
Causes and signs of salpingitis. Diagnosis of the disease and methods of treating the disease in acute and chronic course.
The content of the article:- Causes of salpingitis
- Main symptoms
- Diagnostics
- Treatment methods
- Medicines
- Surgical intervention
- Folk remedies
- Physiotherapy
- Complications
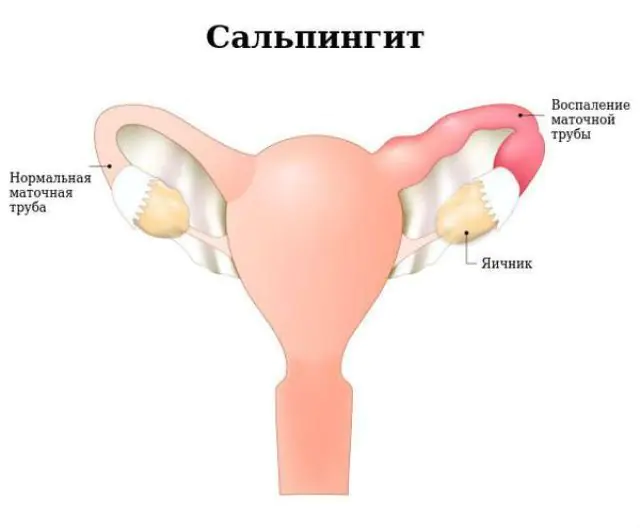
Salpingitis is an inflammatory lesion of the fallopian tube. Among all inflammatory diseases of the internal genital organs in women, this disease is the most common.
Reasons for the development of salpingitis
The disease is caused by an infection. Salpingitis has specific causes (pathogens of specific infectious diseases that have characteristic symptoms) and nonspecific (pathogens cause different symptoms, depending on the affected organ).
Specific causative agents of salpingitis include gonococcus (the causative agent of gonorrhea), chlamydia (the causative agent of genital chlamydia), mycoplasma (the causative agent of genital mycoplasmosis), and mycobacterium (the causative agent of tuberculosis). Less commonly, salpingitis is caused by a virus, such as genital herpes.
The most common causative agent of salpingitis is gonococcus, which enters the fallopian tubes sexually, often with sperm. The pathogen has the ability to attach to the surface of the mucous membrane of the fallopian tubes, that is, it gets the opportunity to penetrate into the deeper layers.
Chlamydia actually gets inside the cell of the tube mucosa and begins the slow process of its destruction. This chronic inflammatory process leads to scarring of the tube.
Nonspecific pathogens of salpingitis include Staphylococcus aureus, Escherichia coli, Proteus, and fungi of the genus Candida.
The infection spreads in the following ways:
- Rising. Infection penetrates from the uterine cavity and vagina through this route. The transfer of the pathogen occurs passively or actively. Bacteria that have penetrated the uterine cavity from the vagina, causing inflammation of the uterus, and then the fallopian tube, move passively. An active transfer mechanism occurs during sexual intercourse, with microbes using either sperm or Trichomonas (the simplest microorganism with flagella) as “transport”.
- Descending. This option is possible if there is inflammation of the abdominal organs that are adjacent to the fallopian tube. Most often, the infection spreads through a descending route from the inflamed appendix during appendicitis. In this case, the left fallopian tube is affected, since the appendix is located on the left. Less commonly, the infection spreads to the right fallopian tube from the sigmoid and rectum.
- Hematogenous. Sometimes the infection chooses to spread through the blood, but this occurs quite rarely.
Predisposing factors can facilitate the development of infectious salpingitis or cause its exacerbation:
- Medical manipulations. With any intrauterine intervention there is a risk of infection through the ascending route. Salpingitis can develop as a result of abortion, diagnostic curettage of the uterus, or during hysterosalpingography (introduction of a radiopaque substance into the uterus and fallopian tube to diagnose patency). Also at risk are women who need to have an intrauterine contraceptive placed, who have recently had childbirth or miscarriages.
- Chronic infection. Any chronic infection in the body can spread through the blood or hematogenous route, therefore, when the body is weakened against the background of a chronic disease of an infectious nature, salpingitis can develop.
- Hypothermia. As you know, hypothermia causes a sharp narrowing of blood vessels, some cells die, and the immune system begins to remove accumulated toxic substances. If there is even a mild infection in the genitals, the disease may worsen or spread.
- Sexual intercourse in the middle of the cycle. It is easier to get an infection from a sexual partner in the middle of the cycle, when the cervical mucus becomes less viscous and easily allows sperm and vaginal fluid to enter the uterus.
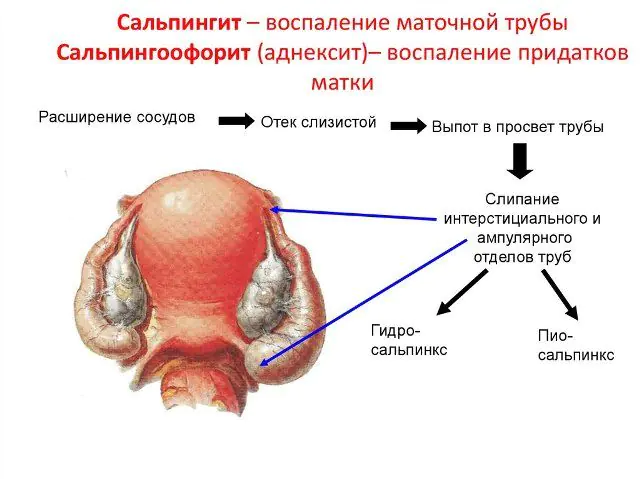
With salpingitis, all three layers of the tube are involved in the inflammatory process - the mucous membrane, the muscular layer and the outer layer of connective tissue. The inflammatory reaction is characterized by dilation of the vessels of the fallopian tube, swelling of its tissues (the tube increases in size) and the release of exudate or inflammatory fluid into its cavity.
A rare cause of salpingitis is torsion of the fallopian tube along with the ovary, when blood circulation is disrupted, the cells of the mucous layer of the tube, which are the worst at tolerating blood deficiency, quickly die, and the process of inflammatory “cleansing” of non-viable tissue begins.
For reference! Fallopian tubes are appendages of the uterus, similar in structure to tunnels. Each tube has a narrow part closer to the uterus and a wide part, open in the form of a flower bud, closer to the ovary. It is where fertilization of the egg occurs. Its function is to ensure transport of the embryo into the uterine cavity.Main symptoms of salpingitis
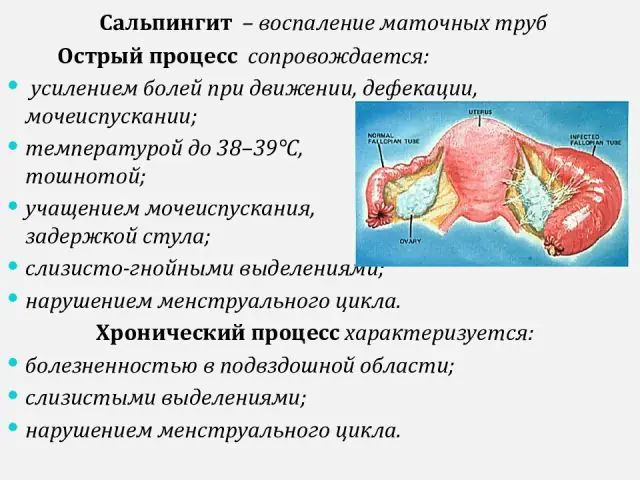
Signs of salpingitis differ depending on the course of the disease. There are acute and chronic, as well as subacute forms of the disease, each of which has its own characteristics.
Acute salpingitis has different severity. It all depends on the pathogen and the general condition of the body. The subacute form is a sluggish acute disease.
Chronic salpingitis is a silent acute illness that develops with improper treatment or weak immunity, as well as if the pathogen itself has low virulence (degree of aggressiveness). All symptoms of chronic salpingitis are unexpressed, and the disease occurs with periodic exacerbations.
Signs of acute salpingitis:
- Pain. A feeling of fullness, nagging and dull pain bothers the lower abdomen. The pain radiates to the hip, lower back, and rectum. This spread of pain is associated with irritation of the pelvic nerve plexuses. When the process spreads to the peritoneum of the pelvis, the pain becomes diffuse, that is, it is felt in the entire lower abdomen, and not just on the right or left. It usually intensifies when pressure is applied to the area of the inflamed appendage. Chronic salpingitis is characterized by increased pain after hypothermia, menstruation or stress.
- Discharge. With severe purulent inflammation, a mass with an unpleasant odor is released from the genital tract. For chronic and non-purulent inflammation, leucorrhoea or mucous discharge.
- General signs of infection. The patient's body temperature rises, chills appear, insomnia, irritability, general weakness and fatigue occur.
- Symptoms of damage to neighboring organs. A woman complains of frequent and painful urination, diarrhea and a painful urge to defecate (bowel movement). Typically, these symptoms indicate concomitant inflammation of nearby organs.
- Autonomic symptoms. They occur with pronounced psycho-emotional arousal, which often accompanies salpingitis. A woman complains of lack of sexual desire and orgasm, pain during intercourse.
Sometimes the only manifestation indicating chronic salpingitis is infertility. Occurs as a result of adhesions in the fallopian tube and pelvic organs. The result is obstruction of the fallopian tube.
Diagnosis of salpingitis

Diagnosis of salpingitis begins with an analysis of complaints and examination of the patient by a gynecologist. During the examination, the doctor palpates or feels the appendages. The appearance of pain when pressing is one of the signs of salpingitis, but not only the fallopian tube can hurt in this area. During a gynecological examination, pus or mucus is detected in the cervical area, which got there from the fallopian tube.
Research and analysis for salpingitis:
- Ultrasound of the pelvic organs. Both conventional and transvaginal ultrasound examinations are performed. In case of acute inflammation, a conventional ultrasound is used, since inserting a sensor into the vagina during an acute infection is prohibited.
- Laparoscopy. This is a surgical method of examining the pelvic cavity using an instrument with a camera. It is laparoscopy that is the main diagnostic study that makes it possible to diagnose chronic salpingitis, identify its consequences (adhesions), and also promptly treat purulent complications.
- Salpingography. X-ray contrast examination of the fallopian tubes reveals changes in the mucous membrane, adhesions, and cysts of the fallopian tube. A dye is injected into the uterine cavity and fallopian tubes, after which a series of x-rays are taken. But the technique is not used for acute purulent salpingitis.
- Smear examination. A smear taken from the cervical mucosa taken during a gynecological examination is sent to the laboratory, where it is used for several tests at once. Firstly, a PCR analysis is carried out, which reveals the DNA of the pathogen, and secondly, the collected material is inoculated on a nutrient medium. This is backanalysis. After a few days, bacterial growth appears on the nutrient medium. The pathogen is diagnosed based on the type of growth and treated with various antibiotics. This is how sensitivity to antibiotics is determined. But the causative agent of salpingitis can be detected in a cervical smear only in 10-25% of cases.
- Other tests. To diagnose the inflammatory reaction and assess the general condition, a general, biochemical and serological blood test for infectious agents is prescribed (especially if tuberculosis is suspected).
Treatment methods for salpingitis
Treatment of an acute form of the disease always begins with antibiotics, since the cause of the disease is infection. For purulent inflammation, surgical intervention is required. Additionally, restorative medications and physical therapy are prescribed. If acute and severe salpingitis has developed, treatment is carried out in the hospital, so the woman is hospitalized as soon as possible. Chronic salpingitis, if there is no need for surgery, can be treated in a clinic. In any case, sexual intercourse should be excluded for this period.
Medications for salpingitis

Metronidazole for the treatment of salpingitis
Considering that salpingitis can be caused by various microbes, and at the same time, several antibiotics are prescribed at once. The duration of treatment should be 7-14 days. For severe inflammation, antibiotics are administered intravenously or intramuscularly until the condition improves and for another 1-2 days after the symptoms disappear. The action of all drugs is aimed at destroying the bacterial cell.
In chronic salpingitis, antibiotics are prescribed only during periods of exacerbation of inflammation, as evidenced by blood tests.
Antibiotics prescribed for salpingitis:
- Amoxiclav. The price of 15 tablets in the minimum dose starts at 250 rubles (103 hryvnia). The maximum dose costs from 420 rubles for 14 tablets (200 hryvnia). Analogs: Augmentin, Flemoklav, Medoklav.
- Ceftriaxone. A bottle of the drug for injection costs 17 rubles (7 hryvnia). Analogs are Cefson, Cefaxon.
- Ciprofloxacin. The price of tablets is from 33 rubles (22 hryvnia) for 10 pieces. The injection solution costs 35 rubles (22 hryvnia). Analogs: Ificipro, Procipro, Ciprodox.
- Gentamicin. 10 ampoules can be purchased for 40-50 rubles (16-20 hryvnia). Analogs are Garamycin, Gentacyclol.
- Lincomycin. The price of 10 ampoules starts at 40 rubles (16 hryvnia), tablets and capsules cost 60-90 rubles (from 25 hryvnia). Analogues: Dalatsin, Clindamycin-Norton.
- Azithromycin. The price of tablets is from 60-90 rubles (35-40 hryvnia). Analogs are Azivok, Sumamed, Zitrolide.
- Doxycycline. The price for 10 tablets is from 20 rubles (8 hryvnia). Analogues - Doxycil, Dovitsil.
- Metronidazole. The price for tablets starts from 10 rubles (25 hryvnia), for candles - from 100 rubles (40 hryvnia). Analogues: Terzhinan, Trichopolum.
In case of salpingitis, it is mandatory to prescribe some antifungal drug to prevent the side effects of antibiotics (there is a risk of activating a fungal infection).
Among the antifungal agents used to treat salpingitis are:
- Nystatin, the price of which is 20-28 rubles or 8-12 hryvnia for tablets, 84 rubles (35 hryvnia) for candles.
- Fluconazole (Diflucan), which can be purchased for 20-170 rubles (from 17-20 hryvnia).
- Polygynax, which sells for 400 rubles for 6 candles (120 hryvnia) and 700 rubles for 12 capsules (190 hryvnia).
All three antifungal drugs are considered interchangeable.
If salpingitis is caused or supported by a virus, then Acyclovir (Gerpevir) is additionally prescribed, which destroys the herpes virus. Its price for 20 tablets is from 60 rubles (25 hryvnia).
Additionally, for salpingitis, rectal or vaginal suppositories with analgesic, anti-inflammatory, and immunostimulating effects are prescribed.
In addition, treatment for salpingitis includes the following drugs:
- Interferon - a drug with antiviral activity. Analogues - Viferon, Genferon. The price of candles is from 370 rubles (from 160 hryvnia).
- Indomethacin - a drug that relieves pain and inflammation. An analogue is Metacin. The price for 10 candles starts at 90 rubles (40 hryvnia).
In case of severe general condition and the development of complications, infusion therapy is carried out in a hospital setting, the essence of which is the administration of liquids and blood-purifying drugs intravenously. The introduced substances remove toxins, restore acid-base balance, restoring the balance of the internal environment.
Surgical intervention for salpingitis

Surgery is required only if complications develop. The doctor will perform either open surgery or solve the problem using laparoscopy.
Surgical treatment allows you to get rid of adhesions and restore the patency of the tube, remove pus and cysts.
If severe purulent salpingitis has developed, surgery is required urgently, as it threatens the development of peritonitis. Urgent surgical intervention is also necessary for tubal pregnancy. In both cases, the fallopian tube is completely removed.
Folk remedies against salpingitis

Traditional medicine helps restore immunity and reduce the severity of the inflammatory reaction in chronic salpingitis. These methods are not a substitute for antibiotics if there is an infection.
For inflammation of the fallopian tube, you can use the following folk recipes:
- Take 1 part chamomile, 3 parts nettle leaves, 5 parts knotweed herb. Mix everything together. Pour 2 tablespoons of the mixture into a liter of boiling water, leave for an hour in a thermos. Use for douching twice a day.
- Take 2 parts of valerian root and lemon balm leaves, 3 parts of mantle grass and nettle. Pour 2 teaspoons of the mixture into one glass of boiling water, leave for 30-40 minutes, strain. The decoction should be drunk 20 ml per day.
Physiotherapy for salpingitis

Physiotherapy is indicated if the disease lasts more than 2 years. Natural and physical methods are suitable for treating chronic salpingitis. Natural medicinal baths (radon, iodine-bromine, hydrogen sulfide) are suitable.
Physical methods involve therapeutic effects in the form of microwave therapy, pulsed ultrasound, zinc electrophoresis, magnetic field, laser radiation.
The therapeutic effect is due to improved blood circulation in the fallopian tube, stimulation of regeneration processes and inhibition of the growth of scar tissue and adhesions.
Complications of salpingitis

Ectopic pregnancy as a complication of salpingitis
According to research, every second case of salpingitis is complicated by inflammation of the ovary on the same side. This condition is called “salpingoophoritis” or “adnexitis”.
Complications of salpingitis include:
- Infertility. The outcome of inflammation largely determines the nature of the inflammatory fluid. If the exudate contains a lot of fibrin (glue protein), then after the liquid part of the pus is absorbed, the walls of the tube stick together. The fallopian tube is contracted from the outside by dense adhesions between the organs, and from the inside its lumen narrows, and it cannot pass the egg further. Therefore, the unfertilized egg is destroyed, and if the sperm do reach the tube, then more often the embryo implants into the uterine wall (ectopic pregnancy), unable to move further.
- Ectopic pregnancy. Any chronic inflammation disrupts the function of the cilia of the mucous membrane. Thanks to their movement, mucus and fluid move towards the uterus. The fertilized egg is not moved by the movement of these cilia. Together with adhesions, this creates a favorable situation for tubal pregnancy.
- Sactosalpinx. If a lot of fluid is formed, and the lumen of the tube is closed on both sides, then so-called sactosalpinxes are formed - sacs filled with mucous fluid inside the tube. Essentially, these are intratubal cysts.
- Pyosalpinx and abscess. If pus forms inside the tube, the condition is called pyosalpinx. It causes adhesions between the fallopian tube and neighboring organs (intestines, bladder, omentum). If the ovarian end of the tube remains open, then the pus spreads to the ovary and an abscess or abscess occurs.
- Pelvioperitonitis. With salpingitis, there is always a risk of inflammation of the pelvic peritoneum, pelvioperitonitis. If the infection is not treated in time, the inflammation goes higher and causes general peritonitis, that is, inflammation of the entire abdominal cavity (above the pelvis).
How to treat salpingitis - watch the video:



