
Causes and signs of peritonitis. Disease stages and classification. Methods of diagnosis and treatment of peritonitis.
The content of the article:- What is peritonitis
- Reasons for development
- Symptoms and stages
- Diagnostics
- Treatment options
- Surgical intervention
- Medicines
Peritonitis is an inflammation of the peritoneum, which is a life-threatening complication of pathologies or injuries to the abdominal organ. The inflammatory process is often acute, that is, it develops quickly - over several hours and days. Much less often, the pathology subsides and resumes again, that is, it proceeds in a chronic form.
What is peritonitis?

Since the abdominal cavity is divided into several anatomical sections, and there are quite a few causes of peritonitis, it is customary to distinguish several forms of inflammation of the peritoneal layers.
Depending on the prevalence, there is the following classification of peritonitis:
- Limited peritonitis. It occurs if the area of inflamed peritoneum is limited by some formation, and the inflammation does not tend to spread beyond the affected peritoneum. Essentially, it is an abscess or abscess, the boundaries of which are adhesions, fibrinous deposits, omentum (a fold of peritoneum that contains a lot of fatty tissue) or intestinal loops. Accordingly, appendicular (in the area of the appendix), subphrenic, subhepatic and pelvic abscesses may occur.
- Diffuse peritonitis. The inflammation spreads quickly and does not tend to be limited to any one part of the abdominal cavity. If peritonitis is located near the source of infection, then it is considered local, but if it occupies several anatomical areas of the abdominal cavity, then it is general.
The peritoneum itself has 2 layers: visceral (inner layer) and parietal (outer layer). Its inflammation is accompanied by the release of inflammatory fluid, the nature of which determines the form of peritonitis.
Depending on the type of effusion, infectious peritonitis is:
- Serous. The liquid is colorless and consists mainly of protective white blood cells.
- Fibrinous. Through small pores on the layers of the peritoneum, with severe inflammation, fibrin begins to be released - a substance that has adhesive properties. This form leads to the formation of adhesions in the abdominal cavity.
- Purulent. Pus can form in the peritoneum itself or get there due to a rupture of an already inflamed organ in which a purulent mass has accumulated. Pus consists of dead white blood cells and bacteria. Purulent peritonitis is life-threatening because reabsorption of pus through the open pores of the peritoneal layers is impossible.
- Putrefactive. The putrefactive component of effusion occurs if putrefactive bacteria enter the abdominal cavity, which gradually destroy the wall of the affected abdominal organ
There are also mixed forms, for example, fibrinous-purulent peritonitis.
Aseptic peritonitis can be:
- Gall - Occurs after a rupture of the gallbladder or bile ducts.
- Mochevym - develops if urine enters the peritoneum, which is observed when the urinary tract (ureters and bladder) ruptures. Renal rupture does not cause urinary peritonitis because the kidneys themselves are not covered by peritoneum (they are located in the retroperitoneum).
- Kalov - when any part of the intestine ruptures.
- Enzymatic - occurs when pancreatic juice spills into the abdominal cavity.
- Hemorrhagic - characterized by the presence of blood discharge in the abdominal cavity. Most often this is observed with a rupture of the organ wall or abdominal injury.
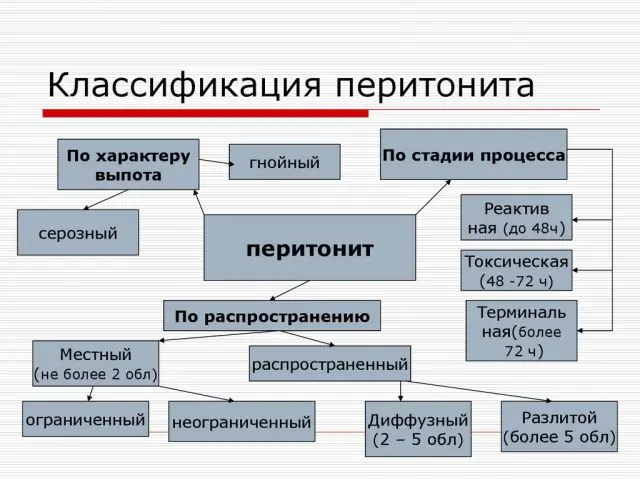
Scheme of types of peritonitis
Complications of peritonitis are associated with two scenarios - abdominal sepsis and septic shock. Abdominal or abdominal sepsis is an advanced disease when there is no specific (primary) source of pus in the abdominal cavity. This complication requires several operations.
Sepsis is blood poisoning and the formation of purulent foci in other organs. Manifestations of sepsis may include liver damage (hepatitis), brain damage (encephalopathy, cerebral edema), pneumonia, heart failure, and kidney failure.
Other complications of peritonitis include intestinal paresis (decrease in intestinal muscle tone), dehydration, and intestinal fistulas.
The prognosis of peritonitis depends on age, gender, and duration of the disease. It is worsened by the presence of colon disease, a malignant tumor. If peritonitis lasts longer than 24 hours, there is a very high risk of death.
Note! Often “peritonitis” is called “acute abdomen”. But the latter concept applies to any pathology of the abdominal organs, which requires surgical treatment. Thus, an “acute abdomen” is a potential peritonitis.Reasons for the development of peritonitis

Peritonitis most often develops under the influence of an infection that penetrates from any source into the abdominal cavity. The abdominal cavity itself and the peritoneum (the thin membrane that covers the abdominal organs and abdominal wall) are normally sterile, due to the ability of this membrane to absorb and digest bacteria and foreign bodies that land on its surface. Infected infection or toxic substances are quickly absorbed from the surface into the blood and lymphatic system.
The causative agents of peritonitis can be:
- Nonspecific bacteria. These are all natural bacteria that normally populate the gastrointestinal tract, for example, E. coli, staphylococcus, streptococcus, enterococcus.
- Specific microbes. All pathogens that are not characteristic inhabitants of the digestive system, which cause one disease with typical symptoms (the disease is usually called the same as the pathogen). Specific pathogens include Mycobacterium tuberculosis, gonococci, and pneumococci.
Infection occurs either primary or secondary. The primary entry of microbes is observed when an infection is introduced through the blood, lymph, or through the fallopian tubes. In this case, peritonitis will be called primary. But this occurs quite rarely - only 10-15% of cases. Secondary infection is observed much more often and is a consequence of inflammation of the abdominal organ.
The causes of secondary peritonitis can be:
- Perforation. This is a rupture of an organ and a violation of the integrity of its wall, as a result of which the contents of its cavity enter the abdominal cavity. Violation of the tightness of the organ can occur with appendicitis (inflammation of the appendix of the cecum), cholecystitis (inflammation of the gallbladder), pancreatitis (inflammation of the pancreas), stomach or duodenal ulcer, intestinal diverticulum (pouch-like expansion in a limited area), as well as cancer destruction.
- Injury. Can be open or closed. An open penetrating wound to the abdomen causes immediate contamination of the abdominal cavity and violates the integrity of the internal organs. A closed injury occurs when there is hemorrhage into an organ (a strong blow to the stomach), a foreign body enters the stomach or intestines and ruptures their walls from the inside.
- Postoperative complications. A complication after surgery on the abdominal organs is caused by peritonitis when the postoperative wound becomes infected, or the sutures placed on the intestines are insufficient.
The most common cause of peritonitis is appendicitis (almost 60% of cases). In second place in prevalence is acute cholecystitis (10%), in third place are diseases of the stomach and duodenum (7%).
Non-infectious factors can also cause an inflammatory reaction of the peritoneum. Such inflammation is called aseptic (“a” - absence, “septic” - associated with infection) or abacterial. The causes of aseptic peritonitis can be bile, blood, urine, pancreatic juice, that is, any liquid that can enter the peritoneum when internal organs are damaged.
Symptoms and stages of peritonitis
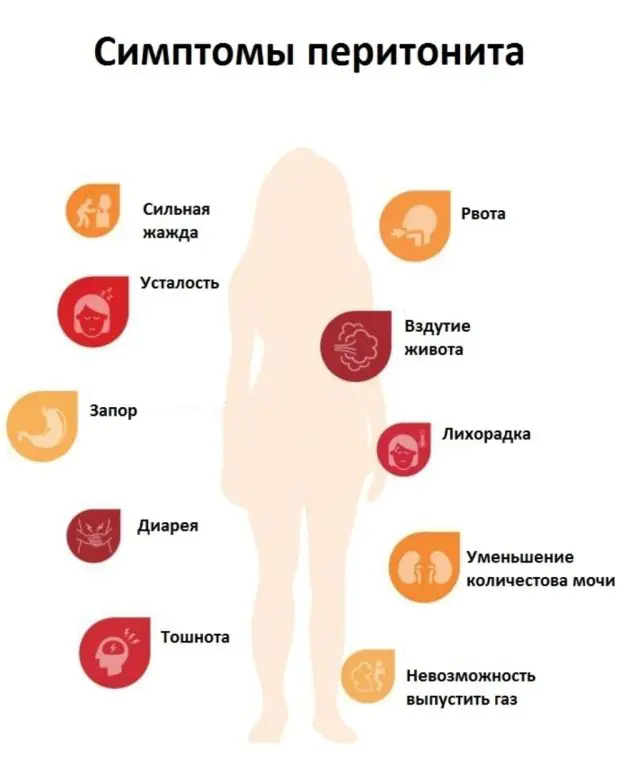
The onset of peritonitis is a disease of the abdominal organ. Symptoms depend on the stage of the inflammatory process in the peritoneum, as well as on the nature of the inflammatory fluid. If purulent peritonitis has developed, symptoms occur faster and are more pronounced.
Acute peritonitis causes the following symptoms, depending on the stage:
- Stage 1 (reactive). Any infection or fluid that spills onto the peritoneum after an organ rupture causes a typical inflammatory reaction - redness, swelling and the formation of an inflammatory effusion. In the first stage of peritonitis, severe abdominal pain occurs. It doesn't disappear, it lasts forever. The pain intensifies if the patient tries to move and change body position, and decreases if he lies still. Sometimes there is vomiting and diarrhea that does not bring relief. The first stage lasts 24 hours from the onset of inflammation of the peritoneum.
- Stage 2 (toxic). In addition to the local reaction, general symptoms appear, for example, fever occurs, the patient’s general condition deteriorates sharply, sticky sweat appears, dry skin and tongue, and the skin becomes pale. The patient's pulse quickens and blood pressure rises. Abdominal pain becomes more intense. A person tosses around in bed and cannot find a comfortable position. The reason for the general reaction of the body is the absorption of toxins and tissue breakdown products from the inflamed peritoneum into the bloodstream. The second stage develops 1-2 days after the onset of the disease.
- Stage 3 (terminal). This is the stage of complications and complete depletion of the body’s defenses. The appearance of signs of damage to the central nervous system is typical. The patient is apathetic, inactive, confusion appears, and sometimes there are attacks of excitement. The skin becomes bluish, facial features become pointed, and the eyeballs become sunken. Blood pressure drops sharply. Severe vomiting appears, and the vomit sometimes contains feces. The pain spreads throughout the abdomen.
Diagnosis of peritonitis

Peritonitis causes signs of irritation of the peritoneum, which can be determined by a doctor during examination. Other studies are aimed at identifying the cause of the disease and choosing a treatment method.
A general examination by a doctor can detect the following symptoms of peritoneal irritation:
- Shchetkin-Blumberg symptom. The doctor places his open palm on the area of maximum pain, slowly immerses his fingers, starting to press on the peritoneum. Then he abruptly takes his hand away. With peritonitis, a sharp increase in pain occurs at the moment when the doctor removes the hand.
- Plank belly. This refers to the protective tension of the muscles of the anterior abdominal wall. It occurs reflexively along with the appearance of pain in the area of inflammation of the peritoneum.
- Fetal position. The patient lies motionless, pressing his legs to his stomach (this reduces the tension of the peritoneum and pain).
- Kulenkampf's sign. The symptom is determined in women during vaginal examination. The doctor inserts fingers up to the cervix. With peritonitis, pain is detected in the area of the posterior vaginal fornix (inflammatory fluid accumulates there).
Signs of primary pathology are identified separately, for example, symptoms characteristic of appendicitis, cholecystitis, pancreatitis.
Diagnosis of peritonitis in a hospital requires the following tests and studies:
- General blood analysis. Reveals an inflammatory reaction in the form of a sharp increase in the level of leukocytes and ESR.
- Blood chemistry. Necessary for assessing the function of internal organs (primarily the liver, kidneys and pancreas). When they are damaged, changes in the level of liver and pancreatic enzymes, changes in the level of total protein, glucose, potassium, sodium, chlorine, acid-base balance of the blood and other indicators are detected.
- Bacteriological analysis. To find out whether there is infection of the whole body and blood (sepsis), a blood test is taken for sterility. If microbes are present in the blood, then after inoculating it on a nutrient medium, the growth of bacteria is determined (the pathogen itself and its sensitivity to antibiotics are identified). For bacterial analysis, inflammatory fluid taken from the abdominal cavity is also used.
- X-ray examination of the abdomen. When peritonitis has developed, a survey (without contrast agents) x-ray may reveal signs of intestinal obstruction, a raised diaphragm, the absence of a gas bubble in the stomach and other symptoms that indirectly indicate an inflammatory process in the peritoneum.
- Ultrasound. Ultrasound can help identify some causes of peritonitis, such as complications from gallstones, intestinal obstruction, bladder damage, and pelvic inflammatory disease (genital inflammation).
- Laparoscopy. This procedure is the main and most accurate for diagnosing peritonitis. The doctor inserts an endoscope through punctures on the anterior abdominal wall to examine the abdominal cavity. Using the same instrument, you can collect inflammatory fluid (it will be sent to the laboratory to identify the causative agent of the infection).
Additionally, the state of the immune system (immunogram), blood coagulation system (coagulogram) is determined, ECG and other studies are performed to prepare the patient for surgery.
Important! If a patient has nonspecific peritonitis, several microbes are detected in the abdominal cavity according to tests in the inflammatory fluid, but with specific peritonitis - only one microbe.Methods of treating peritonitis
You need to know that there is only one option for treating peritonitis - in the hospital and through surgery. In addition to surgery, the patient requires general therapy, but it is always carried out on the condition that the patient is scheduled for surgery. Situations when peritonitis is treated exclusively with medications do not relate to the disease itself, but to its prevention in non-purulent inflammation of the abdominal organ.
Surgical intervention in the treatment of peritonitis

The photo shows how surgery is performed for peritonitis
Surgical treatment of peritonitis consists of open surgery on the abdominal cavity. Laparoscopic surgery is performed through small punctures using instruments under video camera control; it is not performed in acute peritonitis. The fact is that with an open operation, inspection of all parts of the abdominal cavity and assessment of the integrity of the organ is much easier and more effective. In addition, the cause of the disease itself often requires open surgery.
For peritonitis during surgery the following is performed:
- removal of the source of infection (pus, bile, blood, dead or inflamed organ);
- restoring the integrity of the affected organ (suturing the wall in case of injury);
- administration of antiseptic solutions (iodine, hydrogen peroxide) to treat infected peritoneum;
- drainage of the abdominal cavity (after suturing the wound, a tube is left in it, through which newly accumulated purulent fluid can be removed).
The scope of the operation may be greater, depending on the cause of the disease. If peritonitis develops due to cancer, treatment recommendations vary. Often a minimal operation is performed to close the organ defect (perforation of the stomach or intestines), after which the patient is sent to remove the tumor itself, if possible.
After completion of the operation, repeated cleansing of the abdominal cavity (another operation) is required in the coming days if the peritonitis was widespread.
Important! If a diagnosis of “peritonitis” is established, the operation should be performed urgently, that is, within the next 2-3 hours after the patient’s hospitalization.Medicines for the treatment of peritonitis

General treatment of peritonitis includes the use of drugs that fight the infectious agent, remove toxins from the general bloodstream, and restore water and acid-base balance.
Important! It is strictly forbidden to take any painkiller until the diagnosis is confirmed. Relieving pain will make diagnosis more difficult because the main symptoms of peritoneal irritation will disappear or weaken.Antibiotics for peritonitis are prescribed before surgery, introduced into the abdominal cavity during surgery, and continued after removal of the pus for 10-14 days.
For peritonitis, the following antibacterial drugs are prescribed:
- Cefuroxime. It is a broad-spectrum antibiotic. The medicine is sold in ampoules-bottles. Price for 5 pieces - 75 rubles (41 hryvnia). Analogs of the drug - Claforan, Cefosin, Cephabol.
- Amoxiclav. An effective antibiotic against many bacteria. The price of powder for preparing a solution for intravenous administration is from 57 rubles (23 hryvnia). Tablets cost from 250 rubles (103 hryvnia). The maximum dose will cost 420 rubles for 14 tablets (200 hryvnia). Analogue - Medoclav, Flemoclav, Augmentin.
- Metronidazole. This is an antibacterial drug that destroys not only bacteria, but also infectious agents that belong to the class of protozoa. It is especially important for peritonitis against the background of a gynecological infection. A bottle of solution can be bought for 25-57 rubles (11-23 hryvnia). Analogue - Metronidazole-AKOS.
- Clindamycin. Prescribed if tests reveal putrefactive bacteria. An ampoule with the drug costs from 580 rubles (235 hryvnia), tablets - from 160 rubles (65 hryvnia). Analogues - Clindacin, Klimitsin.
- Vancomycin. A “reserve” antibiotic that is used if you are allergic to Amoxiclav. The price of the bottle is from 340 rubles (138 hryvnia). An analogue of the drug is Editsin.
- Ciprofloxacin. Antibacterial drug with a strong effect against bacteria. The injection solution costs from 35 rubles (22 hryvnia). Analogues - Ificipro, Procipro, Ciprodox.
- Fluconazole. This is an antifungal drug that can be bought for 20-170 rubles (from 17-20 hryvnia). Analogues are Caspofungin, Micafungin, Diflucan, which are similar in action.

In addition to antibiotics, in the hospital the patient is given intravenous solutions for detoxification, painkillers, anti-inflammatory drugs, and intestinal stimulants (as indicated). This treatment is called symptomatic, that is, aimed at eliminating individual symptoms. In case of massive blood loss, red blood cell transfusion is required.
How to treat peritonitis - watch the video:



