Growth and development of nevi
Nevi are cells of our skin in which pigment is accumulated in large quantities. Considering that the pigment can accumulate anywhere, it is not surprising that there are no exceptions for nevus where it appears, even on the mucous membrane. So a mole in the mouth is not something strange or dangerous, although it is quite rare, just like on the eyes. Some nevi appear immediately after birth - these are skin developmental defects, others - in the first years of life. Most often, pigment spots appear during adolescence, when hormones in people's bodies are raging.
In some places there are a lot of nevi, in others there are very few of them. This is due to a number of factors. Many people notice small moles on the neck, the reasons for which are:
- genetic predisposition,
- hormonal imbalances in the body,
- ultraviolet irradiation.
The biggest problem for every person is excessive sun exposure. This causes new pigment spots to appear on the neck, shoulders and face, which can cause them to disappear or degenerate. Sun exposure can also cause the disease vitiligo (white spots on the skin that cannot be treated). Therefore, it is worth protecting your body from the sun and solarium.
If you have a mole on your pupil, it means that you have again neglected sun protection. Dark glasses help those with increased accumulation of pigment in the pupils to get rid of the appearance of nevi in such unusual places. In addition to glasses, a hat that covers your eyes from ultraviolet radiation will also help.
It is also important to know that changes in nevi do not bode well, so you should monitor this especially carefully. Only a congenital birthmark can grow along with how you grow. Acquired nevi should not change, and in cases of changes, you should immediately seek help from a doctor.
Removing pigment spots
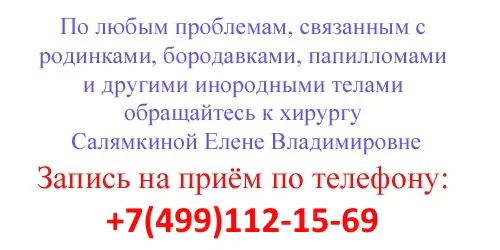
It is not surprising that you are concerned about whether to remove moles. Many doubts may lie in wait for you along this path, but remember, if you entrust this operation to Elena Vladimirovna Salyamkina, there will be no complications. On online forums, many share their experiences of removing nevi, after which they have:
- a new mole grows,
- inflammation appears
- there is melanoma.
But you should understand that a nevus can only be removed in a medical facility by a qualified surgeon! Only this can guarantee your safety and health. It is also important to monitor the wound after removal surgery. For example, if a mole gets wet, the wound may become inflamed. After excision of a nevus by any method, it is necessary to avoid getting the pigment spot, or more precisely the place where it was, wet for about a week. Here are the treatment options for nevi:
- Laser surgery. This is the process of excision of a pigment spot with a laser beam. The procedure is painless, bloodless and very fast. There are no traces left after the operation;
- Surgery. This is the removal of a nevus with a scalpel under local anesthesia; stitches are placed on the wound, so a scar may remain;
- Surgitron. This is a device that removes nevus using high frequency radio waves. The operation itself is called radiosurgery, it is quite well known, used and bloodless;
- Cryodestruction. This is practically burning out moles with liquid nitrogen at a very low temperature. However, because of this, skin cells are destroyed, therefore, wound healing will take many times longer;
- Electrocoagulation. This is the effect of high-frequency electric current on the pigment spot. The operation may leave a thermal burn, which will damage healthy skin and delay the recovery process.
Checking nevi for degeneration
What options for examining and checking pigmented spots are acceptable today:
- self-examination (examination of the body at home),
- dermatoscopy (study of changes using a dermatoscope, which increases the examined area by 10 times),
- histology (examination of removed nevus in the laboratory).
Not all neoplasms are worth studying so carefully, but if some changes appear that are difficult to notice, then you should consult a doctor. At home, you can pay attention to the following symptoms of a dangerous change in the nevus:
- itching of the mole, peeling and dryness,
- the appearance of deformation on the surface of the formation (cracks, nodules, bumps, compactions),
- change in the boundaries of the formation (torn boundaries, blurring, asymmetry),
- bleeding, suppuration,
- The color of the nevus began to change in any way,
- swelling, bloating and redness,
- growth (sharp increase in nevus or its disappearance).
As for other examinations, they will not bring results; no fortune telling or correspondence consultations can give you a real answer to your questions. A biopsy of a mole will also not help; on the contrary, it will complicate your situation. A skin biopsy is acceptable, but in a place where there is no birthmark. Many people believe that a nevus biopsy cannot be dangerous, because a nevus is skin cells. But do not forget that a lot of pigment has accumulated under the epidermis, which can begin to behave aggressively due to the biopsy.
It is important to be especially careful about nevi in potentially dangerous places on the body. This includes a mole on the back of the hand, on the sole of the feet, on the scalp, etc. These places are extremely easy to damage and injure, so doctors advise removing such growths as soon as possible. If you do not want to get rid of traumatic spots on your body, then you need to at least monitor whether they are changing. Any changes in nevi may indicate the beginning of a complex process of degeneration of a benign tumor into melanoma.
Is it possible to do a nevus biopsy and why?
Every good doctor will tell you that biopsy of a mole is unacceptable if you want to save your health and life! During a biopsy, it is necessary to excise the cells of the tumor without removing it. In essence, the biopsy simulates a serious injury to the nevus, which can easily cause degeneration of the injured pigmented formation. After this, the biopsy will not show any negative results, but you will notice that the nevus has begun to change and will receive a diagnosis of melanoma as a “gift”. Therefore, under no circumstances agree to a biopsy of a birthmark and refuse the doctor who offers such a study!
There are no home treatment options for nevi; you won’t be able to check them at home. Any medicine for moles that your friends offer you can only do harm. The only option that will help is to remove the nevus completely. If you want to find out whether there was a danger from a remote formation, order histology of the mole. This is a paid operation and is not included in the cost of nevus removal, but if the doctor advises you to do this or you are worried yourself, do not refuse the study.
Remember that a biopsy is not a cure for moles; it cannot remove tumors. A biopsy involves taking skin cells for research, but taking cells with pigment, i.e. nevi are not allowed! About 5 years ago, many patients believed that nevus biopsy was acceptable, but now everyone understands how dangerous it is, because not a single sane person will say that this is normal, safe and possible.
IMPORTANT! A biopsy can only be performed on an area of skin free from moles, and biopsy of a mole is prohibited and unacceptable. This can affect the degeneration of the area under study, cause melanoma and a protracted course of treatment and rehabilitation.
Surgeon, Candidate of Medical Sciences, Associate Professor of the Department of Surgical Diseases and Clinical Angiology, Moscow State Medical University named after. A.I. Evdokimov.
Has thematic improvements in oncology, thoracic surgery, vascular surgery, laparoscopic and robotic surgery
Area of professional interests: general surgery, laparoscopic and open interventions on the abdominal organs, for tumors of the gastrointestinal tract.
Surgical treatment for acute and chronic diseases of the gastrointestinal tract (cholecystitis, hiatal hernia, complications of peptic ulcer of the stomach and duodenum, tumors of the stomach, small and large intestine, reconstructive surgery on the colon) hernia of the anterior abdominal wall (umbilical, inguinal, postoperative), removal of skin and subcutaneous tissue tumors.
Telephone for consultation: 8 (903) 969-18-59.
With constant trauma to a large nevus, inflammation and bleeding often occur. In this case, the doctor will suggest testing a sample of skin tissue. In what cases and how is a mole biopsy performed? What should you pay attention to, should you agree to an invasive procedure?
What is and indications for biopsy
Nevus biopsy is a misconception. It is more correct to talk about examining the skin in order to identify pathologies of the dermis of various etiologies. The analysis is carried out for bacterial infections, if a fungus or a malignant nature of the disease is suspected.
During surgery, a small piece of skin is excised and sent for cytology. If a malignant nature is suspected, the mole should be completely removed with a supply of healthy tissue. The resulting biopsy specimen is necessarily sent for histological examination.
Indications for collecting biological material:
- suspicion of the malignant nature of the neoplasm;
- detection of benign nevus;
- diagnosis of bacterial infections, including skin tuberculosis;
- examination of tissues in diseases accompanied by an inflammatory process;
- screening, dynamic observation during treatment of oncological pathologies;
- autoimmune processes (lupus, psoriasis);
- scleroderma of various etiologies;
- fungal invasion;
- periarteritis nodosa;
- Darier's dyskeratosis;
- treatment control.
Methods for examining a mole before removal
The patient can independently assume the malignant nature of the nevus. For self-diagnosis, the ACCORD or ABCDE methods are used. The size of the birthmark, its symmetry and shape, the color of the formation, and the presence of uneven edges are taken into account.
If you detect at least one sign, you should contact a dermatologist.
Additional necessary examinations:
- examination of the skin - search for deformations indicating the development of melanoma;
- histological and cytological examination of tissues taken after removal of the nevus - carried out by an oncologist in the direction of a dermatologist;
- CT, MRI of various organs and systems if active metastasis is suspected - this will allow you to develop patient management tactics and make prognoses.
Additionally, urine and blood tests are indicated. This is required to assess the functioning of the urinary system and liver. Based on this information, the doctor will decide on treatment tactics.
Difference between puncture, biopsy and mole scraping
To diagnose oncology, various methods of collecting biological material are used. How to understand diversity?
- Puncture (fine-needle biopsy) - when tissue is collected, it is not the tumor site that is obtained, but its cells. The tumor membrane is punctured and biological material is collected. The study is carried out using cytological methods. Indicated for collecting samples from lymphatic collectors when diagnosing thyroid cancer. It is not used to study nevus tissue.
- Biopsy – removal of tumor tissue. This is a diagnostic and therapeutic procedure. If a nevus is suspected of being malignant, an excisional biopsy is performed to remove the suspicious formation and capture areas of healthy tissue. The amount of indentation from the edge during the initial biopsy is no more than 1 mm. After histological examination of the tissue, according to indications, more extensive excision of the skin is performed. This helps prevent relapses of the disease.
- A mole scraping or shaving biopsy is the removal of the top layer of the tumor using a specialized blade-like instrument. This method is used when excisional biopsy is not possible when melanoma is localized on the fingertips, face, or genitals.
The standard method for examining suspicious nevi is an excisional biopsy. Scraping and other methods are either not used, or may contribute to tumor growth and the appearance of secondary tumors.
Why and how it is carried out
Biopsy is a minimally invasive technique for research and treatment of various diseases. Allows you to establish the correct diagnosis. The concept of “biopsy” is not identical to the diagnosis of “cancer”. The invention of this method has made it possible to reduce the frequency of extensive surgical interventions and the use of aggressive medications.
No specialized preparation is required for skin examination. It is advisable to stop taking any medications, especially blood thinners, 1 week before the procedure. On the day of sample collection, stop smoking and drinking alcohol. If you have a history of a chronic disease, you should inform your doctor.
The tissue is excised, the bleeding is stopped with the help of hemostatic drugs. If the size of the wound surface is significant, then suturing the edges of the wound or applying a skin implant is indicated.
Wound care after the procedure
The method of caring for a postoperative wound should be clarified with the surgeon who performed the procedure. Standard recommendations include:
- wearing a sterile bandage for several days;
- if signs of bleeding appear one day after collecting the sample, you should seek medical help;
- before treating the wound surface, you need to wash your hands with soap;
- It is not advisable to wet this area of the skin surface with water;
- the wound should be clean, without signs of bleeding or discharge of ichor;
- after water procedures, the wound surface is treated with an antiseptic as prescribed by the doctor;
- It is forbidden to deform the tissue in the wound area. This contributes to infection of the surface, reducing the rate of regeneration of the epidermis.
Complete healing takes from 7 to 14 days. To speed up tissue regeneration, the doctor will suggest antiseptic, wound-healing drugs based on panthenol. Relief of painful and unpleasant sensations only with the help of drugs. If signs of infection appear or bleeding begins, you should immediately contact a medical facility.
Decoding the results
The histological examination result form will indicate the type of cells that make up the sample and their nature. That is, either normal melanocytes or atypical cells were identified.
If the analysis has confirmed the malignant nature of the neoplasm, the doctor who conducted the study and compiled the pathomorphological report must indicate the following in it:
- The histological type of the biopsy is penetrating carcinoma or transitional state, designated as ca in-situ (stage zero cancer).
- Dimensions of melanoma, degree of germination according to Breslow in tenths of a millimeter, microlevels according to Clark.
- Indicate whether there are tissue erosions.
- The presence of infiltration of blood vessels and lymphocytes.
At the end, a conclusion is made about the stage of the pathological process and a prognosis for the patient’s survival.
The degeneration of small moles on the body cannot always be diagnosed using a dermatoscope. Erroneous diagnoses, resection of a tumor using a laser or electrical destruction pose a danger to the life and health of the patient. Histological examination of tissues is not carried out in this case.
If the nevus behaves suspiciously, you need to take a referral for a surgical biopsy of the tumor. The consequences of rash decisions will be sad. When diagnosed early, melanoma is curable in most cases.