Skin cancer is a malignant tumor that develops from the epidermal cells (cover cells) of the skin.
Melanoma is an extremely malignant tumor of pigment cells in the skin.
Causes of skin cancer
The causes of skin cancer can be divided into: exogenous and endogenous.
1. Exogenous factors (external).
— One of the most important exogenous factors of skin cancer is exposure to UV radiation (in particular, the UV spectrum of solar rays). While chronic UV damage to the skin is important for the development of basal cell and squamous cell skin cancers, the risk of developing melanoma is greatest with intermittent (possibly even single) intense exposure to sunlight. This position is confirmed by the fact that skin melanoma often occurs on areas of the body protected by clothing. It has been established that skin melanoma most often affects people who spend most of their time indoors, but who are periodically exposed to intense UV exposure (recreation outdoors under the sun). While skin cancer occurs in unprotected areas. It is believed that the increase in the incidence of skin cancer to a certain extent
associated with the destruction of the ozone layer, located in the stratosphere and blocking most of the UV rays.
An important and very common etiological factor of skin melanoma is trauma to pigmented nevi (bruises, abrasions and cuts).
There are reports of the possible etiological role of rays from fluorescent lighting, chemical carcinogens, in particular hair dyes, as well as ionizing radiation and strong electromagnetic fields.
2. Endogenous factors.
— Ethnic factors influence the incidence of skin cancer. The tumor is more common among people with fair skin; it occurs less frequently among blacks.
— Skin cancer and melanoma most often occur in individuals with a small amount of pigment in their tissues (i.e., light skin, hair, eyes), which is combined with increased sensitivity to UV rays. Taking into account skin and hair color, the risk of developing cancer increases by 1.6 times in blondes, 2 times in people with fair skin and 3 times in people with red hair.
— In recent years, immune factors of the body have become increasingly important in the occurrence of skin cancer. Immunosuppression and immunodeficiency states of the body increase the risk of the disease. In addition, endocrine factors are of certain importance. In particular, it has been established that pregnancy can
have a stimulating effect on the degeneration of pigmented nevi.
— Influence on the disease by gender, age and anatomical location of the tumor. These factors are closely interrelated. Skin melanoma is 2 times more common in women, with the peak incidence occurring at the age of 41-50 years; most often affects people in the 5th decade of life; the most common locations of the tumor are the skin of the extremities and torso; In women, primary melanoma is most often localized on the face, buttocks and legs, in men - on the skin of the anterior and lateral surface of the chest wall, thighs, hands, heel area and toes.
- in addition, there are a number of hereditary skin diseases that predispose to the development of cancer (xeroderma pigmentosum, Bowen's disease, Paget's disease and others).
Types of skin cancer:
1. Basal cell carcinoma (basalioma) is a tumor from the upper layer of the epidermis, bearing the same name, it is characterized by growth into the depths of tissues with their destruction, is not capable of metastasizing, and does not relapse.
It may appear as confluent nodules measuring 2-5 mm, prone to ulceration, or as a large nodule measuring up to 2 cm or more.
It is not dangerous, except in cases where it is located on the face or ears, in which case it can reach large sizes and germinate facial organs: nose, eyeball, ear with their destruction and the development of infection, including brain damage.
More common in older people. Perhaps in combination with tumors of internal organs: intestines, stomach and others.
2. Squamous cell carcinoma - arises from cells of the deeper layers of the skin, has aggressive growth, can reach large sizes and metastasize to the lymph nodes and internal organs. The tumor has a nodule or nodule-like appearance, or a “cauliflower” appearance.
3. Skin appendage cancer is a malignant tumor of the sebaceous, sweat glands or hair follicles.
Skin appendage cancer
4. Melanoma - not a skin cancer, is an extremely aggressive malignant pigmented tumor of the skin, quickly metastasizes, practically untreatable. It has the appearance of a pigment spot (mole), bright black or pink, rapidly growing spot (non-pigmented melanoma, less common).
Often an ordinary mole degenerates into melanoma.
Skin Cancer Symptoms
There are several signs of malignant degeneration of a mole (nevus):
1) Horizontal growth;
2) Vertical growth above surrounding tissues;
3) The appearance of asymmetry or irregular outlines (scalloping) of the edges, that is, a change in its shape;
4) Complete or partial (uneven) change in color, the appearance of areas of associated depigmentation;
5) The appearance of a feeling of itching and burning;
6) Ulceration of the epidermis over the mole;
7) Wetting of the surface and bleeding from its surface;
Absence or loss of hair on the surface of the nevus;
9) Inflammation in the area of the nevus and in the tissues surrounding it;
10) Peeling of the surface of the nevus with the formation of “dry” crusts;
11) The appearance of small pinpoint nodules on the surface of the mole;
12) The appearance of daughter pigmented or pink formations (satellites) in the skin around the nevus;
13) Change in the consistency of the nevus, that is, its softening or loosening;
14) The appearance of a shiny glossy surface;
15) Disappearance of the skin pattern on the surface of the mole.
Diagnosis of skin cancer
The diagnosis of skin cancer is made based on a number of examinations:
— visual examination: the appearance of the tumor, size, condition of nearby lymph nodes are assessed;
— a smear or scraping from a tumor is made by a doctor with a special instrument, the material taken is sent to a cytology laboratory for examination under a microscope; by the appearance of the cells, one or another skin tumor can be accurately determined or suspected. Under no circumstances should you scrape or injure tumors suspected of melanoma yourself, as this can cause the development of metastases.
- biopsy: taking a piece or the entire tumor for examination (total biopsy) for examination under a microscope;
- ultrasound examination of the tumor and nearby lymph nodes is used for more accurate diagnosis of the tumor and the presence of metastases;
— ultrasound examination of the abdominal organs is performed to exclude distant metastases to the abdominal organs;
- X-ray of the lungs: to exclude metastases to the lungs.
Stages of skin cancer:
Stage 1: tumor size does not exceed 2 cm;
Stage 2: tumor size from 2 to 5 cm;
Stage 3: tumor size is more than 5 cm or there is metastatic damage to nearby lymph nodes (for example, for tumors of the skin of the shoulder - damage to the axillary lymph nodes);
Stage 4: the tumor grows into nearby organs (muscles, bones, cartilage) or distant metastases are detected.
This classification is not applicable for melanoma; for it, staging is used according to the depth of germination into the skin and underlying tissues.
Survival for skin cancer is certainly different at different stages: with the first 2 stages, the prognosis is much better and survival rate reaches 100%, with 3-4 stages the survival rate sharply decreases to 70% or less. As for melanoma, even in the initial stages the prognosis is not always positive; this tumor can quickly metastasize to any internal organs and the brain.
Skin cancer treatment
In the treatment of skin cancer, like any malignant tumor, the leading role belongs to the surgical method. Removal of the tumor within healthy tissue is the key to long-term survival and absence of relapses.
For the treatment of skin basal cell carcinomas, especially on the face, where there is not much skin and it is difficult to achieve a good cosmetic effect, radiation therapy at a dose of 40-50 Gy is successfully used. In addition, radiation therapy can be used to treat squamous cell skin cancer. In weakened, elderly patients, chemotherapy ointments were previously used, but they have now been replaced by more effective methods, such as surgery and radiation.
In the presence of metastases of skin cancer, if it is impossible to completely remove them, chemotherapy is used, and it is also used in the presence of metastases in nearby lymph nodes, to prevent relapses of the disease.
In the treatment of skin melanomas, a surgical method is also used; in the presence of metastases, various chemotherapy regimens are possible, but the effect of them is insignificant, since the tumor is practically insensitive to any of the modern chemotherapy drugs. Radiation treatment is not used for melanoma, since the tumor is not sensitive to it.
Treatment with folk remedies is unacceptable, especially in the case of melanoma, since any compresses and lotions can dramatically increase tumor growth.
Complications of skin cancer
Complications of skin cancer may include: development of infection (suppuration); bleeding from the tumor, germination of vital organs by the tumor (large vessels, eyeball, meninges and brain tissue when the tumor is localized on the head and in advanced cases).
Preventing skin cancer
Prevention of skin cancer and melanoma mainly consists of reducing sun exposure, especially in fair-skinned people, and in hot countries with a scorching and unusual climate. You should also avoid occupational injuries and skin damage (chemicals, metals, arsenic).
Consultation with a doctor on skin cancer and melanoma:
Question: How common is skin cancer?
Answer: This is the most common tumor, especially basal cell carcinoma. These tumors are found everywhere after 60 years of age; many patients do not pay attention to them, since the growth of the tumor is slow and does not cause concern.
Question: What is melanoma and why is it dangerous?
Answer: Melanoma is an extremely malignant pigmented tumor of the skin and mucous membranes. It is dangerous due to its aggressive growth and rapid metastasis to both nearby lymph nodes and internal organs. Melanoma metastases can quickly lead to exhaustion and death of patients, even with the use of the entire arsenal of modern medical means.
Melanoma is considered one of the most insidious human malignant tumors, the morbidity and mortality from which is steadily increasing from year to year. They talk about it on TV, write in magazines and on the Internet. The interest of ordinary people is due to the fact that the tumor is increasingly being detected in residents of various countries, and the number of deaths is still high, even despite intensive treatment.
In terms of prevalence, melanoma lags significantly behind epithelial skin tumors (squamous cell carcinoma, basal cell carcinoma, etc.), according to various sources, accounting for 1.5 to 3% of cases, but it is much more dangerous. Over the 50 years of the last century, the incidence increased by 600%. This figure is enough to seriously fear the disease and look for the causes and methods of treating it.

What it is?
Melanoma is a malignant tumor that develops from melanocytes—pigment cells that produce melanin. Along with squamous cell and basal cell skin cancer, it is a malignant skin tumor. It is predominantly localized in the skin, less commonly in the retina and mucous membranes (oral cavity, vagina, rectum).
One of the most dangerous human malignant tumors, often recurrent and metastasizing through the lymphogenous and hematogenous route to almost all organs. A peculiarity is the body’s weak response or its absence, which is why melanoma often progresses rapidly.
Causes
Let's look at the main reasons that cause the development of melanoma:
- Prolonged and frequent exposure to ultraviolet radiation on the skin. The sun at its zenith is especially dangerous. This also includes exposure to artificial sources of ultraviolet radiation (solariums, bactericidal lamps, etc.).
- Traumatic lesions of age spots, nevi, especially in those places where there is constant contact with clothing and other environmental factors.
- Traumatic lesions of moles.
Melanoma develops from moles or nevi in 60% of cases. That's quite a lot. The main places where melanomas develop are such parts of the body as: head; neck; hands; legs; back; breast; palms; soles; scrotum.
People who have more than one of the following risk factors are most likely to get melanoma:
- A history of sunburn.
- Presence of skin diseases, skin cancer, melanoma in the family.
- Genetically determined red hair color, the presence of freckles and also fair skin.
- Light, almost white skin, due to genetic characteristics, low content of melanin pigment in the skin.
- The presence of age spots and nevi on the body. But, if hair grows on the nevus, then this area of the skin cannot degenerate into a malignant form.
- The presence of a large number of moles on the body. It is believed that if there are more than 50 moles, then this can already be dangerous.
- Old age, but recently melanoma is becoming more common in young people.
- The presence of skin diseases that can trigger the development of melanoma. These are diseases such as Dubreuil's melanosis, xeroderma pigmentosum and some others.
If a person belongs to any group from the above list, then he should be very careful in the sun and attentive to his health, since he has a fairly high probability of developing melanoma.

Statistics
According to WHO, in 2000, more than 200,000 cases of melanoma were diagnosed worldwide and 65,000 melanoma-related deaths occurred.
In the period from 1998 to 2008, the increase in the incidence of melanoma in the Russian Federation was 38.17%, and the standardized incidence rate increased from 4.04 to 5.46 per 100,000 population. In 2008, the number of new cases of skin melanoma in the Russian Federation amounted to 7,744 people. The mortality rate from melanoma in the Russian Federation in 2008 was 3159 people, and the standardized mortality rate was 2.23 people per 100,000 population. The average age of melanoma patients diagnosed for the first time in their lives in 2008 in the Russian Federation was 58.7 years[3]. The highest incidence was observed at the age of 75-84 years.
In 2005, the United States recorded 59,580 new cases of melanoma and 7,700 deaths due to this tumor. In SEER (The Surveillance, Ep >
Clinical types
In fact, there are a considerable number of melanomas, including blood melanoma, nail melanoma, lung melanoma, choroidal melanoma, non-pigmented melanoma and others, which develop over time in different parts of the human body due to the course of the disease and metastases, but in medicine the following are distinguished: main types of melanomas:
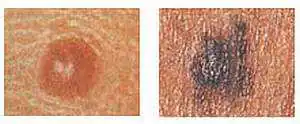
- Superficial or superficial melanoma. This is the more common type of tumor (70%). The course of the disease is characterized by prolonged, relatively benign growth in the outer layer of the skin. With this type of melanoma, a spot appears with jagged edges, the color of which can change: tan brown, red, black, blue or even white.
- Nodular (nodular) melanoma is in second place in the number of diagnosed patients (15-30% of cases). Most common in people over 50 years of age. Can form on any part of the body. But, as a rule, such tumors appear in women - on the lower extremities, in men - on the body. Often nodular melanoma forms against the background of a nevus. Characterized by vertical growth and aggressive development. Develops in 6-18 months. This type of tumor has a round or oval shape. Patients often consult a doctor when melanoma has already taken the form of a black or black-blue plaque, which has clear boundaries and raised edges. In some cases, nodular melanoma grows to a large size, or takes the form of a polyp that has ulcerations and is characterized by hyperactivity.
- Lentiginous melanoma. This form of the disease is also known as lentigo maligna or Hutchinson's freckle. Most often it is formed from an age-related pigment spot, a birthmark, or less often from an ordinary mole. This type of tumor is prone to forming in those areas of the body that are most exposed to solar ultraviolet radiation, such as the face, ears, neck, and hands. This melanoma develops very slowly in most sick people, sometimes it can take up to 30 years to reach the final stage of its development. Metastasis occurs rarely, and there is evidence of resorption of this formation, therefore lentiginous melanoma is considered the most favorable skin cancer in terms of prognosis.
- Lentigo maligna is similar to superficial melanoma. Development is long, in the upper layers of the skin. In this case, the affected area of the skin is flat or slightly raised, unevenly colored. The color of such a spot is patterned with brown and dark brown components. This melanoma often occurs in older people due to constant exposure to sunlight. Lesions appear on the face, ears, arms, and upper torso.

Melanoma symptoms
In the initial stage of development of a malignant tumor on healthy skin, and even more so against the background of a nevus, there are few obvious visual differences between them. Benign birthmarks are characterized by:
- Symmetrical shape.
- Smooth, even outlines.
- Uniform pigmentation, giving the formation a color ranging from yellow to brown and even sometimes black.
- A flat surface that is flush with the surface of the surrounding skin or slightly evenly raised above it.
- No increase in size or slight growth over a long period of time.
The main symptoms of melanoma are as follows:
- Hair loss from the surface of the nevus is caused by the degeneration of melanocytes into tumor cells and the destruction of hair follicles.
- Itching, burning and tingling in the area of pigment formation is caused by increased cell division within it.
- Ulcers and/or cracks, bleeding, or oozing are caused by the tumor destroying normal skin cells. Therefore, the top layer bursts, exposing the lower layers of skin. As a result, at the slightest injury, the tumor “explodes” and its contents pour out. In this case, cancer cells enter healthy skin, penetrating into it.
- An increase in size indicates increased cell division within the pigment formation.
- Uneven edges and thickening of the mole are a sign of increased division of tumor cells, as well as their germination into healthy skin.
- The appearance of “daughter” moles or “satellites” near the main pigment formation is a sign of local metastasis of tumor cells.
- The appearance of redness in the form of a corolla around the pigment formation is inflammation, indicating that the immune system has recognized tumor cells. Therefore, she sent special substances (interleukins, interferons and others) to the tumor site, which are designed to fight cancer cells.
- The disappearance of the skin pattern is caused by the tumor destroying the normal skin cells that form the skin pattern.
- Signs of eye damage: dark spots appear on the iris of the eye, visual disturbances and signs of inflammation (redness), there is pain in the affected eye.
- Color change:
1) Strengthening or the appearance of darker areas on the pigment formation is due to the fact that the melanocyte, degenerating into a tumor cell, loses its processes. Therefore, the pigment, unable to leave the cell, accumulates.
2) Clearing is due to the fact that the pigment cell loses the ability to produce melanin.
Each “birthmark” goes through the following stages of development:
- Borderline nevus, which is a spotty formation, the nests of cells of which are located in the epidermal layer.
- Mixed nevus - cell nests migrate into the dermis over the entire area of the spot; clinically, such an element is a papular formation.
- Intradermal nevus - the formation cells completely disappear from the epidermal layer and remain only in the dermis; gradually the formation loses pigmentation and undergoes reverse development (involution).
Stages
The course of melanoma is determined by the specific stage to which the patient’s condition corresponds at a particular moment; there are five of them in total: stage zero, stages I, II, III and IV. Stage zero allows you to identify tumor cells exclusively within the outer cell layer; their germination to deep-lying tissues does not occur at this stage.
- Melanoma in the early stages. Treatment involves local excision of the tumor within normal, healthy tissue. The total amount of healthy skin that must be removed depends on the depth of disease penetration. Removing lymph nodes near the melanoma does not increase the survival rate of people with stage I melanoma;
- Stage 2. In addition to excision of the formation, a biopsy of regional lymph nodes is performed. If a malignant process is confirmed during sample analysis, the entire group of lymph nodes in this area is removed. Additionally, alpha interferons can be prescribed for prevention purposes.
- Stage 3. In addition to the tumor, all lymph nodes that are located nearby are excised. If there are several melanomas, all of them must be removed. Radiation therapy is performed in the affected area, immunotherapy and chemotherapy are also prescribed. As we have already noted, relapses of the disease cannot be ruled out even with correctly defined and administered treatment. A pathological process can return either to an area that was previously damaged or to form in a part of the body that was not related to the previous course of the process.
- Stage 4. At this stage, melanoma patients cannot be completely cured. With the help of surgical operations, large tumors that cause extremely unpleasant symptoms are removed. It is extremely rare that metastases are removed from organs, but this directly depends on their location and symptoms. Chemotherapy and immunotherapy are often used in this case. Forecasts at this stage of the disease are extremely disappointing and on average amount to up to six months of life for people who develop melanoma and reach this stage. In rare cases, people diagnosed with stage 4 melanoma live several more years.
The main complication of melanoma is the spread of the pathological process through metastases.
Postoperative complications include the appearance of signs of infection, changes in the postoperative incision (swelling, bleeding, discharge) and pain. At the site of the removed melanoma or on healthy skin, a new mole may develop or discoloration of the skin may occur.

Metastasis
Malignant melanoma is prone to fairly pronounced metastasis, not only through the lymphogenous route, but also through the hematogenous route. The brain, liver, lungs, and heart are predominantly affected, as we have already noted. In addition, dissemination (spread) of tumor nodes along the skin of the torso or limb often occurs.
The option cannot be ruled out in which the patient seeks the help of a specialist solely on the basis of actual enlargement of the lymph nodes in any area. Meanwhile, a thorough survey in this case can determine that a certain time ago, for example, he, in order to achieve the appropriate cosmetic effect, removed a wart. This “wart” actually turned out to be melanoma, which was subsequently confirmed by the results of histological examination of the lymph nodes.
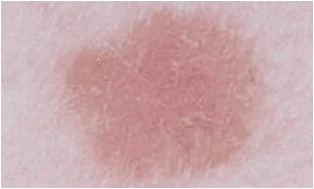
What melanoma looks like, photo
The photo below shows how the disease manifests itself in humans in the initial and other stages.

Melanoma may appear as a flat pigmented or non-pigmented spot with a slight elevation, round, polygonal, oval or irregular in shape with a diameter greater than 6 mm. It can maintain a smooth shiny surface for a long time, on which small ulcerations, unevenness, and bleeding subsequently occur with minor trauma.
Pigmentation is often uneven, but more intense in the central part, sometimes with a characteristic rim of black color around the base. The color of the entire neoplasm can be brown, black with a bluish tint, purple, variegated in the form of individual unevenly distributed spots.
Diagnostics
A doctor can suspect melanoma based on the patient’s complaints and visual examination of the changed skin. To confirm the diagnosis:
- Dermatoscopy is an examination of an area of skin under a special device. This examination helps to examine the edges of the spot, its growth in the epidermis, and internal inclusions.
- Biopsy – taking a tumor sample for histological examination.
- Ultrasound and computed tomography are prescribed to detect metastases and to determine the stage of cancer.
If necessary, and to exclude other skin diseases, the doctor may prescribe a number of diagnostic procedures and blood tests. The effectiveness of their elimination largely depends on the accuracy of diagnosing melanomas.
How to treat melanoma?
In the initial stage of melanoma, surgical excision of the tumor is mandatory. It can be economical, with removal of no more than 2 cm of skin from the edge of the melanoma, or wide, with resection of skin up to 5 cm around the border of the neoplasm. There is no single standard in the surgical treatment of stage I and II melanoma in this regard. Wide excision of melanoma guarantees a more complete removal of the tumor focus, but at the same time it may cause a recurrence of cancer at the site of the formed scar or transplanted skin flap. The type of surgical treatment for melanoma depends on the type and location of the tumor, as well as the patient's decision.
Part of the combined treatment of melanoma is preoperative radiation therapy. It is prescribed in the presence of ulcerations on the tumor, bleeding and inflammation in the area of the tumor. Local radiation therapy suppresses the biological activity of malignant cells and creates favorable conditions for surgical treatment of melanoma.
Radiation therapy is rarely used as an independent method of treating melanoma. And in the preoperative period of treatment of melanoma, its use has become common practice, since excision of the tumor can be carried out literally the next day after the end of the course of radiation therapy. The interval for recovery of the body between two types of treatment for symptoms of skin melanoma is usually not maintained.

Forecast for life
The prognosis for melanoma depends on the time of detection and the degree of tumor progression. When detected early, most melanomas respond well to treatment.
Melanoma that has grown deeply or has spread to the lymph nodes increases the risk of recurrence after treatment. If the depth of the lesion exceeds 4 mm or there is a lesion in the lymph node, then there is a high probability of metastasis to other organs and tissues. When secondary lesions appear (stages 3 and 4), treatment of melanoma becomes ineffective.
- Survival rates for melanoma vary widely depending on the stage of the disease and the treatment provided. In the initial stage, cure is most likely. Also, cure can occur in almost all cases of stage 2 melanoma. Patients treated in the first stage have a 95 percent five-year survival rate and 88 percent ten-year survival rate. For the second stage, these figures are 79% and 64%, respectively.
- In stages 3 and 4, the cancer has spread to distant organs, resulting in a significantly reduced survival rate. The five-year survival rate of patients with stage 3 melanoma ranges (according to various sources) from 29% to 69%. Ten-year survival is achieved in only 15 percent of patients. If the disease has progressed to stage 4, then the chance of five-year survival is reduced to 7-19%. There are no 10-year survival statistics for patients with stage 4.
The risk of melanoma recurrence increases in patients with a large tumor thickness, as well as in the presence of ulcerations of melanoma and nearby metastatic skin lesions. Recurrent melanoma can occur either in close proximity to the previous site or at a considerable distance from it.
A malignant tumor that is localized in the basal layer of the skin and spreads to healthy skin is called melanoma. Its development is ensured by pigment cells that have degenerated into cancer cells.
This disease appears due to the degeneration of an ordinary and harmless (at first glance) nevus or mole on various parts of the human body or in the mucous membrane. It proceeds aggressively and quickly. Melanoma affects both men and women aged 35 to 50 years.
Doctors are not always able to diagnose this disease at an early stage. It is detected when metastasis appears. This is why it is difficult, and in some cases impossible, to cure melanoma.
What does skin melanoma look like in photographs?
Signs of skin melanoma are specific. They are directly dependent on the form and stage of the disease. It looks like small nodules or plaques on the surface of the skin of any part of the body, which are very similar to moles. Malignant cells grow deep and wide in the skin, reaching a diameter of 10 centimeters.
If the diagnosis is made at the initial stage, then there may be no symptoms, but in the third or fourth stages the following signs of skin melanoma are already obvious:
- a sharp deterioration in health;
- the body is subjected to severe intoxication;
- moles begin to grow rapidly, changing in shape and color.
The disease can be identified if you conduct your own examination. You should urgently visit an oncologist when:
- the mole began to increase in size, changed color (turned pale or darkened, the color became uneven), and its edges became uneven and asymmetrical;
- tingling or itching is felt in the abdomen (cells are dividing intensively);
- a red, inflamed border appeared around the spot;
- the mole festers;
- more spots appeared;
- the nevus became dense and uneven.
When the disease reaches the fourth stage, bleeding from the nevus is observed, the epidermis becomes damaged, the mole itches, hurts, and pigment grows around it. All these signs indicate the spread of the disease and metastases.
Also, signs of skin melanoma can be: the patient has a very bad headache and joints, enlarged lymph nodes, decreased vision, cough and lumps under the skin. The patient loses weight sharply.
A malignant neoplasm is not necessarily dark in color, which makes diagnosis difficult.
If you take a photo of skin melanoma with a certain time interval, you can see how the tumor grows and changes its size.

What skin melanoma looks like in the photo

Photo of skin melanoma on the left - the color is uniform, image on the right - there is a color change in one element

Photo on the left - the edges are smooth, photo on the right - the border is not clear
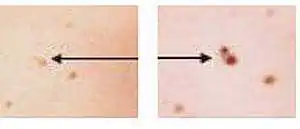
The image on the left is just a mole, the image on the right is changed in size, shade and shape
The image on the left is a symmetrical mole (normal), the image on the right is what skin melanoma looks like
This disease occurs not only on the skin of the body, but also on the nails, limbs, and face.

Nail affected by melanoma
A line along the nail plate that is brown or dark in color is considered by doctors to be malignant melanoma, especially when the unevenness of the edge and its thickening are noticeable.
Skin melanoma can also occur on the face, since it is most often exposed to sunlight, so there is a high risk of tumors appearing.

Facial skin melanoma
Diagnosis of skin melanoma on the face and other parts of the body is carried out using several examinations by an oncologist:
- examination (assessing the appearance of the tumor, determining its size, palpating the nearest lymph nodes;
- taking a smear or scraping from a problem area on the face with a special instrument, sending the material to a cytology laboratory for examination under a microscope;
- taking a biopsy (part or the entire tumor) for microscopic examination;
- Ultrasound of the tumor and nearby lymph nodes;
- Ultrasound of the abdominal cavity to detect metastases in internal organs;
- X-ray of the lungs to determine the presence or absence of metastasis to the lungs.
Skin melanoma: forecasts
Skin melanoma has prognoses for later life that directly depend on the stage of the disease, as well as on the medical measures performed (surgery, radiation therapy, chemotherapy, immunological treatment). The disease is well treated if it is detected at the initial (95% of patients survive for 5 years, 88% for 10 years) and second (79% of patients will survive for 5 years, 64% for 10 years) stages.
A tumor that has grown deeply (more than 4 millimeters) or has reached the lymph nodes can metastasize or appear again after therapeutic measures. Treatment will not work if the disease is in the third or fourth stage, due to its spread to the internal organs. In the third stage, 29-69% of people will survive for 5 years, only 15% of patients will survive for 10 years. At the fourth stage, the five-year survival rate is from 7% to 19%.
]After successful treatment (even if years have passed), it is necessary to be examined regularly so that a relapse does not occur. Recurrence of the tumor may occur if it was thick.
In case of relapse, the prognosis for recovery can be favorable if treatment is started on time.
How is skin melanoma prevented?
Preventive measures for the disease are:
- limiting exposure to direct sunlight (especially important for those with fair skin);
- stop visiting the solarium if there is a tendency to develop moles;
- prevention of epidermal injuries associated with professional activities;
- avoiding the influence of heavy metal salts, arsenic and other chemicals on the skin;
- absence of bad habits;
- healthy eating.
It should be remembered that only the initial stage of the disease can be cured, so if symptoms are detected, you must immediately seek medical help. It is prohibited to remove or injure a tumor (mole) yourself, otherwise metastases will occur!
Skin melanoma code according to ICD 10
Skin melanoma according to ICD 10 (international classification of diseases) has code C43. It is divided into 10 malignant melanomas:
- lips (C43.0);
- eyelid, eyelid commissure (C43.1);
- ear, external auditory canal (C43.2);
- other and unspecified facial parts (C43.3);
- neck and part of the head where hair grows (C43.4);
- torso (C43.5);
- upper limbs, shoulder joint area (C43.6);
- lower extremities, hip joint area (C43.7);
- other parts of the epidermis (C43.8);
- unaccounted for (C43.9).



