
Causes and symptoms of intestinal ischemia, diagnosis of the disease. Methods of treating the disease: conservative and aggressive therapy. Prevention of pathology.
The content of the article:- What is intestinal ischemia
- Causes
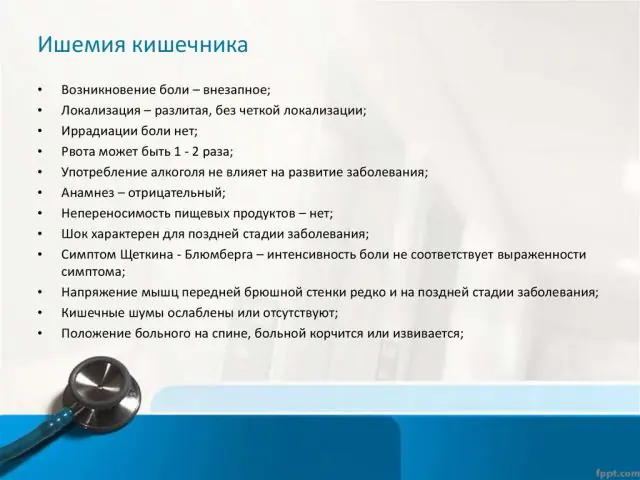
- Main symptoms
- Treatment methods
- Surgical intervention
Intestinal ischemia is a disease that develops as a result of deterioration of blood circulation in the lower gastrointestinal tract and manifests itself as abdominal pain. The pathology is dangerous because it disrupts the normal functioning of the intestines. The chronic form of the disease is fraught with weight loss and tissue necrosis, and 90% of acute conditions are fatal. The difficulty in treating intestinal ischemia was the lack of a systematic approach and the development of clear evidence-based treatment recommendations. The first unified document describing the method of care for such patients was published only in 2017 in the International Journal of Emergency Medicine.
What is intestinal ischemia?
Clinical picture of intestinal ischemia
Blood supply to the lower gastrointestinal tract (GIT) is provided by three arteries (celiac trunk, superior and inferior mesenteric). In one cardiac output, 15-35% of the blood flow occurs in this area. The level of blood supply depends on the stage of digestion.
In general, intestinal tissue is resistant to hypoxia; intestinal ischemia will begin to develop when blood supply decreases by more than 50% within 12 hours.
The etiology of disorders may be different. The disease is quite rare. Only 0.09-0.2% of all abdominal pathologies are due to this dysfunction. At the same time, not all specialists have the proper training to make the correct diagnosis. A complex symptom complex and the lack of standardized diagnostic algorithms against the background of late consultation with a doctor lead to a high number of deaths (from 55% to 80% of patients with a chronic condition and up to 90% with an acute form of the disease).
Note! More than 20 terms combine pathologies with symptoms of intestinal ischemia, among the frequently called ones are abdominal ischemic syndrome, mesenteric arterial insufficiency, and abdominal sore throat. Whatever the term is, it describes the lack of blood supply to the abdominal cavity.Causes of intestinal ischemia
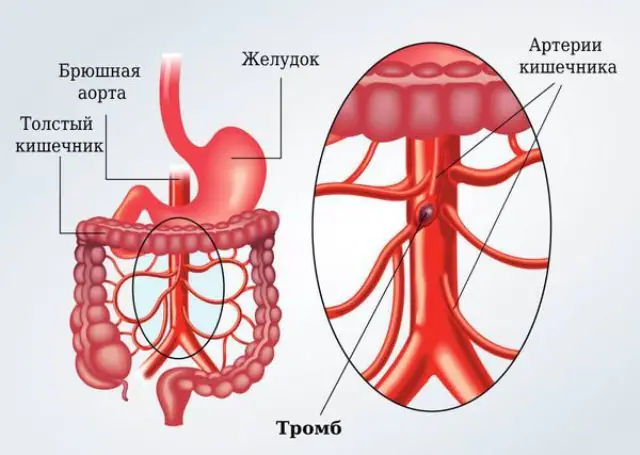
Based on the speed of development of symptoms of intestinal ischemia, acute and chronic forms of the disease are distinguished. The acute form is characterized by a sudden disruption of blood circulation and the development of a pathogenic clinical picture. Acute intestinal ischemia develops with thrombosis of the upper and lower mesenteric arteries and veins. The risk of such a pathology is significantly higher in patients with atherosclerosis, atrial fibrillation or cardiogenic shock. A sharp deterioration in blood circulation is also possible with embolism (blockage of blood vessels with uncharacteristic particles). Embolism, in turn, accompanies diseases of the cardiovascular system - heart defects, arrhythmias, but is also possible after transplantation surgery.
Less commonly, the cause of the development of acute forms of pathology is thrombosis of the mesenteric veins. Dysfunction can be provoked by inflammatory processes in the body or by taking certain pharmacological agents (cocaine, vasopressin, a number of oral contraceptives that increase blood clotting). In 50% of cases, it is not possible to identify the cause of the acute form of the disease. However, it has been established that concomitant pathologies are heart failure, arrhythmia, and hypotension. Presumably, the development of acute intestinal ischemia can also be caused by dehydration and accumulation of toxic substances.
Possible provoking factors for the development of the chronic form of the disease continue to be established. A clear relationship between the pathology and cardiac ischemia, atherosclerosis, and hypertension was revealed. In general, the causes of chronic poor circulation can be divided into two types - those caused by arterial dysfunction and extravascular compression. The extravasal type of deterioration in blood circulation is diagnosed in 10-38% of cases and is often associated with cancer in the abdominal cavity.
Note! The etiology of the disease is under study. Thus, it has been established that the risk of diagnosing chronic intestinal ischemia is higher in patients with Dunbar syndrome and Winivarter-Buerger disease, but the true mechanism of the relationship between pathologies is still being studied.Main symptoms of intestinal ischemia
The difficulty of diagnosing the disease is caused by the vague symptoms inherent in many diseases of the gastrointestinal tract. And if the pathology in the acute form, leading to infarction of the lower gastrointestinal tract, becomes more pronounced over time, then the chronic form is hidden under many “masks”.
In 96% of cases, patients complain of abdominal pain after eating. This condition is explained by increased stress during the period of active digestion. The pain is localized mainly in the navel area and varies in nature. In the early stages of the disease, the discomfort is comparable to the heaviness in the stomach or slightly lower. As the pathology develops, the pain becomes aching, gradually intensifying.
Another sign of chronic intestinal ischemia, which is often classified as a symptom of a common eating disorder, is intestinal dysfunction - increased flatulence, loose stools, but there may also be constipation. A clear symptom of disease progression is the patient’s weight loss. Weight loss is associated both with refusal to eat, caused by fear of pain, and with a deterioration in the absorptive functions of the intestines.
The symptom of atrophy of the gastric mucosa and ulcerative lesions deserves special attention. Various sources cite the figure from 18% to 46% of patients with stomach ulcers, who are subsequently found to have chronic intestinal ischemia. It is noteworthy that most often ulcerative lesions in this case occur on the antral mucosa. This is associated with the special sensitivity of the area to hypoxia.
According to the severity of the clinical picture, three functional classes of intestinal ischemia are distinguished:
- Clinical symptoms are not expressed, pain appears only during periods of active digestive stress, and is absent at rest.
- At rest, there are symptoms of poor circulation, which intensify during periods of stress. The patient loses weight, experiences constant pain, and the functions of the pancreas and intestines are impaired.
- The pain syndrome becomes chronic, and clear signs of the disorder appear—extreme weight loss, dystrophy of the gastrointestinal tract.
In 15% of patients, the third functional class of the disease is accompanied by tissue necrosis, which can lead to death.
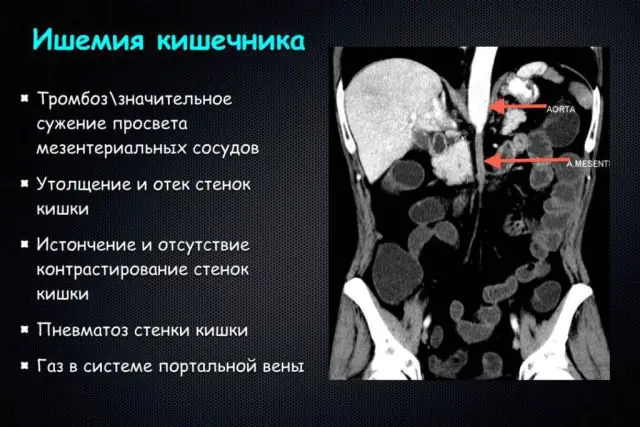
Early diagnosis of intestinal ischemia allows you to begin timely treatment and stop the progression of the pathology. At the initial stage, the doctor collects anamnesis, necessarily assessing whether the patient belongs to the risk group for the disease. X-ray of the abdominal cavity during this period is not very informative. The effectiveness of the method is no more than 45%.
The patient is prescribed an extensive range of examinations:
- analysis of blood cells for leukocytes - an abnormally high level is found in 90% of patients;
- lactate level analysis - an elevated level may indicate systemic gastrointestinal disorders and is a reason for performing a computed tomography scan;
- detailed blood test.
Esophagogastroduodenoscopy, colonoscopy, ultrasound of the abdominal aorta, angiography and Dopplerography can be used as additional instrumental examination methods.
Note! Specialized laboratory tests for diagnosing intestinal ischemia have not been developed at the moment, so patients need to undergo a whole range of multidirectional tests.Methods for treating intestinal ischemia

Essentiale N for the treatment of intestinal ischemia
The treatment regimen for the disease depends on the form of the pathology. Acute intestinal ischemia requires emergency treatment and early surgical intervention. But in the early stages of the chronic form of the disease, drug treatment and diet therapy are acceptable. Pharmacological treatment is aimed not only at treating the underlying disease, but also at eliminating symptoms.
The tactics of conservative treatment of intestinal ischemia are selected by the doctor individually depending on the functional class of the clinical picture. Certain recommendations regarding nutrition can be followed after surgery, as well as as part of disease prevention.
An important rule is the fractionation of meals: portions should be small, and the frequency of meals should be increased. The diet is lipid-lowering and includes 60% carbohydrates, 30% fats, 10% proteins. Preference should be given to vegetable fats and foods rich in fiber. Diet therapy should be prescribed taking into account the individual characteristics of the body and concomitant diseases of the person.
The diet is designed to normalize lipid levels. For the same purpose, lipid-lowering drugs Simvastatin, Fluvastatin, Atorvastatin can be prescribed; their action is aimed at reducing cholesterol levels. Simvastatin costs 39 hryvnia, 277 rubles per pack, but therapy can last more than six months.
In connection with prolonged drug treatment with statins, careful monitoring of liver enzymes will be required, as well as taking a course of hepatoprotectors - Essentiale N or its analogues Glutargin, Antral. Hepatoprotectors cost from 95 hryvnia, 160 rubles (Glutargin) to several thousand (Essentiale).
Drugs are selected individually to normalize the enzymatic activity of the gastrointestinal tract, as well as reduce the symptoms of the disease. Conservative therapy is considered effective if it is possible to reduce or completely eliminate symptoms and improve the hemodynamics of the gastrointestinal tract.
Note! Conservative therapy for intestinal ischemia has proven itself well in the treatment of patients with class 2 pathology. However, the decision on treatment tactics is made solely by the doctor.Surgical intervention for intestinal ischemia

Early surgical intervention is performed for acute forms of the disease. If the cause of insufficient blood circulation is embolism, then embolectomy or thrombectomy is performed. One of the intervention options is also a bypass connection of blood vessels and removal of necrotic areas of the gastrointestinal tract.
The prognosis for acute intestinal ischemia before surgery is 50%. In some cases, endovascular therapy (vascular) can be performed, aimed at improving blood circulation in the gastrointestinal tract by dilating blood vessels.
Patients with a chronic form of pathology of the third, as well as second class, with significant narrowing of blood vessels are sent to the department of vascular surgery. Depending on the degree of dysfunction and level of vascular narrowing, various types of bypass surgery, angioplasty or stenting are performed. Revascularization is also carried out in relation to patients undergoing surgery for other diagnoses in the area of the aorta or renal artery.
Due to the rarity of the disease, narrowly targeted measures to prevent intestinal ischemia have not yet been developed. The main recommendations of doctors are compliance with general health measures: normalization of nutrition and frequency of meals, moderate physical activity, avoidance of stress and overwork. It is recommended to stop drinking alcohol and smoking. People at risk need to monitor the functioning of the gastrointestinal tract and cardiovascular system, and if the first signs of illness are detected, consult a doctor. Preventive examinations are a key component of early diagnosis and minimizing the consequences of pathology.
How to treat intestinal ischemia - watch the video:
Intestinal ischemia is a difficult to diagnose disease that, if ignored, can be fatal. Difficulties are caused by the combined symptoms and passive attitude of many patients to dysfunctions of the gastrointestinal tract. At the same time, timely treatment gives a positive prognosis for intestinal ischemia.



