Causes, symptoms, complaints and complications of pulmonary embolism. Diagnostic methods and methods of treating pathology.
The content of the article:- Causes of pulmonary embolism
- Main symptoms
- Diagnostic methods
- Treatment options
- Medicines
- Surgical intervention
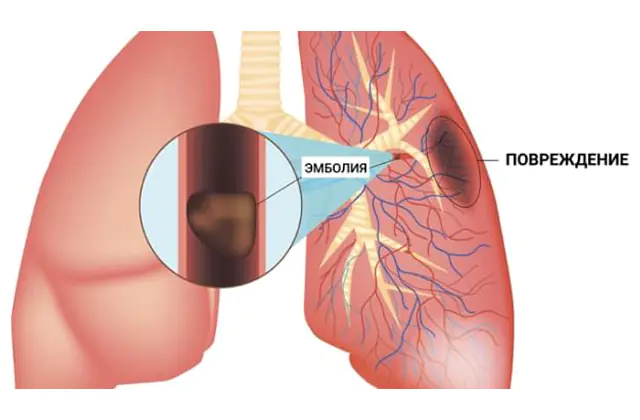
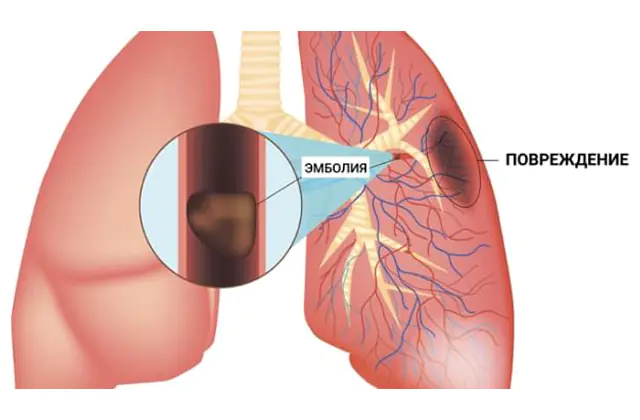
Pulmonary embolism (pulmonary embolism) is a blockage of the lumen of a branch of the pulmonary artery, or less commonly its trunk, with a piece of a foreign body (embolus) that has entered a vessel with blood flow. As a result, blood does not reach some segment of the lung through a blocked artery, and respiratory failure develops. Due to the sudden disruption of blood circulation, acute pulmonary embolism is a life-threatening condition.
Causes of pulmonary embolism
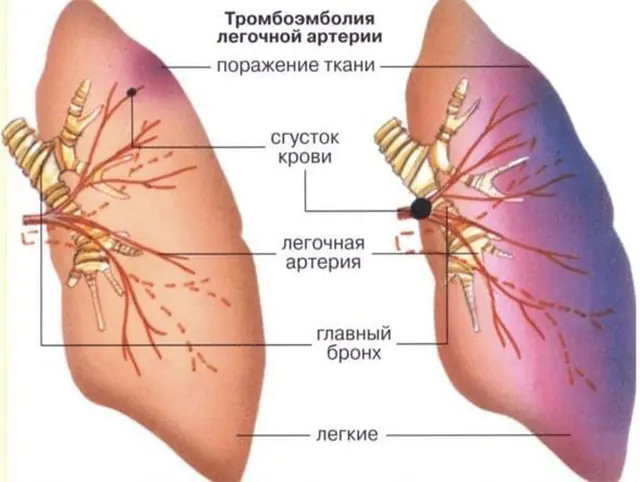
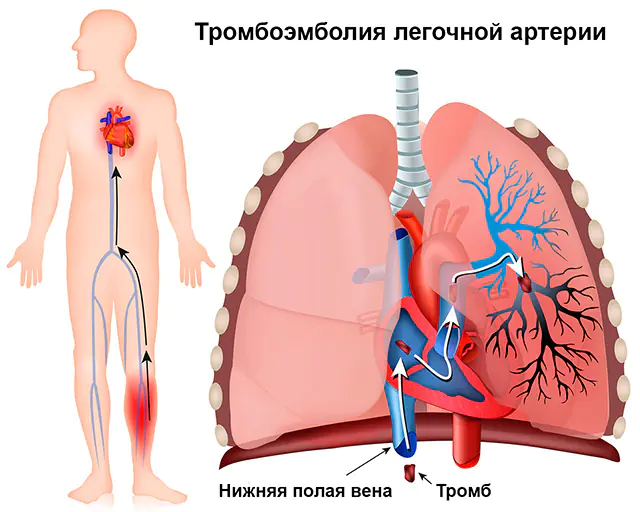
In almost 90% of cases, pulmonary embolism is caused by a thrombus, a blood clot, so the full name of the pathology is “pulmonary embolism.” The thrombus itself forms in the veins of the systemic circulation (these are the veins of the upper and lower extremities, large veins of the abdominal organs) or in the right parts of the heart (the right atrium and right ventricle). It is from these veins and cavities that the thrombus can enter the pulmonary artery, which leaves the right ventricle and sends venous blood to be enriched with oxygen to the lungs.
Pulmonary embolism can also be caused by:
- fat droplets- they enter the bloodstream when long bones are broken;
- air- if the rules for administering drugs intravenously are violated, air may remain in the syringe or dropper;
- textile— cells of a malignant tumor can enter the bloodstream when it is destroyed, a piece of collagen in diseases that destroy connective tissue (systemic lupus erythematosus).
For thromboembolism to form, conditions must be favorable. These are the factors that cause damage to the vascular wall, slow down blood flow or increase blood clotting.
Pulmonary embolism has the following causes:
- Pathological process in a vessel or cavity of the heart. Damage to the inner lining of a vessel or heart triggers the process of platelet adhesion and the formation of a blood clot. Most often, a blood clot forms during phlebitis, an inflammation of the deep veins.
- Physical inactivity. If a person is forced to remain in bed for a long time, the muscles of the lower extremities stop working, and this in turn slows down the blood flow in the veins, causes stagnation and promotes thrombosis.
- Hypercoagulation. Increased blood clotting occurs with heavy bleeding, taking birth control pills, hereditary diseases, and malignant neoplasms. Any surgical intervention or medical manipulation (venous catheterization) also increases the risk of thrombosis with subsequent embolism.
- Blood diseases. Blood tumors in which the number of red blood cells (erythremia) or white blood cells (leukemia) increases causes the blood to thicken. With the slightest damage to the vessel from the inside, more red blood cells and white blood cells accumulate on the blood clot than usual.
- Heart diseases. A blood clot forms in the right side of the heart with a sharp weakening and expansion of the muscles of the atrium and ventricle (chronic heart failure), cardiac arrhythmias (atrial fibrillation), after myocardial infarction. With rheumatism or infective endocarditis, the tricuspid valve is damaged, and an inflammatory mass forms on it - vegetations. With infectious inflammation, they tend to increase in size and easily tear off from the place of attachment.
Not every blood clot that forms in the veins can cause a pulmonary embolism. The detachment of a blood clot and its transfer by the blood flow to the pulmonary artery is possible only if it is poorly attached to the wall of the vein. Such blood clots are called floating or floating because one end is not fixed, but moves freely under the influence of the direction of blood flow. It can come off in large or small pieces, causing occlusion (closing of the lumen) of a large or small branch of the pulmonary artery.
Blockage of any branch of the pulmonary artery leads to the cessation of nutrition to an area of the lung - this is called a pulmonary infarction. The larger the size of the vessel, the larger the area that is destroyed. At the site of a pulmonary infarction, inflammation (pneumonia) develops, which often spreads to the pleura, causing pleurisy.
Main symptoms of pulmonary embolism
Symptoms of embolism depend on the number of blocked pulmonary arteries and their caliber, therefore it is customary to distinguish between massive, submassive and non-massive forms of the disease. Massive blockage causes an acute course of the disease. Acute pulmonary embolism develops at lightning speed, causing sudden respiratory failure and cardiac arrest, and has very pronounced symptoms. Submassive disease is characterized by a large volume of damage to the pulmonary arteries; the symptoms are pronounced, but do not develop as quickly as with the massive form.
Acute pulmonary embolism causes the following symptoms:
- Chest pain. It is associated with the occurrence of pneumonia and pleurisy at the site of pulmonary infarction, which leads to irritation of the pain receptors of the pleura. Discomfort is felt behind the sternum or in the right hypochondrium. Characteristically, the pain increases when the chest moves (breathing, coughing, changing body position).
- Dyspnea. Breathing disorders are caused by the appearance of so-called “dead” space in the lungs, which corresponds to the area “controlled” by the closed pulmonary artery (gas exchange does not occur in this zone). The less breathing space in the lungs, the less oxygen in the blood, and this is a signal to stimulate the respiratory center, which causes the body to breathe more often and the person to experience a lack of air.
- Cough. It occurs due to reflex irritation of the bronchi and spasm of their muscle rings. Bronchospasm develops under the influence of substances that are released from a blood clot that has entered the pulmonary artery.
- Hemoptysis. Occurs only in 1/3 of cases. When you cough, streaks of blood are released from burst vessels in the lung.
- Hiccups. It is observed when the lumen of the pulmonary artery branches located in the lower parts of the lungs closes. If the area of the lung closer to the diaphragm becomes necrotic, then irritation of the phrenic nerve occurs, and the person suffers from hiccups.
- Loss of consciousness. Caused by a sharp drop in blood pressure. In the pulmonary arteries themselves, the pressure rises sharply. Blood has difficulty entering the lungs and cannot reach the left side of the heart to spread throughout the body. As a result, the amount of blood that reaches the brain is sharply reduced. This manifests itself as dizziness or fainting. Possible mental agitation or apathy.
- Fever. In approximately half of the cases, the body temperature rises above 37°C. This symptom is caused by an inflammatory process in the “dead space” area. It is typical that antibiotics do not have a therapeutic effect for such fever.
- Blueness and pallor of the skin. A sudden drop in blood pressure reduces blood flow to the skin, causing paleness. Blueness is associated with a decrease in the respiratory surface of the lungs and the accumulation of carbon dioxide in the blood.
It is typical for pulmonary embolism that in the presence of shortness of breath and chest pain, the patient can calmly lie in a horizontal position. It is this circumstance that makes it possible to distinguish embolism from myocardial infarction.
When small particles of a blood clot enter the bloodstream from the veins, they are carried by the bloodstream into small pulmonary arteries, and a non-massive or chronic pulmonary embolism develops.
Important! All signs of non-massive pulmonary embolism are mild, so it often occurs “under the guise” of other diseases, for example, unexplained and frequent pneumonia, which quickly disappear and recur periodically.Although pulmonary embolism is considered a fatal disease, the risk of death is 30%, but if treatment is started in time, this risk is reduced to 10%.
Pulmonary embolism can have the following consequences:
- Acute cor pulmonale. This is a condition of overload of the right side of the heart that occurs over a period of hours or days. The reason for this complication is a sharp increase in pressure in the pulmonary artery. In order for blood to continue flowing from the right heart to the pulmonary artery, the right ventricle must overcome more resistance. If it fails, muscle weakness develops and blood accumulates in the veins. This is manifested by swelling of the neck veins, enlargement of the liver, and swelling of the lower extremities.
- Shock. When large branches of the pulmonary artery are blocked, a reflex drop in total blood pressure occurs. In addition, cor pulmonale causes less blood to return to the left ventricle from the lungs.
Methods for diagnosing pulmonary embolism
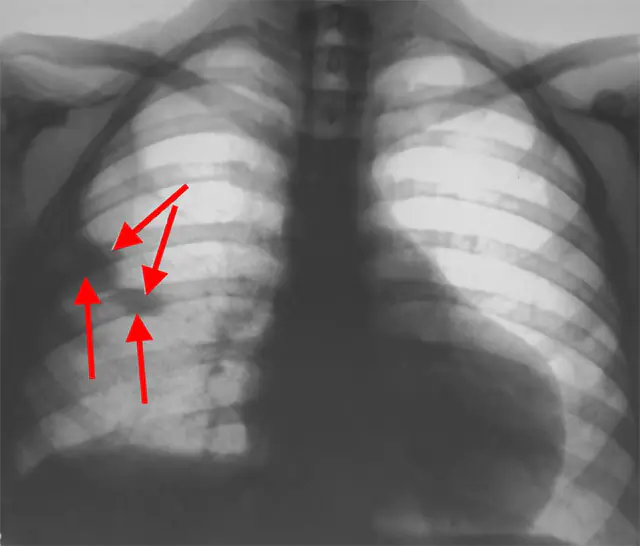
The photo shows a chest x-ray
Diagnosis of embolism includes assessing the condition of the lungs and heart, locating the location of the blockage and the source of the clot. In acute embolism, the diagnosis is made based on the symptoms, after which first aid begins. Clarifying studies and analyzes are carried out in the hospital.
Diagnosis is more difficult if pulmonary embolism has a chronic or subacute course, in which the symptoms are not expressed and do not have characteristic features. Chronic pulmonary embolism is suspected if a person has venous disease of the lower extremities and bone fractures in combination with shortness of breath and hemoptysis.
To diagnose pulmonary embolism, the following is carried out:
- Listening to the lungs. There is weak breathing and a lot of moist rales, sometimes crepitus (crackling) during inspiration. With the development of pleurisy, a pleural friction noise is heard.
- Blood pressure and pulse measurement. The pulse during embolism can be very fast - more than 100 beats per minute, and the pressure is low. Sometimes a paradoxical pulse is recorded (during inspiration, the filling of the pulse weakens), which is a sign of right ventricular heart failure.
- ECG. An electrocardiogram reveals signs of overload of the right ventricle and right atrium, sinus tachycardia (normal but fast rhythm) and arrhythmia (atrial fibrillation and flutter, extrasystoles) are recorded. In 30% of cases, the ECG may not change in any way in the presence of a blood clot in the pulmonary artery.
- Chest X-ray. The image shows a high location of the diaphragm on the side of the affected lung. Within 24 hours, signs of pulmonary infarction appear (the lesion has the shape of a triangle, corresponding to the segment of the lung). With massive and submassive embolism, the size of the heart increases and the trunk of the pulmonary artery expands.
- Ultrasound. An echo examination of the heart reveals dilatation of the right ventricle and right atrium, increased pressure in the pulmonary artery itself. Ultrasound (duplex scanning) also allows you to detect the source of a severed blood clot, see the blood clot itself in the heart or in the veins of the lower, less often the upper, extremities.
- Lung scintigraphy. With the help of radioactive technetium and xenon, it is possible to accurately diagnose pulmonary embolism. Technetium is injected intravenously to visualize the vessels in the pulmonary artery system (locating the site of blockage), and xenon is given to the patient to inhale through a mask to obtain an image of the respiratory surface of the lungs. The diagnosis of embolism is confirmed if the airiness of the lungs is preserved, but the pattern of blood vessels is sharply weakened.
- Angiopulmonography. This is an x-ray of the lungs using a contrast agent. Contrast is injected through the femoral vein using a catheter, and a series of x-rays are taken. With pulmonary embolism, a “stump” is detected - this is a defect in the filling of the artery blocked by a thrombus.
- General blood analysis. Detects an inflammatory reaction during the development of infarction pneumonia and pleurisy; with severe or prolonged hemoptysis, it will help assess the degree of anemia (low levels of hemoglobin and red blood cells).
- Blood test forD-dimer.It is mandatory to perform if a pulmonary embolism is suspected. D-dimer is a protein that is formed in large quantities when the thrombosis process starts.
Treatment options for pulmonary embolism
Treatment of the disease is always carried out in a hospital setting. In case of acute thromboembolism, therapy begins already at the stage of emergency medical care. If pulmonary embolism is diagnosed, treatment is carried out with the use of medications. In some cases, surgery is indicated.
Medicines to treat pulmonary embolism

The photo shows drugs for the treatment of pulmonary embolism
The drugs that are prescribed for pulmonary embolism are designed to stop the process of increasing the size of the blood clot and destroy the blood clot itself, which is stuck in the pulmonary artery.
For pulmonary embolism, the following medications are prescribed:
- Thrombolytics. They consist of substances that can destroy a blood clot. The main drug is Streptokinase. Analogues are Urokinase and Alteplase. The price for 1 bottle of Streptokinase is about 7 thousand rubles (3 thousand hryvnia), for Alteplase you need to pay 22-28 thousand rubles (9-12 thousand hryvnia). Urokinase costs 15-19 thousand rubles (6-8 thousand hryvnia).
- Anticoagulants. Suppress the action of blood clotting factors, thereby stopping the process of thrombus enlargement. The main drug is Heparin. The price for 5 ampoules ranges from 360 to 560 rubles (180-230 hryvnia). Analogs are Enoxaparin, Fondaparinux. The cost of analogues is much higher - 1700-5000 rubles (690-2100 hryvnia) for 10 syringes with solution. Dabigatran, Rivaroxaban, and Warfarin also have a similar effect. All three drugs are in different price categories. Warfarin in the amount of 100 tablets can be purchased for 180 rubles (73 hryvnia), and newer drugs Dabigatran and Rivaroxaban - from 1000 rubles (400 hryvnia) for 10 capsules.
- Antiplatelet agents. They act on platelets, blood cells that stick together, creating a framework for a future blood clot. For pulmonary embolism, Ticlopidine is indicated. Analogues are Clopidogrel, Plavix. The price is about 2,700 rubles (730 hryvnia) for a package of 28 tablets.
Additionally, oxygen, cardiotonics (stimulating heart contraction and increasing blood pressure) and intravenous solutions to maintain blood pressure are indicated to maintain cardiac activity.
Surgery for pulmonary embolism
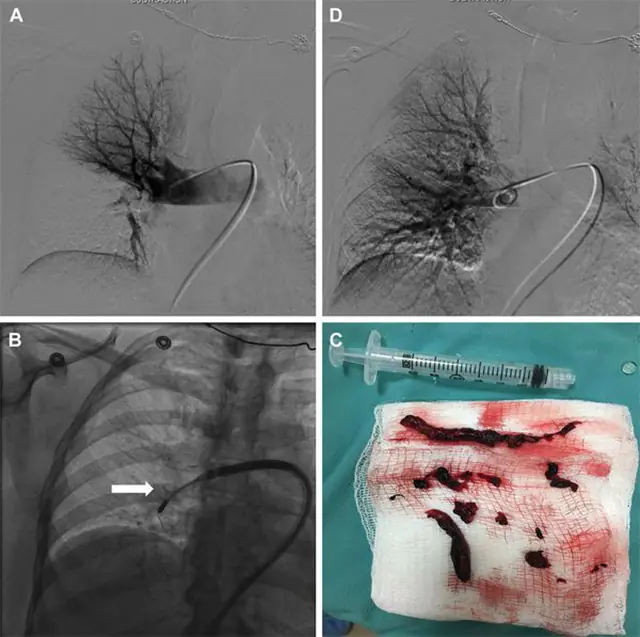
Pulmonary embolism, according to the doctor's recommendations, is eliminated through surgery if there is a massive blockage of the pulmonary arteries. For thromboembolism, two types of operations can be performed: embolectomy and installation of a vena cava filter.
Embolectomy is the removal of blood clots from blood vessels. It is performed if complications develop, such as shock and acute cor pulmonale. Indicated in the absence of effect from the use of thrombolytics or in the presence of contraindications to their administration.
Surgical intervention is carried out directly and indirectly. Direct removal is an open operation performed under artificial circulation.
Currently, the indirect method of removing a blood clot through a catheter is more often used. A catheter inserted into a closed artery destroys the blood clot inside the vessel. Fragments of a destroyed blood clot can be removed through a special syringe. In some cases, these fragments are also carried away by the bloodstream, becoming stuck in smaller branches of the pulmonary artery (small blood clots are easier to treat with medication).
In patients with a blood clot in deep vessels or with a high risk of recurrent embolism, a special mesh called a vena cava filter is installed in the inferior vena cava. This “trap” catches all the blood clots that decide to break off and float towards the pulmonary artery. Installation of a vena cava filter is performed using a closed operation through a probe.
What is pulmonary embolism - watch the video: