
What is sepsis: first signs, causes and diagnosis of the disease. Methods of treatment and methods of preventing sepsis in adults.
The content of the article:- What is sepsis
- Reasons for development
- Main symptoms
- Diagnostics
- How to treat sepsis
- Prevention
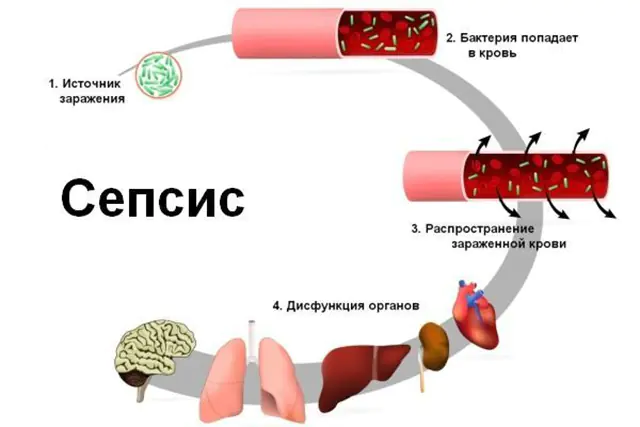
Sepsis (from the Greek “rotting,” “decomposition”) is a disease that affects the entire body, with pyogenic bacteria entering the bloodstream and then spreading throughout the body, causing the formation of ulcers in many organs. Therefore, sepsis is usually called blood poisoning in any purulent infection.
What is sepsis?

The photo shows the disease sepsis
Sepsis is a life-threatening condition. There are several stages, each of which has its own characteristics. According to them, 5 forms or types of illness are distinguished, which can transform into one another, that is, either from more severe to mild (this will mean recovery), or gradually become more complicated (there is a risk of death).
The following types of sepsis are distinguished:
- Purulent-resorptive fever- this is not sepsis yet, but a condition that risks developing into it. This form is characterized by a combination of a large local purulent focus and high temperature (above 38? C), which lasts for more than a week, but the pathogen cannot be detected in the blood.
- Septicotoxemia- this is already the beginning of sepsis. The symptoms of the first form are accompanied by signs of blood poisoning; microbes can be identified in it (culture on nutrient media is positive).
- Septicemia- this form is characterized by a very serious condition of the patient. There is a local purulent focus, a very high temperature and a positive blood test for microbes.
- Septicopyemia- the patient develops metastatic ulcers, that is, in addition to the known purulent focus, secondary foci of purulent infection appear in other organs.
- Chronic sepsis- a situation when purulent foci are already healing, the blood still contains infectious agents, episodes of fever periodically occur, and metastatic ulcers can form from time to time.
Sepsis can also be acute (lasts up to 6 weeks), chronic (lasts more than 6 months) and fulminant (develops in 1-2 days).
All complications of sepsis are reduced to septic shock. Shock is a condition when most of the body's vital functions stop working. Bacteria and their toxins tend to cause a sharp relaxation of the walls of blood vessels, which causes blood pressure to drop and fluid from the vessels passes into the tissues. Due to the lack of liquid blood throughout the body, the process of blood clotting can begin right inside the vessels. All organs receive less oxygen and blood, multiple organ failure develops - the simultaneous development of failure of the heart, kidneys, liver and lungs, internal bleeding.
Causes of sepsis development
The cause of sepsis is always a purulent infection. The causative agent can be almost any bacteria, but most often these are pyogenic microbes such as staphylococci, streptococci, Pseudomonas aeruginosa, Proteus, and Escherichia coli. All these microbes are ubiquitous. Many of them can be isolated from the body of even a healthy person.
In recent years, fungi of the genus Candida have also begun to cause sepsis. This is due to the improper use of antibiotics.
Viruses themselves cannot cause sepsis because there is no pus in a viral infection. However, the virus can sharply weaken the immune system, which the pathogenic bacteria present in the body will take advantage of and cause a purulent infection.
Sepsis cannot be contracted from another person, since it is a consequence of an infectious disease that a person already has, so the source is in the human body. An exception is sepsis, which occurs due to a violation of the sterility of the procedures performed by medical staff. It can also occur after operations.
The source of infection in sepsis can be:
- Lungs. Chronic diseases of the lungs and bronchi can easily cause the formation of pus (abscesses) inside the bronchus or in the lung tissue.
- Intestines. Bacteria are constantly present here, but they do not enter the blood. In some chronic diseases (ulcerative colitis and enteritis), pus is formed, and since the intestinal wall is rich in blood vessels, the pus can be absorbed into the blood.
- Leather. The source of the causative agent of sepsis can be phlegmon (purulent infection of adipose tissue), hidradenitis (inflammation of the sweat gland), pemphigus, purulent mastitis, as well as any skin infection in which blisters filled with pus form.
- Bones. Inflammation of bone tissue occurs with purulent osteomyelitis. The periosteum, which surrounds the bones, is rich in blood vessels, so in severe infections, pus easily penetrates into the blood.
- Ear, throat, nose. Purulent foci that form in the nasal cavity or paranasal sinuses (purulent sinusitis), in the middle ear (with otitis and mastoiditis), in the tonsils (with sore throat) often persist for a long time. Against the background of decreased immunity, all these diseases can cause sepsis.
- Teeth. Pus that accumulates in soft tissues when teeth are damaged immediately penetrates into the blood. With each brushing of the teeth, the mucous membrane is partially damaged, and microbes temporarily gain access to the bloodstream.
- Genitourinary system. Urogenital infections are often not completely cured; pathogens are present in these organs and are normal. Gynecological sepsis is especially common with purulent inflammation of the internal female genital organs (endometritis, salpingoophoritis).
Sepsis has causes that can also be divided into community-acquired and hospital-acquired. If an infection develops 48 hours after a person is admitted to hospital, the cause of sepsis is a bacteria that is common in the department (there are microorganisms that adapt to hospital conditions).
The development of sepsis proceeds as follows. In the presence of a purulent focus in the body against the background of a sharp decrease in immunity, when the pathogen is very dangerous and the protective forces are greatly suppressed, a purulent focus first forms. The inflammation becomes stronger and stronger, treatment does not help, and local immunity cannot cope. The pathogens penetrate the blood without encountering any obstacles. Here they are met by immune cells, which make up the general immune system. If these defenders fail, then the pathogens spread through the blood to all organs, settling in them and causing new foci of purulent inflammation.
Important! The severity of sepsis depends on the properties of the pathogen, the severity of the inflammatory process and the state of the immune system. Still, the decisive factor is an immunodeficiency state, in which even a mild infection can cause severe inflammation and blood poisoning.Main symptoms of sepsis
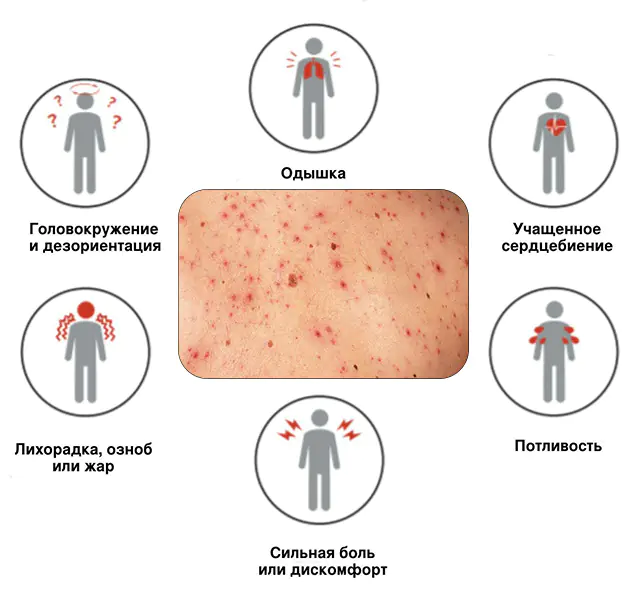
Sepsis always develops against the background of a pre-existing infectious disease. The fact that blood poisoning has occurred and the infection is spreading throughout the body can be judged by additional signs of sepsis:
- Local symptoms of inflammation. They correspond to the cause and place where the purulent focus formed. That is, how sepsis manifests itself locally depends entirely on the portal of entry and the source of infection. As it develops, all local symptoms become more pronounced. The disease invades more and more areas of the affected organ or breaks into neighboring organs and cavities. For example, a lung abscess can break into the pleural cavity (pain in the chest will appear when breathing), pus from the intestines can enter the abdominal cavity (sharp pain in the abdomen will appear, which intensifies with the slightest movement).
- General symptoms of inflammation. These signs are a consequence of the body’s general reaction to blood poisoning by pathogens and their toxins. A sick person develops a severe fever, his health sharply deteriorates, his performance decreases, weakness, pain in muscles and joints, chills, and cold sweat appear.
- Blood coagulation disorder. Many pathogens, such as staphylococcus, can enhance blood clotting. This causes the formation of small blood clots (thrombi) in the vessels. Blood clots block the lumen of the vessel, disrupting the blood supply to the organ, and then hemorrhages occur under the skin and into the organs.
- Acute respiratory failure. Breathing becomes rapid and shallow. Shortness of breath appears. This is due to a lack of oxygen due to infection.
- Liver dysfunction. Manifested by yellowness of the skin and sclera. The reason for these symptoms is that the liver is forced to neutralize all toxins and bacteria in the blood. In addition, many bacteria destroy red blood cells, releasing bilirubin, which enters the skin and turns it yellow.
- Damage to the central nervous system. Toxins enter the brain and cause confusion, headaches, irritability, or complete indifference.
- Indigestion. Worries include diarrhea, bloating, vomiting, severe nausea, and lack of appetite. Sometimes vomiting and diarrhea may be bloody.
A striking example of chronic sepsis is damage to the heart valves due to chronic sore throat or purulent inflammation of the oral cavity. Each exacerbation causes the penetration of bacteria into the blood, and they gradually destroy the inner lining of the heart, causing a special form of sepsis - septic endocarditis.
Septic endocarditis is characterized by:
- Slow progression of heart failure- manifested by shortness of breath, palpitations, cardiac arrhythmias, decreased blood pressure, weak pulse, and the appearance of heart murmurs.
- Temperature "candles"- rise and sharp drop in body temperature. If you draw a temperature graph, its shape will resemble candles. Temperature suppositories are a fairly characteristic manifestation of sepsis with a chronic course.
- Anemiais anemia, which is characterized by a decrease in the level of red blood cells and hemoglobin. It manifests itself as weakness, headaches, weight loss (the body lacks oxygen, which is carried by red blood cells). The patient experiences pallor of the skin, which is combined with an earthy tint (“coffee with milk” color).
- Hemorrhages under the skin. A pinpoint red rash may appear on the skin - these are burst small vessels. Most often, such red dots form on the arms, legs and abdomen, especially when the skin is squeezed or pulled.
Sepsis in children of the first year of life can develop due to infection of the umbilical wound. In this case, there is a sharp redness of the navel, from which purulent fluid is released. You may notice an expansion of the venous network on the abdomen, while the skin also swells, and the inguinal lymph nodes enlarge. The skin around the navel becomes greenish - a sign of purulent decomposition. Jaundice may develop quickly. This condition is called umbilical sepsis.
Diagnosis of sepsis
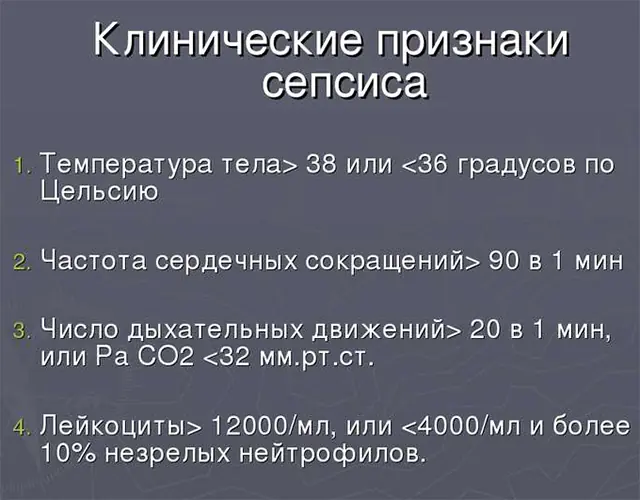
Diagnosis of sepsis requires a mandatory blood test for sterility. Without this analysis, we cannot talk about blood poisoning. Blood for research is taken from a vein, 3 times every hour. Three-time sampling is necessary for the simple reason that microbes may not be constantly present in it, that is, it is necessary to catch the moment of their penetration into the blood from the primary purulent focus.
The blood taken is used to treat the nutrient medium and the growth of microbial colonies is expected. After the bacteria appear, they are treated with different antibiotics to select the right drug for treatment.
Important! Blood cultures are taken before antibiotic treatment is started. Otherwise, the analysis may produce incorrect results. If the patient is taking antibiotics, the doctor must be notified. He will stop the medication for 3 days so he can get tested.In case of sepsis, the following tests must also be taken:
- General blood analysis. It reveals the body’s inflammatory response (increased leukocyte levels, accelerated ESR). In addition, with sepsis, either a decrease in the level of red blood cells (in severe sepsis) or an increase in their level (in chronic sepsis), as well as a low level of hemoglobin (a sign of anemia), is determined.
- Blood chemistry. Allows you to assess the condition of internal organs, especially the liver (based on the level of ALT, AST, bilirubin, total protein), kidneys (urea, creatinine), determine the acid-base balance of the blood, the level of potassium, sodium, calcium, chlorine, acute phase proteins, inflammation (especially CRP, seromucoid) and other indicators.
- Coagulogram. This is an analysis of the blood coagulation system, it reflects the ability of coagulation factors to stop bleeding in time. In sepsis, coagulation factors are depleted (they are produced in the liver), which causes hemorrhage.
- Immunogram. The analysis allows you to obtain data on the state of the body’s protective cells, their activity and quantity.
Additionally, radiography, ultrasound, computed tomography and other methods may be required to identify purulent foci in the body.
How to treat sepsis?
Treatment of sepsis is carried out only in a hospital setting, given that the patient’s condition is almost always very serious and requires intravenous administration of drugs. Since the disease is caused by an infection, it is clear how to treat sepsis - with antibiotics.
Antibiotic therapy is aimed at destroying the pathogen. But these drugs alone will not be enough. If sepsis develops, complex treatment is required. To eliminate the inflammatory process and general intoxication of the body, immunotherapy, symptomatic and surgical treatment, as well as physical therapy are prescribed.
To eliminate sepsis, drugs with antibacterial action are prescribed immediately after taking a blood test for sterility. Before receiving the result, the patient is prescribed broad-spectrum antibiotics, and after receiving information about the sensitivity of the pathogen to a specific drug, the medicine is either changed or several drugs are prescribed. Medicines are administered intravenously.

Among the antibiotics used for sepsis are:
- Cefotaxime. Analogs of the drug - Claforan, Cefosin, Cephabol. The medicine is sold in ampoules-bottles at a price of 75 rubles (41 hryvnia) for 5 pieces.
- Imipenem. Analogues of the drug from the same group of drugs are Aquapenem, Tienam. The price of the drug varies from 300 to 750 rubles (123-300 hryvnia).
- Rifampicin. Analogues are Rifampin, Rifacin. The price for a package of ampoules is about 600 rubles (250 hryvnia).
- Amphotericin. Analogs of the drug include Ampholip, Ambizom, Amfocil, Amphoglucamine. 1 bottle of solution costs about 30 rubles (12 hryvnia).
- Metronidazole. Analogues of the drug from the same group of antibacterial agents are Ornidazole, Meratin, Batsimex. A solution for intravenous administration costs from 32 rubles (15 hryvnia).
- Levofloxacin. Analogues include Basijen, Cipronate, Ofloxabol. The price ranges from 175-1000 rubles (from 40 hryvnia), depending on the analogue.
Drugs for the symptomatic treatment of sepsis are not aimed at correcting impaired body functions and removing toxins. Detoxification therapy is prescribed. Its purpose is to flush the blood of toxins. Solutions are administered intravenously to replace blood plasma, restoring the acid-base balance, blood coagulation system and other changes in metabolism and blood properties that arose as a result of sepsis. In case of severe anemia, intravenous transfusion of blood or red blood cells is indicated.
In the acute period of sepsis, physical therapy is performed to stimulate the body's response and destroy microbes, for example, ultraviolet or laser irradiation of the blood.
To cope with sepsis, it is necessary to eliminate the main risk factor - reduced immunity. Some drugs replace protective immunoglobulins, which are not enough to destroy the infection, while other drugs stimulate the immune system to produce new protective cells.

For immunocorrection the following are used:
- Taktivin. An analogue of the drug is Timalin, Vilozen. 5 ampoules cost about 790 rubles (330 hryvnia).
- Pentaglobin. Analogues include Gistaseroglobulin, Gamimun N, Intratect, Intraglobin, Octagam, Immunovenin. The price per ampoule is 2500-2800 rubles (1000-1200 hryvnia), bottles cost from 12,000 rubles (from 5000 hryvnia).
In order for the body to recover, the pus must be removed. It can only be removed through surgery. The surgeon makes an incision on the inflamed part, removes pus and dead tissue, and rinses the cavity, organ or wound with an antiseptic solution. At the first stage, the wound is not completely sutured. Drainage tubes are left in the former reservoir of pus to remove any remaining mucus or pus that may form while the infection is ongoing. When pus ceases to be released through the drainage tube, the cavity is completely sutured.
Prevention of sepsis

Prevention of the disease consists of timely treatment of any infection and maintaining immunity. To prevent sepsis, doctors' recommendations must be followed exactly.
Firstly, when you receive an injury, especially with an open wound, you need to wash it with antiseptics - these are solutions that destroy bacteria in the wound.
Secondly, if a doctor prescribes a course of antibiotics to treat a chronic purulent infection, then you cannot stop taking the drugs after the symptoms disappear. To prevent sepsis, all antibiotics must be taken for at least 7 days, otherwise the bacteria not only do not die, but also become resistant to this antibiotic - the next time it is prescribed, it may be ineffective.
You can’t just bring down a high fever and treat only the symptoms. High temperature is needed to destroy microbes; if you use only antipyretic and anti-inflammatory drugs without antibiotics, the bacteria will quickly cause sepsis.
Video about what sepsis is, its signs and symptoms:



