Melanoma is considered one of the most insidious human malignant tumors, the morbidity and mortality from which is steadily increasing from year to year. They talk about it on TV, write in magazines and on the Internet. The interest of ordinary people is due to the fact that the tumor is increasingly being detected in residents of various countries, and the number of deaths is still high, even despite intensive treatment.
In terms of prevalence, melanoma lags significantly behind epithelial skin tumors (squamous cell carcinoma, basal cell carcinoma, etc.), according to various sources, accounting for 1.5 to 3% of cases, but it is much more dangerous. Over the 50 years of the last century, the incidence increased by 600%. This figure is enough to seriously fear the disease and look for the causes and methods of treating it.

What it is?
Melanoma is a malignant tumor that develops from melanocytes—pigment cells that produce melanin. Along with squamous cell and basal cell skin cancer, it is a malignant skin tumor. It is predominantly localized in the skin, less commonly in the retina and mucous membranes (oral cavity, vagina, rectum).
One of the most dangerous human malignant tumors, often recurrent and metastasizing through the lymphogenous and hematogenous route to almost all organs. A peculiarity is the body’s weak response or its absence, which is why melanoma often progresses rapidly.
Causes
Let's look at the main reasons that cause the development of melanoma:
- Prolonged and frequent exposure to ultraviolet radiation on the skin. The sun at its zenith is especially dangerous. This also includes exposure to artificial sources of ultraviolet radiation (solariums, bactericidal lamps, etc.).
- Traumatic lesions of age spots, nevi, especially in those places where there is constant contact with clothing and other environmental factors.
- Traumatic lesions of moles.
Melanoma develops from moles or nevi in 60% of cases. That's quite a lot. The main places where melanomas develop are such parts of the body as: head; neck; hands; legs; back; breast; palms; soles; scrotum.
People who have more than one of the following risk factors are most likely to get melanoma:
- A history of sunburn.
- Presence of skin diseases, skin cancer, melanoma in the family.
- Genetically determined red hair color, the presence of freckles and also fair skin.
- Light, almost white skin, due to genetic characteristics, low content of melanin pigment in the skin.
- The presence of age spots and nevi on the body. But, if hair grows on the nevus, then this area of the skin cannot degenerate into a malignant form.
- The presence of a large number of moles on the body. It is believed that if there are more than 50 moles, then this can already be dangerous.
- Old age, but recently melanoma is becoming more common in young people.
- The presence of skin diseases that can trigger the development of melanoma. These are diseases such as Dubreuil's melanosis, xeroderma pigmentosum and some others.
If a person belongs to any group from the above list, then he should be very careful in the sun and attentive to his health, since he has a fairly high probability of developing melanoma.
Statistics
According to WHO, in 2000, more than 200,000 cases of melanoma were diagnosed worldwide and 65,000 melanoma-related deaths occurred.
In the period from 1998 to 2008, the increase in the incidence of melanoma in the Russian Federation was 38.17%, and the standardized incidence rate increased from 4.04 to 5.46 per 100,000 population. In 2008, the number of new cases of skin melanoma in the Russian Federation amounted to 7,744 people. The mortality rate from melanoma in the Russian Federation in 2008 was 3159 people, and the standardized mortality rate was 2.23 people per 100,000 population. The average age of melanoma patients diagnosed for the first time in their lives in 2008 in the Russian Federation was 58.7 years[3]. The highest incidence was observed at the age of 75-84 years.
In 2005, the United States recorded 59,580 new cases of melanoma and 7,700 deaths due to this tumor. In SEER (The Surveillance, Ep >
Clinical types
In fact, there are a considerable number of melanomas, including blood melanoma, nail melanoma, lung melanoma, choroidal melanoma, non-pigmented melanoma and others, which develop over time in different parts of the human body due to the course of the disease and metastases, but in medicine the following are distinguished: main types of melanomas:
- Superficial or superficial melanoma. This is the more common type of tumor (70%). The course of the disease is characterized by prolonged, relatively benign growth in the outer layer of the skin. With this type of melanoma, a spot appears with jagged edges, the color of which can change: tan brown, red, black, blue or even white.
- Nodular (nodular) melanoma is in second place in the number of diagnosed patients (15-30% of cases). Most common in people over 50 years of age. Can form on any part of the body. But, as a rule, such tumors appear in women - on the lower extremities, in men - on the body. Often nodular melanoma forms against the background of a nevus. Characterized by vertical growth and aggressive development. Develops in 6-18 months. This type of tumor has a round or oval shape. Patients often consult a doctor when melanoma has already taken the form of a black or black-blue plaque, which has clear boundaries and raised edges. In some cases, nodular melanoma grows to a large size, or takes the form of a polyp that has ulcerations and is characterized by hyperactivity.
- Lentiginous melanoma. This form of the disease is also known as lentigo maligna or Hutchinson's freckle. Most often it is formed from an age-related pigment spot, a birthmark, or less often from an ordinary mole. This type of tumor is prone to forming in those areas of the body that are most exposed to solar ultraviolet radiation, such as the face, ears, neck, and hands. This melanoma develops very slowly in most sick people, sometimes it can take up to 30 years to reach the final stage of its development. Metastasis occurs rarely, and there is evidence of resorption of this formation, therefore lentiginous melanoma is considered the most favorable skin cancer in terms of prognosis.
- Lentigo maligna is similar to superficial melanoma. Development is long, in the upper layers of the skin. In this case, the affected area of the skin is flat or slightly raised, unevenly colored. The color of such a spot is patterned with brown and dark brown components. This melanoma often occurs in older people due to constant exposure to sunlight. Lesions appear on the face, ears, arms, and upper torso.

Melanoma symptoms
In the initial stage of development of a malignant tumor on healthy skin, and even more so against the background of a nevus, there are few obvious visual differences between them. Benign birthmarks are characterized by:
- Symmetrical shape.
- Smooth, even outlines.
- Uniform pigmentation, giving the formation a color ranging from yellow to brown and even sometimes black.
- A flat surface that is flush with the surface of the surrounding skin or slightly evenly raised above it.
- No increase in size or slight growth over a long period of time.
The main symptoms of melanoma are as follows:
- Hair loss from the surface of the nevus is caused by the degeneration of melanocytes into tumor cells and the destruction of hair follicles.
- Itching, burning and tingling in the area of pigment formation is caused by increased cell division within it.
- Ulcers and/or cracks, bleeding or oozing are caused by the tumor destroying normal skin cells. Therefore, the top layer bursts, exposing the lower layers of skin. As a result, at the slightest injury, the tumor “explodes” and its contents pour out. In this case, cancer cells enter healthy skin, penetrating into it.
- An increase in size indicates increased cell division within the pigment formation.
- Uneven edges and thickening of the mole are a sign of increased division of tumor cells, as well as their germination into healthy skin.
- The appearance of “daughter” moles or “satellites” near the main pigment formation is a sign of local metastasis of tumor cells.
- The appearance of redness in the form of a corolla around the pigment formation is inflammation, indicating that the immune system has recognized tumor cells. Therefore, she sent special substances (interleukins, interferons and others) to the tumor site, which are designed to fight cancer cells.
- The disappearance of the skin pattern is caused by the tumor destroying the normal skin cells that form the skin pattern.
- Signs of eye damage: dark spots appear on the iris of the eye, visual disturbances and signs of inflammation (redness), there is pain in the affected eye.
- Color change:
1) Strengthening or the appearance of darker areas on the pigment formation is due to the fact that the melanocyte, degenerating into a tumor cell, loses its processes. Therefore, the pigment, unable to leave the cell, accumulates.
2) Clearing is due to the fact that the pigment cell loses the ability to produce melanin.
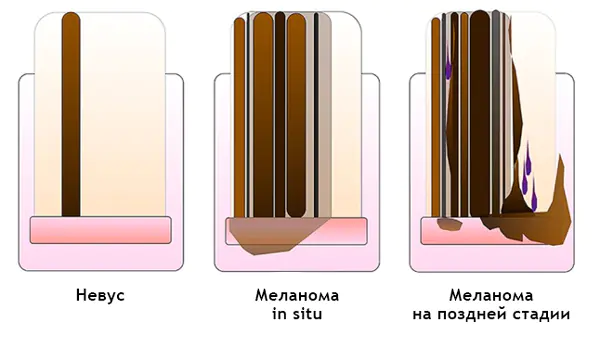
Each “birthmark” goes through the following stages of development:
- Borderline nevus, which is a spotty formation, the nests of cells of which are located in the epidermal layer.
- Mixed nevus - cell nests migrate into the dermis over the entire area of the spot; clinically, such an element is a papular formation.
- Intradermal nevus - the formation cells completely disappear from the epidermal layer and remain only in the dermis; gradually the formation loses pigmentation and undergoes reverse development (involution).
Stages
The course of melanoma is determined by the specific stage to which the patient’s condition corresponds at a particular moment; there are five of them in total: stage zero, stages I, II, III and IV. Stage zero allows you to identify tumor cells exclusively within the outer cell layer; their germination to deep-lying tissues does not occur at this stage.
- Melanoma in the early stages. Treatment involves local excision of the tumor within normal, healthy tissue. The total amount of healthy skin that must be removed depends on the depth of disease penetration. Removing lymph nodes near the melanoma does not increase the survival rate of people with stage I melanoma;
- Stage 2. In addition to excision of the formation, a biopsy of regional lymph nodes is performed. If a malignant process is confirmed during sample analysis, the entire group of lymph nodes in this area is removed. Additionally, alpha interferons can be prescribed for prevention purposes.
- Stage 3. In addition to the tumor, all lymph nodes that are located nearby are excised. If there are several melanomas, all of them must be removed. Radiation therapy is performed in the affected area, immunotherapy and chemotherapy are also prescribed. As we have already noted, relapses of the disease cannot be ruled out even with correctly defined and administered treatment. A pathological process can return either to an area that was previously damaged or to form in a part of the body that was not related to the previous course of the process.
- Stage 4. At this stage, melanoma patients cannot be completely cured. With the help of surgical operations, large tumors that cause extremely unpleasant symptoms are removed. It is extremely rare that metastases are removed from organs, but this directly depends on their location and symptoms. Chemotherapy and immunotherapy are often used in this case. Forecasts at this stage of the disease are extremely disappointing and on average amount to up to six months of life for people who develop melanoma and reach this stage. In rare cases, people diagnosed with stage 4 melanoma live several more years.
The main complication of melanoma is the spread of the pathological process through metastases.
Postoperative complications include the appearance of signs of infection, changes in the postoperative incision (swelling, bleeding, discharge) and pain. At the site of the removed melanoma or on healthy skin, a new mole may develop or discoloration of the skin may occur.

Metastasis
Malignant melanoma is prone to fairly pronounced metastasis, not only through the lymphogenous route, but also through the hematogenous route. The brain, liver, lungs, and heart are predominantly affected, as we have already noted. In addition, dissemination (spread) of tumor nodes along the skin of the torso or limb often occurs.
The option cannot be ruled out in which the patient seeks the help of a specialist solely on the basis of actual enlargement of the lymph nodes in any area. Meanwhile, a thorough survey in this case can determine that a certain time ago, for example, he, in order to achieve the appropriate cosmetic effect, removed a wart. This “wart” actually turned out to be melanoma, which was subsequently confirmed by the results of histological examination of the lymph nodes.
What melanoma looks like, photo
The photo below shows how the disease manifests itself in humans in the initial and other stages.

Melanoma may appear as a flat pigmented or non-pigmented spot with a slight elevation, round, polygonal, oval or irregular in shape with a diameter greater than 6 mm. It can maintain a smooth shiny surface for a long time, on which small ulcerations, unevenness, and bleeding subsequently occur with minor trauma.
Pigmentation is often uneven, but more intense in the central part, sometimes with a characteristic rim of black color around the base. The color of the entire neoplasm can be brown, black with a bluish tint, purple, variegated in the form of individual unevenly distributed spots.
Diagnostics
A doctor can suspect melanoma based on the patient’s complaints and visual examination of the changed skin. To confirm the diagnosis:
- Dermatoscopy is an examination of an area of skin under a special device. This examination helps to examine the edges of the spot, its growth in the epidermis, and internal inclusions.
- Biopsy - taking a tumor sample for histological examination.
- Ultrasound and computed tomography are prescribed to detect metastases and to determine the stage of cancer.
If necessary, and to exclude other skin diseases, the doctor may prescribe a number of diagnostic procedures and blood tests. The effectiveness of their elimination largely depends on the accuracy of diagnosing melanomas.
How to treat melanoma?
In the initial stage of melanoma, surgical excision of the tumor is mandatory. It can be economical, with removal of no more than 2 cm of skin from the edge of the melanoma, or wide, with resection of skin up to 5 cm around the border of the neoplasm. There is no single standard in the surgical treatment of stage I and II melanoma in this regard. Wide excision of melanoma guarantees a more complete removal of the tumor focus, but at the same time it may cause a recurrence of cancer at the site of the formed scar or transplanted skin flap. The type of surgical treatment for melanoma depends on the type and location of the tumor, as well as the patient's decision.
Part of the combined treatment of melanoma is preoperative radiation therapy. It is prescribed in the presence of ulcerations on the tumor, bleeding and inflammation in the area of the tumor. Local radiation therapy suppresses the biological activity of malignant cells and creates favorable conditions for surgical treatment of melanoma.
Radiation therapy is rarely used as an independent method of treating melanoma. And in the preoperative period of treatment of melanoma, its use has become common practice, since excision of the tumor can be carried out literally the next day after the end of the course of radiation therapy. The interval for recovery of the body between two types of treatment for symptoms of skin melanoma is usually not maintained.

Forecast for life
The prognosis for melanoma depends on the time of detection and the degree of tumor progression. When detected early, most melanomas respond well to treatment.
Melanoma that has grown deeply or has spread to the lymph nodes increases the risk of recurrence after treatment. If the depth of the lesion exceeds 4 mm or there is a lesion in the lymph node, then there is a high probability of metastasis to other organs and tissues. When secondary lesions appear (stages 3 and 4), treatment of melanoma becomes ineffective.
- Survival rates for melanoma vary widely depending on the stage of the disease and the treatment provided. In the initial stage, cure is most likely. Also, cure can occur in almost all cases of stage 2 melanoma. Patients treated in the first stage have a 95 percent five-year survival rate and 88 percent ten-year survival rate. For the second stage, these figures are 79% and 64%, respectively.
- In stages 3 and 4, the cancer has spread to distant organs, resulting in a significantly reduced survival rate. The five-year survival rate of patients with stage 3 melanoma ranges (according to various sources) from 29% to 69%. Ten-year survival is achieved in only 15 percent of patients. If the disease has progressed to stage 4, then the chance of five-year survival is reduced to 7-19%. There are no 10-year survival statistics for patients with stage 4.
The risk of melanoma recurrence increases in patients with a large tumor thickness, as well as in the presence of ulcerations of melanoma and nearby metastatic skin lesions. Recurrent melanoma can occur either in close proximity to the previous site or at a considerable distance from it.
Many people who discover a spot under their nail begin to search on the Internet to find out what it could be? And it turns out that this can be a fatal disease - subungual melanoma.
In this article we will look at:
- concept of subungual melanoma;
- the chances of this type of tumor occurring;
- photos of symptoms with histological confirmation;
- ways to distinguish subungual melanoma from hematoma;
- procedures to clarify the diagnosis;
- prognosis and treatment.
Subungual melanoma – what is it?
The share of melanoma among skin tumors is only 4%. But it is from this malignant neoplasm that 80% of patients with skin tumors die [1]. In Russia, about 8,717 people a year currently develop skin melanoma (data for 2012) [2]. Subungual melanoma is located in the nail bed and usually appears as a stripe on the nail.
What are the chances of this type of tumor occurring in a resident of Russia?
Of the total number of melanomas, the share of this tumor is only 2% [3], i.e., in absolute values, in 170 people per year. Against the background of the country's total population of 146,000,000, this, in my opinion, is very small. At the same time, a low incidence rate does not eliminate the possibility of getting sick.
For representatives of other skin phototypes other than 2, the chances may be very different. Representatives of the Mongoloid and Negroid races have a higher (up to 40%) chance of developing melanoma of the nail bed [4, 5].
Where does subungual melanoma appear most often?
The tumor most often affects the big toes [3].
What does subungual melanoma look like? Photos and signs.
All pictures below are histologically confirmed and not taken from the Internet. The source is indicated in square brackets. There are 2 most common signs:
Sign I
Most often, subungual melanoma appears as a brown or black stripe. The strip starts from the nail fold and ends at the edge of the nail. This condition is called longitudinal melanonychia. Some medications can cause such bands to appear - retinoids and Docetaxel (Taxotere) [10]. This sign can also occur in conditions not associated with melanoma, for example, with fungal infection of the nail, pigmented nevus of the nail bed.

Subungual pigmented nevus in a 13-year-old boy [9]

Subungual melanoma stage I, 0.2 mm according to Breslow [10]
Sign II
The most common symptom of this type of melanoma is Hutchinson's sign – transition of pigmentation to the nail fold or fingertip. This feature is visible in 7 of the 8 images below. At the same time, it cannot be stated unequivocally that this symptom occurs only with melanoma. It can also be observed with a transparent cuticle [10].
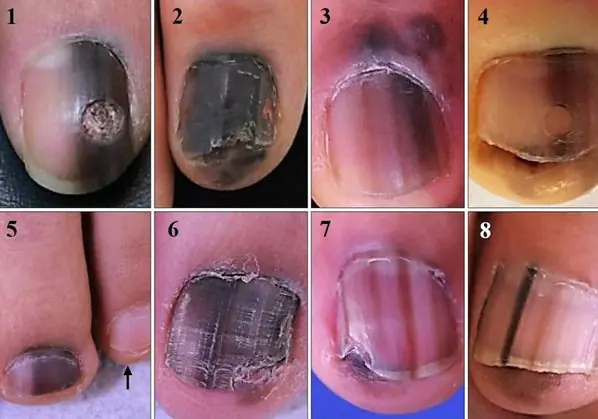
8 cases of subungual melanomas in situ (initial stage) [6]


Subungual melanoma of the thumb with level 4 invasion according to Clark, thickness according to Breslow is not specified [8]
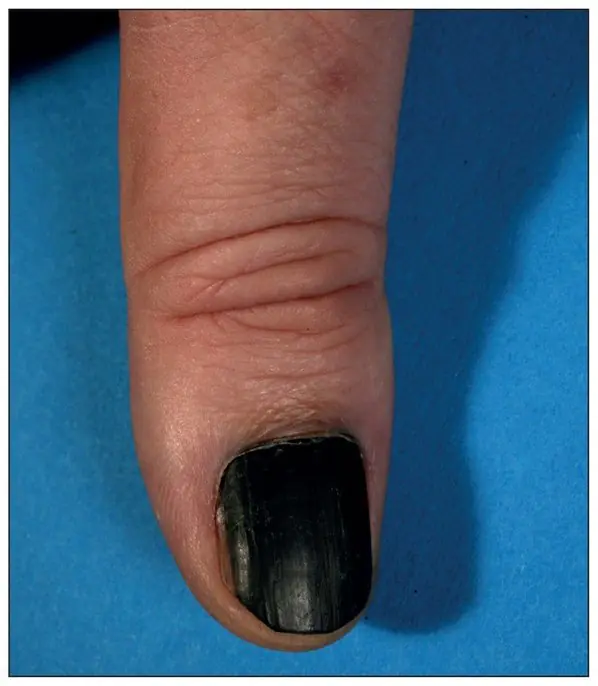
Subungual melanoma, Breslow thickness 1.5 mm [7]
How to distinguish subungual melanoma from everything else?
Here is a fairly simple algorithm.
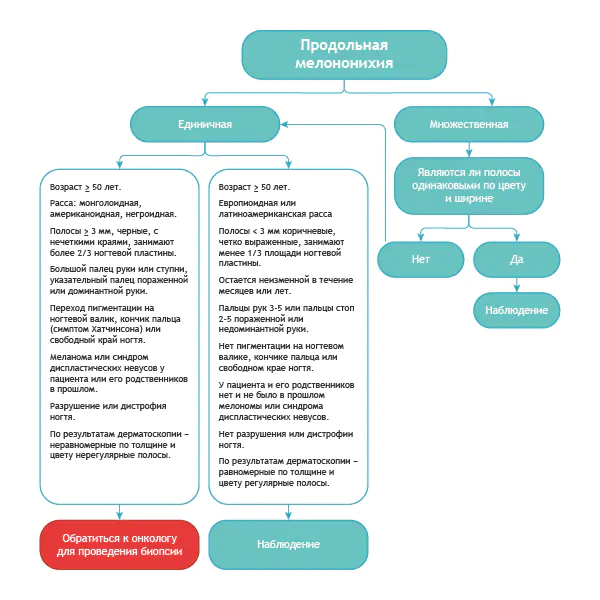
Algorithm for the differential diagnosis of benign melanonychia and the same condition in melanoma [8]
ABCDEF rule for diagnosing nail bed melanoma
A (age) age - the peak incidence of subungual melanoma occurs between 50 and 70 years of age, and also indicates races with an increased risk: Asians, Africans - they account for 1/3 of all melanoma cases.
B (brown to black) – color brown and black, with a stripe width of more than 3 mm and blurry boundaries.
With (change) – change in the color of the nail plate or no change after treatment.
D (digit) – the finger as the most common site of injury.
E (extension) – spread of pigmentation to the nail fold or fingertip (Hutchinson’s symptom).
F (Family) – relatives or the patient have a history of melanoma or dysplastic nevus syndrome. [eleven]
How to distinguish a hematoma from a subungual melanoma by dermatoscopy

Hematoma: [10]
- It moves under the nail along with its growth. You can track this by taking a photo of the formation against the background of a ruler located longitudinally. It is important to note that a hematoma does not always appear due to trauma.
- Color from red-blue to black-blue.
- Does not transfer to the cuticle, nail fold and fingertip.
- Does not involve the entire nail in the longitudinal direction.
- May change within a few weeks.
- The color intensity decreases from the center to the periphery.
- It may be preceded by trauma.
- Small blood spots oriented towards the edge of the nail on dermatoscopy
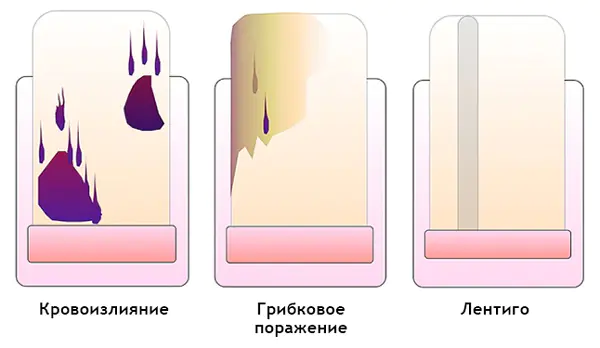
Subungual melanoma: [12]
- Heterogeneous color, irregular stripes with melanonychia.
- Triangular stripes.
- Spreads on the nail plate, free edge of the nail or fingertip.
- Destruction or dystrophy of the nail.
How is the diagnosis made?
If you suspect melanoma of the nail bed, there are 3 scenarios:
- Observation with photographic recording and repeated examinations.
- Biopsy with partial removal of the nail plate.
- Biopsy with complete removal of the nail plate.
The resulting material is sent for histological examination.
Treatment of subungual melanoma
As a rule, we are talking about amputation of a finger. Recently, many researchers are inclined to amputate the phalanx instead of the entire finger. There are also works that show that the amount of indentation does not affect the forecast.
Forecast
As with melanomas of other localizations, the prognosis directly depends on the results of histological examination. At the same time, it should be noted that the prognosis for subungual melanoma is somewhat worse than for those located on other parts of the body. The lower the Breslow thickness, the better the prognosis.
Summary
Subungual melanoma is a tumor that is quite difficult to diagnose early. The most common signs are the presence of a stripe on the nail and the transition of pigmentation to the nail fold or fingertip. If you find one of these symptoms, you need to see an oncologist.
P.S.: If you find yourself at an appointment with a dermatologist or oncologist, show him your nails. If you wear nail polish, it is best to remove it before your appointment.
Bibliography
- Miller AJ, Mihm MC. Melanoma. N Engl J Med. 2006; 355:51-65.
- Data from the Globocan 2012 study, International Agency for Research on Cancer (IARC):
- Kuchelmeister C, Schaumburg-Lever G, Garbe C. Acral cutaneous melanoma in caucasians: clinical features, histopathology and prognosis in 112 patients // J. Dermatol. – 2000
- Takematsu H, Obata M, Tomita Y. Subungual melanoma. A clinicopathologic study of 16 Japanese cases // Cancer. – 1985
- Wu XC, E >
Other articles:
Useful article? Repost on your social network!
Leave a comment or ask a question

Hello! Unfortunately, the information you provided is not enough. An online consultation does not boil down to “I looked at the photo and gave an accurate, reliable diagnosis.”
To make my answer as substantiated as possible, I ask you:
1) Answer the questions in the questionnaire located at this link:
https://cloud.mail.ru/public/N6PL/vjuWrRPvp
You can simply copy the questionnaire into the text entry field and enter the answers immediately after the questions.
2) Send a photo in accordance with the recommendations of this article:
http://beinusov.ru/info/kak-sdelat-khoroshee-foto-rodinki-5-sovetov/
A good photo is more important than a questionnaire, so if you can’t do it as described in the article, it’s better not to waste time and immediately see an oncologist for an in-person consultation.
3) Due to the very large number of questions, I answer only on Mondays.
Finger cancer is a pathological condition of the body, which is characterized by uncontrolled and chaotic division of mutated cells of finger tissues. A malignant neoplasm can originate from the skin, connective tissue and bone layer of the phalanges of the arm or leg.
Classification and description
- Skin cancer of the finger:
Clinically it occurs in the form of melanoma. The tumor is formed from cells of the superficial layer of the epidermis, called melanocytes, since they produce a specific pigment - melanin.

According to the clinical course of the disease, doctors distinguish three forms of finger melanoma:
- The superficial nodular form is considered the most common melanoma, which is formed from congenital nevi and age spots. The pathological neoplasm develops very slowly in the initial period, without causing subjective complaints in the patient. After 1-2 years, such a malignant tumor begins to actively grow, form metastases, causing a tumor of the toe or cancer of the hand. The appearance of the cancerous lesion is a flat brown growth with dotted blue spots. Melanoma, as a rule, shows a tendency to ulcerate, bleed, and does not rise above the surface of the skin.
- Nodular melanoma is considered a particularly aggressive tumor because it has infiltrative growth (penetrates into the deep layers of the skin) and early formation of metastases. The disease is characterized by the development of a nodular lesion of an unchanged area of dark-colored skin. The nodular form of the tumor, as a rule, grows very rapidly, therefore, as a result, the prognosis of the disease is extremely unfavorable.
- Lentigo melanoma predominantly affects older people. Finger cancer is localized in open areas of the skin and looks like a dark blue spot with radial growth of pathological tissue. The prognosis of the disease is considered favorable.
- Tumors of soft tissues of the finger:
Formed from the muscle and ligamentous tissue of the hand. Such cancers of the fingers are abundantly innervated and supplied with blood. Given the nature of the localization of soft tissue sarcoma, the malignant neoplasm rapidly increases in size and forms distant metastases. Clinical manifestations of the tumor include limited swelling and redness of the phalanx of the hand. The occurrence of pain is associated with the pressure of cancerous tissue on the nerve endings of the finger. The pain is not relieved by traditional painkillers for a long time. With timely diagnosis, the disease maintains a favorable outcome.
This is a malignant neoplasm of bone structures. Toe cancer and hands, proceeding according to the osteoid type, affects in most cases middle-aged people.

Symptoms of the disease occur in the later stages of cancer development. The most common complaint of patients is aching pain, which intensifies as the cancer tumor grows. Visual manifestations of oncology: formation of protrusion of the bone structure, dysfunction in the form of joint contracture, ulceration and bleeding.
Osteosarcoma gradually goes through two stages during development:
- Localized sarcoma. The pathological process is concentrated only in the area of primary bone damage.
- Metastatic tumor. At this stage of oncology development, cancer cells may be located in distant organs of the body. For example, finger bone cancer often metastasizes to the axillary lymph nodes and chest organs.
Diagnosis of finger cancer
Diagnosis of malignant tumors of the fingers is carried out by an oncologist. First of all, the patient undergoes a visual and palpation examination, during which the localization and extent of the oncological process is established. After the initial examination, the patient is prescribed additional diagnostic methods:
- An X-ray examination, during which the location and structure of a cancerous lesion of bone tissue is clarified.
- Computed tomography is a highly accurate method for determining the presence of a malignant neoplasm using layer-by-layer fluoroscopy.
- Bone scan. The method allows you to diagnose how toe cancer, so finger cancer, which sometimes cannot be diagnosed using x-ray methods.
The final determination of the type and stage of tumor development is possible based on the results of cytological analysis of mutated cells. Samples of cancerous tissue are removed during a biopsy.
Modern treatment of finger cancer
Modern patients are increasingly choosing the video consultation format to receive recommendations from the most famous doctors, regardless of geolocation. Find out how much it costs to communicate remotely with doctors who treat politicians and presidents!
Oncology of the skin and bone tissue of the extremities can be surgically excised using traditional surgery (late stages of the cancer process) and the method of deep freezing with liquid nitrogen (initial stage of the disease). Malignant processes in the deep layers of the finger and osteosarcoma require radical intervention to remove the tumor along with nearby healthy tissue. In cases of significant spread of oncology, surgeons perform amputation of the hand or upper limb.
Additional methods of therapy that are used to stabilize malignant growth in the preoperative period and to prevent the formation of metastases after tumor resection:
- Chemotherapy is a method of destroying cancer cells using cytotoxic drugs.
- Radiation therapy, which involves the use of highly active x-rays.



