
Types, routes of infection and symptoms of visceral and cutaneous leishmaniasis. How is the disease diagnosed? Treatment of various types of leishmaniasis and prevention.
The content of the article:- Description and types
- Reasons for development
- Main symptoms
- How to treat leishmaniasis
- Visceral
- Cutaneous and mucocutaneous
- Prevention
Leishmaniasis is a parasitic disease, the causative agent of which is transmitted by certain types of insects (mosquitoes, sand flies and others), and therefore is more common in tropical and subtropical regions. The World Health Organization (WHO) classifies the disease as a neglected disease. This means the disease is one of 17 most commonly found in poor and developing countries. Despite modern developments, treatments for leishmaniasis are not available in such regions.
Every year, more than 1 billion people suffer from neglected diseases, and more than 500 thousand die. Based on the number of victims, WHO compares “forgotten” pathologies with AIDS, malaria and others. If in the first case it is mainly residents of poor countries who suffer, then in the second the public is more aware of the problems. Meanwhile, the problem of parasitic disease can be solved with accessible treatment and sufficient prevention.
Description and types of leishmaniasis

The photo shows leishmaniasis on the human body
The parasitic disease leishmaniasis, the causative agent of which belongs to the genus of protists (eukaryotic organisms), is found in 88 countries. The disease is also called black disease, dum-dum fever, kala-azar. Of the entire list of countries where pathology is common, 13 are among the poorest countries in the world.
The first attempts to study the causative agents of the disease were carried out by British Army officer W.B. Leishman, who discovered oval bodies in samples of the spleen of a person who died from infection. Inspired by Leishman's work, Nobel laureate Ronald Ross named the eukaryotic organisms he discovered that cause leishmaniasis in humans, Leishmania.
It should be noted that the disease is caused by more than 20 types of zoonotic infections. For the causative agents of this group of diseases, animals and humans are the natural environment.
There are two morphological forms of Leishmania:
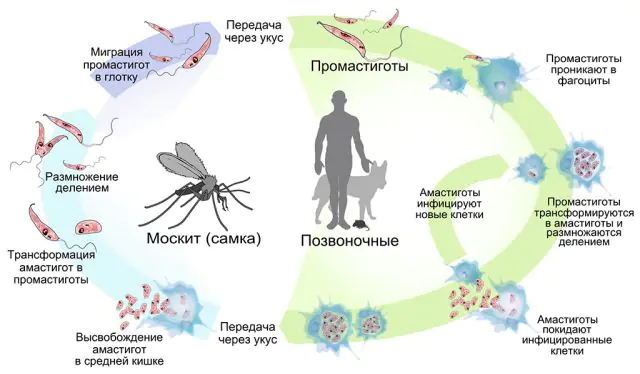
- Promastigotes. They are located in insects that carry leishmaniasis, have a fusiform oblong shape, and are mobile due to the long anterior flagellum. In the form of promastigotes, they can also remain viable for some time on an artificial nutrient medium. The disease is transmitted by Phlebotomus and Lutzomyia mosquitoes. For the former, their habitat is North and South America, and for the latter, Africa.
- Amastigotes. A form characteristic of an infected vertebrate animal (including humans). This pathology occurs in dogs, rodents, and less commonly in cats and horses. Several cases of kangaroo infection have been reported in Australia. The infection is located inside the cell, forming specific “garlands” of oval or round microorganisms with a short flagellum. Such bodies are practically motionless.
Accordingly, the life cycle of the parasite includes residence in two hosts sequentially: an insect and a vertebrate. Mosquitoes acquire the infection from the blood of an infected mammal when they bite. Once in the body of a female mosquito (and only female insects consume blood), the parasite is based in the back of the food canal, where it begins active reproduction. Within 7-10 days, the number of parasitic microorganisms inside the leishmaniasis vector becomes so large that it reaches the upper digestive tract. Subsequently, the infected insect, biting the victim, cannot swallow the blood after the bite due to blockage of the tract. By regurgitating “saliva” back into the wound of the vertebrate, the mosquito transfers the promastigotes to a new host. In one bite, 100-1000 parasites can enter the wound of a person or animal.
In the vertebrate body, neutrophils (a subtype of leukocytes) move to the site of an insect bite, whose task is to block and digest solid foreign particles. Cutaneous leishmaniasis and other forms of the disease do not develop inside neutrophils, since the pathogen does not have the opportunity to multiply. However, under the influence of natural processes in the body, neutrophils disintegrate into individual bodies, which are captured for further processing by macrophages. Thus, the parasite enters macrophages, bypassing active attacks by the immune system. Already inside macrophages, promastigotes transform into amastigotes. This process takes on average 4 days. In the form of an amastigote, the parasites multiply every 24 hours in the body of a new host.
There are more than 20 species of parasites from the genus Leishmania, but only a few forms of leishmaniasis are recognized. Today, the clinical and epidemiological classification of pathology predominates, dividing the disease into the following types:
- Cutaneous leishmaniasis. Includes one form of the disease - mucosal, also called mucocutaneous. Up to 1 million cases of this type of pathology are recorded annually. The main number of infected people falls on 7 countries, mainly in the Middle East and South America. The pathology is characterized by pronounced skin lesions, stigmas, and skin ulcers. The mucous form is found only in the New World and is manifested, in addition to the skin, by damage to the mucous membrane.
- Visceral leishmaniasis. It is characterized by attacks of fever, enlargement of internal organs, and a sharp loss of body weight. This type of disease is recorded mainly in equatorial regions. Every year, 90 thousand people are infected with parasites of this species, but WHO claims that the statistics are incomplete, only 25-45% of patients seek help, and in other cases the pathology is not diagnosed due to refusal or inability to see a doctor.
Causes of development of leishmaniasis
As already noted, the route of infection with leishmaniasis is from an infected insect to a person. In this case, up to 90 species of insects can serve as carriers.
Depending on the source of infection, the following types of leishmaniasis are distinguished:
- Anthropotic- insects become infected from a sick person, this type of pathology can be passed on to an animal, but when an infected animal is bitten by the next mosquito, the insect is not infected;
- Zoonotic- an insect becomes infected from other animals, and then transfers the parasite to humans.
Cases of parasite infection have become more frequent due to environmental changes: the construction of irrigation canals and dams leads to changes in the natural habitat of insects.
It is noted that cases of infection with parasitic pathology have increased significantly due to climate change. Thus, an increase in humidity with a simultaneous increase in average daily temperature contributes to the expansion of the habitat of parasite carriers, and drought and crop failures lead to the migration of various population groups to areas endemic for parasites.
Indirect causes of the spread of the disease also include urbanization. Leishmaniasis in humans can occur as a result of invasion of new forested, previously uninhabited areas. But, despite the various ways of infection with leishmaniasis, the pathology does not actively manifest itself in everyone.
Associated risk factors for the development of leishmaniasis are:
- Low level of socio-economic conditions— open sewers and landfills near densely populated areas create an excellent breeding ground for insects, also providing them with “human” food;
- Cultural characteristics in some underdeveloped countries— sleeping in the open air makes it easier for insects to gain access to the human body, and as a result, for infection by the parasite;
- Unbalanced nutrition of low-income groups of the population(the main risk group susceptible to diseases) - the likelihood of infection is significantly higher in people suffering from a lack of protein, iron, and zinc in the diet.
Main symptoms of leishmaniasis

Signs of leishmaniasis depend on the type of disease, the general health of the patient, and the timeliness of assistance. Thus, the visceral type of leishmaniasis may not show external signs for a long time. However, with a weakened immune system, symptoms develop over several weeks. During this period, the patient may have a fever several times, an upset stomach and a sharp decrease in body weight, and as a result, general weakness. A detailed examination of such patients will show an enlarged spleen and liver, and in some cases enlarged lymph nodes become noticeable. Without proper treatment, complications develop in the visceral form of pathology - a decrease in blood cells, susceptibility to other infections, and in an advanced state - death.
Depending on the location of the pathology, visceral infection can also manifest itself as ulcers in open areas or throughout the body. When treated, such ulcers remain for up to several months (for those infected with parasite strains from East Africa) or even several years (if the infection occurred with strains from India).
At the time of infection with cutaneous leishmaniasis, a small bump appears at the site of the insect bite. As the parasites multiply in the body (the process takes from several weeks to several months), the number of bumps on the skin increases. The seals themselves eventually open as weeping ulcers. If the wound does not become infected, which, given the unhygienic conditions for the spread of the disease, is unlikely, it will be covered with a scab. Such wounds take several months to several years to heal, leaving behind scars.
The signs of mucosal leishmaniasis are the same as those of the cutaneous type, only the ulcers cover, in addition to the skin, also the mucous membranes. The first wounds appear in the nose or throat, as evidenced by nasal congestion, bleeding, and, over time, facial deformation.
Important! In patients with AIDS, the symptoms of parasite infection are more active and vivid, and complications develop much faster. Early diagnosis and treatment of pathology can save the patient's life.Diagnosis of leishmaniasis is carried out on the basis of a general blood test, analysis of biomaterials from the ulcer, as well as analysis of tissue from the lymph nodes. Without fail, the doctor collects an anamnesis, taking into account the patient’s travels over the previous 2 years. It is important to understand that the diagnostic methodology depends on the region of infection.
Thus, an indication of visceral pathology will be an increased ESR in the blood, an increased content of globulins, and anemia. Antibodies to parasites may also be detected in the blood. At the same time, antibodies will not be detected in patients with immune dysfunction, as well as in skin lesions. In this case, the patient will be recommended to conduct a microscopic examination of a smear of ulcers, molecular tests to search for DNA of the pathogen, and collection and analysis of cerebrospinal fluid.
Important! To establish the exact cause of the disorders, the patient undergoes differential diagnosis; with the help of a comprehensive examination, the presence of syphilis, lupus and other pathologies is excluded.How to treat leishmaniasis?
When the first symptoms of leishmaniasis are detected, if the patient has reasons to suspect infection with such a parasite, it is necessary to urgently consult an infectious disease doctor. Treatment of the disease depends on the form of the pathology, the geographic location of infection, and the type of parasite. If facial deformity has already begun, reconstructive surgery will be recommended after eliminating the parasite. During rehabilitation, it is important for the patient to monitor nutrition and personal hygiene rules, and maintain immunity at the proper level.
Treatment of visceral leishmaniasis

In the visceral form of the disease, treatment should be immediate. Drugs for leishmaniasis are recommended exclusively by a doctor, taking into account the location of infection, as well as the state of the person’s immune system. Thus, in the USA, therapy consists mainly of intravenous administration of specialized antifungal drugs, which include amphotericin B. For infection in South America or Africa, injections of antimony may be recommended. But parasites from India are resistant to antimony, so they are treated with miltefosine.
This type of therapy has side effects such as nausea and vomiting. Treatment of visceral leishmaniasis is stopped if the functioning of the cardiovascular system worsens. In this case, drugs for visceral type pathology are replaced with antibiotics against concomitant infections, and the patient is recommended to receive a blood transfusion.
Note! An important component of therapy is enhanced nutrition, since patients are often depleted by parasites.Treatment of cutaneous and mucocutaneous leishmaniasis
The prescribed therapy depends on the form of cutaneous leishmaniasis, as well as the degree of damage to the patient’s body. Small skin ulcers are subjected to heat or cold treatment, treatment with Amoebicide, and injections of sodium stibogluconate directly into the wound (a similar procedure is not performed in the USA).
If large areas of the skin are affected or the mucosal form of the disease is diagnosed, if complications of leishmaniasis have developed, treatment is carried out in the form of intravenous injections of Miltefosine, Amphotericin B and other antifungal drugs. A unified methodology for treating the disease has not been developed to date due to the wide species gradation of the pathology, as well as the dependence of the manifestations of the disease on the state of the patient’s immune system.
If the mucosal form of infection has already caused a destructive complication, then reconstructive facial surgery can be performed after antiparasitic therapy. Any surgical manipulations can be performed no earlier than 1 year after the end of the main antiparasitic therapy, when the risk of disease relapse is significantly lower. A prerequisite for treatment is the patient's compliance with personal hygiene rules.
Important! In patients with AIDS, the risk of relapse of the pathology is much higher. Such patients are prescribed additional antiretroviral therapy to improve the functioning of the immune system and reduce the risk of recurrence of the disease.Prevention of leishmaniasis
Prevention of leishmaniasis requires a combined approach, since the disease itself has a complex distribution system, including a carrier, an intermediate carrier, and a patient.

The photo shows the treatment of the area against mosquitoes
The main measures to prevent the spread of leishmaniasis are:
- combating insects that carry the disease - spraying special compositions against mosquitoes, using special nets, individual human protection in places where there is a high concentration of insects;
- control of infected animals - prevention in this case depends on the geographical region and the type of animal carrier;
- socialization and cultural exchange, global partnerships that involve building affordable housing and changing the cultural habits of different nations, such as not sleeping outdoors;
- surveillance of the spread of pathology, timely diagnosis and treatment, availability of drugs for therapy.
To effectively combat leishmaniasis, WHO is carrying out a number of activities:
- provides financial subsidies to national programs to treat diseases in poor regions;
- monitors the effectiveness of implemented therapeutic programs;
- stimulates the development of affordable healthcare in remote corners of the planet;
- stimulates the search for new treatments for the disease that are available even in poor countries;
- carries out explanatory work on the importance of timely examinations and the need for treatment.
Leishmaniasis is one of the dangerous “forgotten” diseases. Despite the reassuring term “forgotten,” the pathology is detected annually in more than 1 million inhabitants of the Earth. As a rule, people from the poorest countries on the planet suffer; up to 65 thousand people die annually from this pathology. Today, effective methods for treating most forms of the disease have been developed, but therapy is not available to everyone. Inadequate nutrition, difficult living conditions, lack of normal hygiene and protection from insects provoke new epidemics. Treatment and prevention of leishmaniasis is one of the important tasks assigned to WHO and national health organizations in countries of the endemic zone. However, the prevention of pathology also implies the personal responsibility of each person: when the first signs of the disease are detected, it is imperative to consult a doctor and begin treatment in order to avoid further spread of parasites. Travelers are strongly advised to familiarize themselves with the possible risks and undergo the necessary vaccinations before traveling to dangerous regions.
What is leishmaniasis - watch the video:



