Synovitis, its causes, types and symptoms. Diagnostic methods, drug and surgical treatment. Danger of the disease, prognosis for the patient.
The content of the article:- Causes of synovitis
- Main symptoms
- Diagnostic methods
- Treatment methods
- Medicines
- Physiotherapy
- Surgical intervention
- Complications and prevention
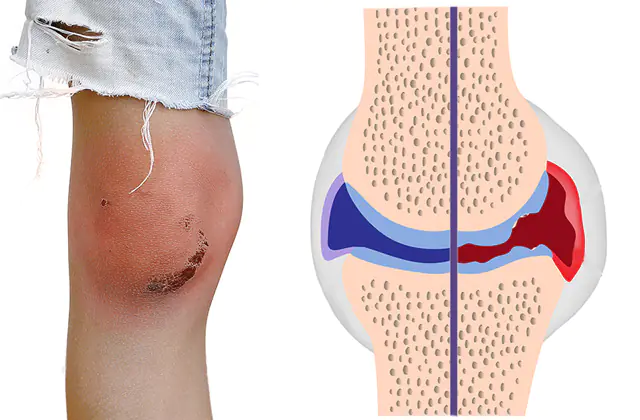
Synovitis is an inflammation of the inner lining of the joint capsules, which occurs as a result of injuries and overexertion or as a reaction to exposure to an infectious pathogen. Affects the hip, shoulder, ankle, wrist, knee and elbow joints. If left unattended, it can lead to degenerative changes in cartilage and bone erosion.
Main causes of synovitis

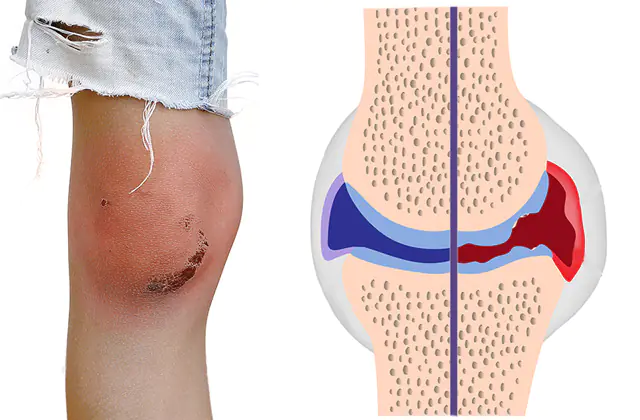
The movable joints of bones in the human body are surrounded by a joint capsule - a dense tissue bag, the inner layer of which produces shock-absorbing fluid. Inflammation of this inner (synovial) layer is called synovitis of the joint. The inflamed joint membrane swells and begins to abundantly generate pathological fluid - effusion or exudate.
Typically, synovitis appears as a secondary symptom against the background of another disease - for example, gout, rheumatism or systemic lupus erythematosus. The nature of the course can be subclinical (without pronounced symptoms), acute and chronic. The transition to a chronic form is judged by the degeneration of joint tissue - the thin synovial membrane is replaced by a thickened fibrous one.
Depending on the source of inflammation, synovitis is divided into two broad categories:
- Infectious. Inflammation is caused by pathological microorganisms that enter the joint capsule through the bloodstream or during injury. As a rule, these are bacteria (staphylococci, streptococci, gonococci), less often - viruses (influenza, hepatitis C) or mycobacteria (Koch bacillus). Synovitis caused by a pathogen of a specific disease is called specific.
- Aseptic. It develops from frequent extreme loads on the joint, under the influence of allergens, disruption of the endocrine system, and also as an autoimmune reaction of the body in certain diseases of the musculoskeletal system.
Main symptoms of synovitis
The main symptom of synovitis is pain in the affected joint. With traumatic inflammation, pain is localized in the same joint. Secondary forms that arise against the background of other diseases can be characterized by wandering pain, affecting several different joints at different times.
Externally, the affected joint will look swollen and red. When palpated, it is warmer than the surrounding tissues. There are difficulties in its operation: the patient cannot fully straighten or bend it. There is a general malaise - weakness, fever up to 38.5°C.
In the subclinical form, pain and external changes in the joint may be absent, while pathological changes can be noticed using ultrasound or magnetic resonance imaging.
Sometimes pain may be the only symptom, while the affected joint will look absolutely normal for some time - without redness or increase in size.
Methods for diagnosing synovitis

The acute form of synovitis can be diagnosed already during the initial examination by a doctor - by palpating the affected joint. Fluid accumulations are clearly visible on MRI, as well as using ultrasound scanning. When making a diagnosis, it is important to timely distinguish synovitis from tendonitis - inflammation of the tendons adjacent to the joint, which has similar external symptoms.
Since the cause of synovitis is almost always another disease, a set of diagnostic procedures may also include allergy tests or blood tests.
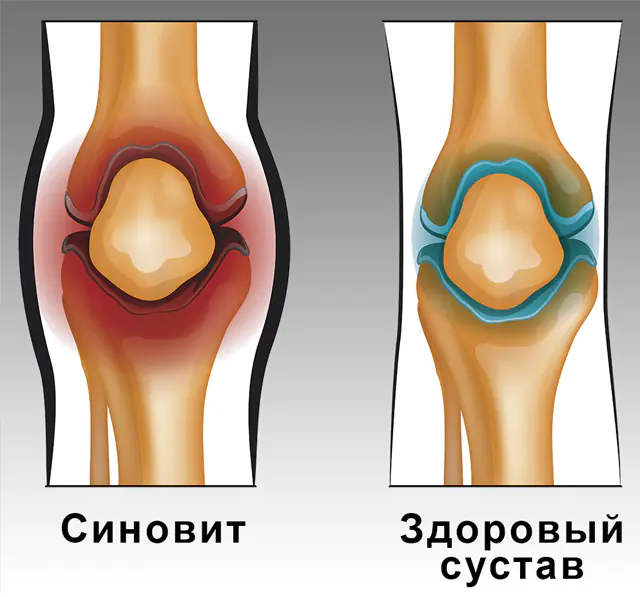
In case of confirmed synovitis, arthroscopy may be prescribed: under local anesthesia, an arthroscope, a surgical instrument, is inserted into the area of the damaged joint through a micro-incision, with the help of which it is possible to diagnose its diseases and carry out the necessary reconstructive operations. An arthroscope is a small tube with a built-in high-definition camera that allows the surgeon to work on the joints without having to open them completely.
Laboratory analysis of the contents of the synovial bursa plays a key role in differential diagnosis. The liquid is taken through a puncture - an injection into the damaged joint using local anesthesia. Most often, such a puncture is performed for synovitis of the knee joint. The procedure is performed on an empty stomach.
In the laboratory, the material taken is examined for several indicators:
- The physicochemical properties of the liquid (color, pH, turbidity, viscosity, volume) will indicate the severity of inflammation and possible hemorrhage into the joint;
- The presence of pathological elements and inclusions can indicate a specific primary pathology that caused inflammation (for example, with gout, crystals of uric acid salts will be observed in the synovial fluid);
- The presence of cellular elements above the permissible norm (cytosis) allows one to judge the rate of development of inflammation and helps in differential diagnosis;
- An increase in the level of glucose and lactic acid in the synovial fluid indicates a possible infection of the joint capsule;
- If infectious synovitis is suspected, a bacteriological analysis is performed to determine the presence of pathogenic microorganisms in the fluid.
Rarer forms of the disease are synovitis of the ankle and hip joint. If the latter is suspected, during examination the patient is asked to spread his legs in a lying position. The movement of an inflamed hip will be limited compared to a healthy one.
It is also possible to perform a biopsy (taking a tissue sample) of the bursa. The procedure is carried out either by puncture or using an arthroscope.
Methods for treating synovitis
As with the treatment of any inflammatory process, the treatment of synovitis involves a multifaceted approach: stopping inflammation, eliminating any pathogens and restoring the body after the disease. Your doctor will tell you how to treat synovitis and whether surgical intervention is always necessary.
Medicines for synovitis

Complex drug therapy for synovitis is prescribed to perform several tasks: relieving inflammation, pain relief, disinfecting the joint during an infectious disease, resolving the primary condition that became the source of inflammation. Each of these problems is solved with the help of a drug of a certain pharmacotherapeutic group.
Effective drugs for synovitis:
- NSAIDs (non-steroidal anti-inflammatory drugs)- to suppress pain and inflammation. Such drugs include Diclofenac, Ibuprofen and acetylsalicylic acid. Voltaren (analogue - Diklak) is an example of diclofenac ointment for synovitis. A 50-gram tube of this medicine will cost you 500 rubles. (170-200 UAH).
- Glucocorticoids- used for drug blockade for recurrent synovitis. A package of Betaspan (Depos) injection solution is relatively expensive - 1,200 rubles. (300-500 UAH).
- Antibiotics- in the fight against infectious synovitis. Lincomycin (analogue - Dalatsin) is administered in combination with Novocaine. All necessary solutions can be purchased for 170 rubles. (50-70 UAH).
In addition, appropriate specific drugs are prescribed for the treatment of primary synovitis.
Physiotherapy in the treatment of synovitis

Treatment of synovitis with medications is carried out in combination with physiotherapeutic procedures. During free time from procedures, the joint should be kept at rest and immobilized. If the knee joint is inflamed, the leg must be completely straightened and fixed in an elevated position. In case of inflammation of the ankle, a fixing pressure bandage is applied.
Depending on the affected joint and accompanying phenomena, massage, electrophoresis (Novocaine), UHF therapy may be prescribed:
- electrophoresis- introduction of a medicinal substance through the skin using electrodes;
- UHF therapy— stimulation of blood flow and immune system through an electromagnetic field.
Surgical intervention for synovitis
Inflammation of the joint capsule responds well to drug treatment, however, some severe (chronic and purulent) cases may require urgent surgical intervention.
Arthroscopy is a minimally invasive procedure, a surgical procedure performed under general or local anesthesia to insert an arthroscope. It can be produced for both diagnostic and therapeutic purposes. You can return home after such an operation either on the same day or the next.
Punctures of synovial contents are usually carried out for diagnostic purposes, but if there is a significant accumulation of effusion in the joint capsule, therapeutic punctures will also be indicated. This method is especially often used for infectious synovitis: depending on the severity of inflammation, suppuration is pumped out either using a puncture or by drainage.
A major surgical intervention is the operation of excision (partial or complete removal) of the synovial membrane of the joint - synovectomy. Prescribed when conservative treatment fails and inflammation becomes chronic.
Under general anesthesia, the muscle covering the affected joint is dissected, the joint capsule is opened, after which the synovial layer is partially or completely removed. As a rule, complete removal is performed in case of rheumatoid joint damage.
Upon completion of the operation, a plaster is applied, which will need to be kept in place for about a month after the initial (3-4 days) replacement. In addition, the operated joint must be regularly developed using a functional splint.
Important! The effectiveness of alternative treatment for synovitis has not been proven; the severity of the inflammation can only be aggravated. The disease is easily amenable to traditional therapy: under the influence of ordinary anti-inflammatory drugs, the disease, not complicated by external factors, recedes. Do not self-medicate or use folk remedies for synovitis: if you experience dull “wandering” pain in the joints or persistent discomfort that manifests itself during extension, be sure to consult a rheumatologist.Complications and prevention of synovitis

The inflamed synovium becomes fibrous over time and begins to replace surrounding tissue, including causing cartilage destruction and bone erosion. Erosive synovitis especially often develops against the background of rheumatoid arthritis.
Any form of synovitis is fraught with possible loss of joint mobility. Aseptic synovitis, left unattended, can lead to dislocations over time.
Infectious synovitis can extend beyond the joint capsule and cause phlegmon (extensive purulent inflammation without clear boundaries) or panarthritis (purulent inflammation of all joint tissues).
In rare cases, infectious synovitis can cause blood poisoning.
Inflammation of the joint capsule is a secondary phenomenon, and in the prevention of synovitis, attention should be paid, first of all, to the prevention of diseases and conditions in which inflammation tends to manifest itself. The risk group is primarily people who have already been diagnosed with any disease of the musculoskeletal system.
Limiting the influence of allergens, observing safety precautions during physical activity, as well as hygiene rules will reduce the risk of getting sick. After recovery, it is recommended, together with your doctor, to develop a set of exercises to strengthen and restore normal mobility of the affected joint.
Video on the topic of what is synovitis of the knee joint and how to treat it: