anton Rodionov, cardiologist, candidate of medical sciences, associate professor of the department of faculty therapy No. 1 of the Sechenov First Moscow State Medical University
When a person develops a myocardial infarction, blood flow in one or more coronary vessels is disrupted. This leads to an imbalance between the need of myocardiocytes for oxygen and its supply. Changes in metabolism due to lack of nutrients aggravate the condition of the affected tissue. As a result, cardiac muscle cells begin to necrotize and die. In place of the dead tissue, a scar forms. In this article I want to talk about the mechanism and possible consequences of such a “replacement”.
Development mechanism
At the time of development of an acute infarction, a sharp disruption of the blood supply to the myocardium occurs for the following reasons:
- Rupture of an atherosclerotic plaque under the influence of a sharp jump in pressure, increased heart rate and acceleration, and accelerated blood flow through the coronary vessels.
- Blockage of blood vessels due to blood thickening (acceleration of platelet aggregation, activation of the coagulation system, decreased rate of blood clot lysis).
- Spasm of the coronary artery (vasoconstriction).
I often observed patients in whom several factors were identified as the cause of the disease with myocardial damage. In young patients, vasospasm is often the basis of pathological disorders, which is not possible to determine after the start of treatment.
Expert advice
I strongly recommend starting treatment in a hospital immediately after an acute attack, since only in this case is it possible to limit the further spread of necrosis and minimize irreversible changes in the myocardium.
The study of histological samples confirms the destruction of the cardiac myocyte 20 minutes after the development of ischemia. After 2-3 hours of lack of oxygen, their glycogen reserves are depleted, which marks their irreversible death. Replacement of myocarditis with granulation tissue occurs within 1-2 months.
As my practice and the observations of colleagues show, the scar on the heart is finally consolidated after six months from the moment the first symptoms of acute infarction appear and is a section of coarse collagen fibers.
Classification
Heart scars can be classified according to their location and extent of distribution.
They can be located along the coronary vessels:
- Impairment of blood flow in the anterior interventricular artery leads to ischemia with the subsequent appearance of a scar in the area of the septum between the ventricles, involving the papillae and lateral wall, as well as on the anterior surface and apex of the left ventricle.
- The infero-posterior and lateral part is affected when the left circumflex coronary artery is blocked.
- Problems with the blood supply to the myocardium in the right artery results in irreversible changes in the right ventricle and can affect the posterior inferior part of the left ventricle and the septum. But such a violation is extremely rare.
According to the type of distribution, scars can be local (focal), which can be compared to a scar on the body, or diffuse (multiple). Experts call the second option dystrophic changes in the myocardium.
How does a scar manifest itself?
The acute period of a heart attack is characterized by a variety of clinical manifestations. The main symptom is pain, which can be relieved exclusively with narcotic analgesics and can last from an hour to 2-3 days. Then the pain syndrome disappears and the formation of an area of necrosis begins, which takes another 2-3 days. Then comes a period of replacing the affected area with loose connective tissue fibers.
If the correct treatment tactics are used, the following symptoms are noted:
- development of compensatory hypertrophy;
- rhythm disturbance (which often accompanies the acute period) is eliminated;
- tolerance to stress gradually increases.
If a scar that appears on the heart crosses the conduction paths along which the impulse travels, a conduction disorder is recorded, such as a complete or partial blockade.
In the case of successful recovery after a primary small-focal infarction, I did not notice any significant disturbances associated with the functioning of the heart in my patients.
If patients have formed a large scar or many small ones, the following deviations are observed:
- dyspnea;
- increased heart rate;
- the appearance of edema;
- enlargement of the left chambers of the heart;
- pressure fluctuations.
How dangerous is this?
The most dangerous is the development of a scar as a result of large-focal or transmural infarctions, as well as several repeated violations in different basins of the coronary vessels with diffuse multiple lesions.
In the case of a large area of damage or widespread cardiosclerosis, the remaining healthy cells cannot fully compensate for the work of damaged cardiomyocytes. The frequency and strength of contractions increases in order to provide organs and tissues with oxygen and necessary substances.
As a result, tachycardia develops; with its appearance, the load on the heart becomes even greater, which leads to dilatation of the left ventricle and atrium. As it progresses, blood stagnation appears in the right side with the development of heart failure.
I also observed another type of complication: a scar on the heart after a heart attack with extensive and deep damage to all layers of the organ caused the formation of an aneurysm due to the thinning of its wall.
The reasons for the appearance of such a defect are:
- transmural lesion;
- increased blood pressure;
- increased blood pressure inside the ventricle;
- excessive physical activity of the patient, refusal to comply with the regimen.
An aneurysm leads to the rapid development of heart failure, the formation of a parietal thrombus, and pronounced stagnation in the systemic circulation. Often complicated by severe rhythm disturbances leading to death (paroxysmal tachycardia and ventricular fibrillation).
Diagnostics
In order to establish a diagnosis, I conduct a survey and study the medical history (mainly, it includes ischemic heart disease with a history of heart attack). External examination usually reveals increased respiratory rate, weakening of heart sounds during auscultation, the presence of edema, and various rhythm disturbances. I will definitely take a blood pressure measurement.
Then I send you to the following research:
- general and biochemical blood test, coagulogram (will help establish concomitant diseases, cholesterol levels and clotting time);
- EchoCG or ultrasound of the heart helps to establish the presence of localized or diffuse areas of connective tissue, allows you to clarify the location and extent of distribution;
- MRI helps to visualize and reliably assess the affected area;
- scintigraphy is required to determine dysfunctional areas of the myocardium.
With the help of an ECG after a transmural and large-focal infarction, it is possible to clarify where the scar is located on the diseased heart.
It is determined by the presence of a Q wave in different leads, as can be seen in the table.
Localization of post-infarction scar in the left ventricle
Content
The mechanism of scar formation on the heart after myocardial infarction
Causes of scars
Treatment of cardiosclerosis. Stem cells in scar treatment
Danger of scars. Life after myocardial infarction
Coronary heart disease is a pathology of the cardiovascular system, the essence of which is an insufficient supply of oxygen to the heart muscle. This occurs due to circulatory problems. The most dangerous consequence of IHD is myocardial infarction. This is a serious pathological condition in which muscle cells die and are subsequently replaced by connective tissue. The connective tissue area is called a scar.
The mechanism of scar formation on the heart after myocardial infarction
What triggers myocardial infarction? There are several reasons for the development of complications of coronary heart disease:
- Atherosclerosis of the coronary arteries. Mechanical narrowing of the lumen of blood vessels occurs due to the presence of atherosclerotic plaques in them. There is no opportunity to speed up blood flow due to physical or emotional stress. This leads to the development of myocardial infarction precisely during psychoemotional or physical overstrain.
- Spasm of the coronary arteries. Taking medication, hypothermia, the first hours after waking up, emotional stress are factors that provoke vasospasm.
- Blockage of the coronary arteries by a blood clot. The formation of a blood clot in any part of the cardiovascular system is dangerous due to the detachment of such a clot with subsequent blockage of the vascular lumen.
A sudden and complete cessation of blood supply to an area of the heart muscle provokes the death of muscle tissue. Over time, the site of necrosis is replaced by connective tissue. A scar on the heart is called cardiosclerosis.
Causes of scars
The main cause of cardiosclerosis is myocardial infarction. The death of a section of the heart muscle is essentially a wound; after some time, it scars, being replaced by connective tissue. In addition to myocardial infarction, as the main cause of scar formation on the heart, the following conditions can lead to cardiosclerosis:
- Rheumatism. A disease that is mistakenly considered to be a post-articular pathology. But musculoskeletal disease is only one form of rheumatism. The source of rheumatism is the membranes of the heart. The most serious form is cardiac. This is a pathology characterized by the spread of the inflammatory process to all the membranes of the heart.
- Myocarditis. A condition resulting from infectious diseases. Bacteria, fungi, viruses, helminths are the causative agents of myocarditis. General intoxication of the body during this disease provokes the occurrence of an inflammatory process in the muscle layer. The presence of unpleasant sensations in the sternum after suffering from measles, chickenpox, mumps, may indicate the presence of a scar on the heart.
- Cardiac ischemia. Deterioration of blood supply together with metabolic disorders are provoking factors for many diseases.
In addition to the main causes of scars on the heart, cardiosclerosis can also be provoked by:
- diabetes;
- anemia;
- obesity;
- excessive physical stress;
- violation of metabolic processes.
Treatment of cardiosclerosis. Stem cells in scar treatment
A scar on the heart is a condition that is the result of cardiovascular pathology, so treatment of cardiosclerosis also involves treatment of the underlying disease.
In addition to electrocardiogram data, the presence of a scar may be indicated by the following symptoms:
- dyspnea;
- swelling;
- increased fatigue;
- chest pain;
- bluish tint to fingertips.
Therapy for fibrosis (overgrowth of connective tissue) after a heart attack should include the following medications:
- acetylsalicylic acid;
- nitrates;
- diuretics;
- beta blockers;
- metabolites.
The selection of medications should be carried out exclusively by the attending physician. Self-medication is strictly prohibited. Scar growth continues for a month after a heart attack. Therefore, dynamic monitoring of the patient is very important. Surgical treatment is prescribed for rapid deterioration of the condition. Surgical treatment means transplantation of a living heart, bypass surgery, removal of the protruding part of the scar, and installation of a pacemaker.
Modern medicine also offers a treatment method such as the introduction of stem cells. The introduced cells accumulate in the damaged area of the organ, replacing connective tissue cells with primary cardiomyoblasts. This allows you to fully or partially (depending on the severity of the process) restore the contractile function of the heart muscle.
General recommendations for scarring include following a special heart diet and avoiding stress and physical activity.
Danger of scars. Life after myocardial infarction
What types of scars are there, and why are they dangerous? The danger of scarring lies in the disruption of the contractility of the heart muscle, which provokes the development of heart failure. Turning off a section of the heart from working forces the rest of the myocardium to contract in an enhanced mode. Lack of assistance to the organ can lead to disability and repeated heart attacks.
The following types of fibrosis are distinguished:
- Diffuse. The prevalence of lesions affects all muscle tissue.
- Focal. It is distinguished by a clear location in a specific area of the organ. The size is no more than two to three cubic millimeters.
- Diffuse-focal. Uniform distribution of fibrosis foci throughout the organ. The initial size of the lesions is no more than a few cubic millimeters. However, there is a possibility of increase due to fusion of lesions.
All patients who have suffered a myocardial infarction are interested in whether a full life is possible after such a serious illness, and what can be done to improve the quality of life. The course of life after myocardial infarction depends on the speed of medical care, the size of the scar, and lifestyle before the disease. Regardless of these factors, there are five components of a healthy heart that are important to adhere to:
- lack of stress;
- weight control;
- proper nutrition;
- adequate physical activity;
- eliminating bad habits.
It is much easier to prevent the occurrence of connective tissue areas than to get rid of them. Maintaining a healthy lifestyle, paying close attention to your well-being, health and timely seeking medical help guarantees the prevention of scarring on the heart.



