The cesarean section operation is used quite often today, since in many cases it can save the life of the child and mother. The scar on the uterus after a cesarean section can be different and sometimes even dangerous.
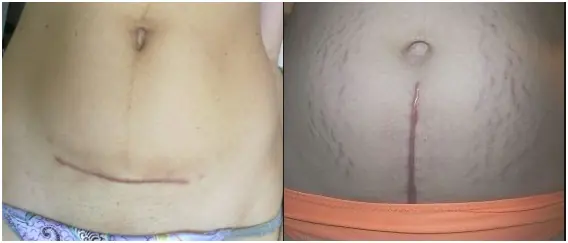
What does a scar look like?
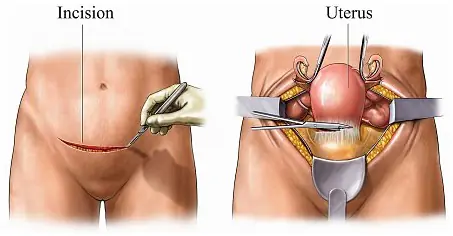
The cut can be made vertically or horizontally. Today, most often during the operation a horizontal incision is made. In this case, the seam is not noticeable in the future, since it is covered with linen. There may be an emergency situation when a vertical incision is made. This happens when the life of the child or mother is in danger and a caesarean section needs to be performed in a short time, since the child is removed easier and faster through a vertical incision.
The thickness and structure of the scar is very important. If the skin in this area is thinned, then there is a high probability of complications during healing. A normal scar is characterized by restoration of the uterine wall and muscle fibers. In this case, its thickness should be about 3 mm.
Note! The skin in the scar area is normally elastic and can withstand a fairly high level of pressure.
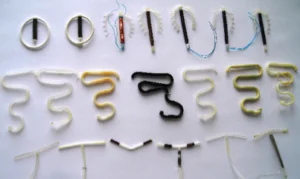
There are 2 main types of scar after cesarean section:
The first option is the norm. The thickness of the scar will not exceed 3-3.7 mm. At this point, the fabrics should be elastic and already withstand pressure. A wealthy scar is characterized by the content of not only connective tissue, but also muscle fibers. This allows it to stretch and contract at the same level as other body tissues.
A failed scar is registered at the stage when it is just beginning to heal. Therefore, it contains only connective tissue. In this case, the scar on the uterus after cesarean section will be thin - 1 mm. Its surface may be ribbed and without elasticity. If pressure is put on it, it will burst. More information about incompetent scars can be found in “Read more”.
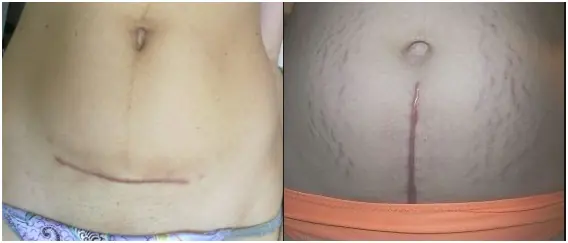
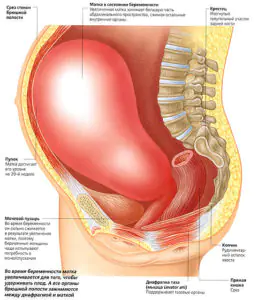
Scar thickness
How many mm should the thickness of the uterine scar be after a cesarean section? Its size is very important during repeated pregnancy. The norm for 32-33 weeks of pregnancy is a width of 3.5 mm. At week 38, the seam should be at least 2 mm. This indicator is the norm and if it is less, it may become untenable. And this is fraught with uterine rupture in late pregnancy. This condition manifests itself with symptoms similar to a miscarriage. When a thinned seam ruptures, dangerous consequences occur.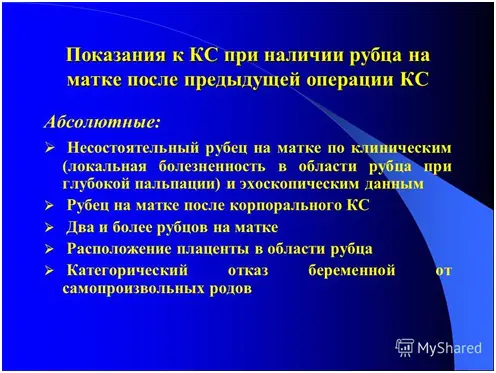
Complications
A cesarean section scar can even be dangerous for both the pregnant woman and the baby. Complications include:
- Lack of blood supply to the fetus - hypoxia;
- Incorrect location of the placenta, namely its attachment. These include anomalies in the form of malpresentation, accretion, ingrowth, too low or tight attachment.
- Disrupted blood clotting process, which leads to the formation of blood clots in a woman.
- Placental insufficiency.
- Rupture of the uterine wall.
In addition, it is noted that the scar subsequently leads to ectopic pregnancy.
With an incompetent scar, the following conditions may appear:
- Dysmenorrhea is painful menstruation.
- Metrorrhagia – discharge before and after menstruation, spotting and bleeding.
- Chronic pain in the pelvic area.
If the suture is not properly processed after surgery, this will lead to bleeding, suppuration and its divergence. These complications are mainly a consequence of infection. Additionally, there will be an inflammatory process around the suture, first the release of ichor, and then the appearance of pus, increased body temperature.
If a uterine rupture occurs, this is a condition that requires emergency medical care.
Treatment
If a woman has a second pregnancy and has a scar on the uterus, then an ultrasound should be performed early. If the fertilized egg is localized on the scar, the patient is advised to terminate the pregnancy, as there will be complications of the condition in the future. A woman can refuse an abortion, then control over the course of pregnancy is increased.
If the suture becomes inflamed after a cesarean section, it is necessary to treat it with various ointments. The doctor prescribes these drugs based on which symptoms still predominate. The most famous are:
- Contractubex is a gel that has a bactericidal effect. Additionally, itching on the wound surface is relieved. This drug is approved for lactation, as it is not absorbed into the blood. It is prescribed for use about 2-3 times a day and applied with light massage movements.
- Zeraderm Ultra is an ointment based on silicone. Thanks to this component, a thin film is formed on the scar, which does not allow moisture to escape from the tissue, thereby improving the structure of the scar and protecting it from microtrauma.
- Kelofibrase is a cream that helps soften tissue, increasing the elasticity of the skin at the scar site. Additionally, the drug has anti-inflammatory and antithrombolytic effects, and blood supply to the affected tissues also improves. Sometimes it is prescribed to make a compress with this cream for the whole night.
Clinical uterine ruptures of the completed type must be treated surgically. To do this, a transsection is performed, after which the rupture in the uterus is sutured or the organ is completely removed. But before this, the child is taken out, no matter how far along the pregnancy it is. This most often occurs before childbirth. If help was provided in the first 20 minutes, then the prognosis for the child is positive.
If an incompetent scar is diagnosed, then it is necessary to perform an open operation, less often laparoscopy is performed. In this case, destructive plastic surgery is performed, that is, the failed scar is excised and sutured in a new way.
Laparoscopy has a disadvantage in this case, since using this method it is impossible to influence in any way possible blood loss. Therefore, it often happens that laparoscopy ends with the opening of the abdominal cavity.
In the patient, the suture may thicken until an intrauterine septum forms. In this case, metroplasty is performed. That is, a surgical operation in which this septum is excised. This pathology is nothing more than an anomaly.
Metroplasty is also performed if the scar is uneven and includes ligatures, niches, etc.
Wobenzym is an anti-inflammatory drug that additionally has antiplatelet, fibrinolytic and immunomodulatory effects. This drug is often prescribed to women immediately after a cesarean section. This drug promotes rapid recovery and acceleration of healing and scarring processes after surgery. This is due to the improvement of blood microcirculation, the provision of antioxidant properties, and an increase in the supply of oxygen to the affected tissues. It is very important that Wobenzym prevents the development of endometritis. Because it occurs very often.
Forecast
If there is a scar on the uterus, this does not mean that the next time a woman should give birth only by cesarean section. If all the doctor’s recommendations are followed, then next time you can actually give birth naturally. The conditions for this are:
- transverse incision from a previous operation;
- the scar was initially wealthy;
- the placenta is placed normally, without any abnormalities;
- there is no history of gynecological diseases;
- correct position of the child;
- absence of critical situations-reasons for caesarean section.
If all this is observed, then natural childbirth can be carried out with a scar from a previous birth and the prognosis is favorable.
Doctors also give a favorable prognosis for the condition of the scar if the next pregnancy occurs 2 years after the first cesarean section.
Conclusion
A suture after a cesarean section requires special care and compliance with all doctor’s recommendations. This is due to the fact that if it fails, many complications of the condition and even rupture of the scar may occur. Especially women with repeated pregnancies need to carefully monitor their condition to avoid any negative consequences for the fetus. Indeed, in many cases this requires an abortion.


By clicking the "Submit" button, you accept the terms of the privacy policy and consent to the processing of personal data under the conditions and for the purposes specified in it.

Normal and pathological scar
If the incision on the uterus has healed well, then during an ultrasound the scar will be barely noticeable or even invisible. Normally, its thickness is at least 4-5 mm. During pregnancy, this indicator changes. At 32-33 weeks, the normal thickness of the scar is 3.5 mm, at 37-38 – 2 mm.
Incompetent scar on the uterus
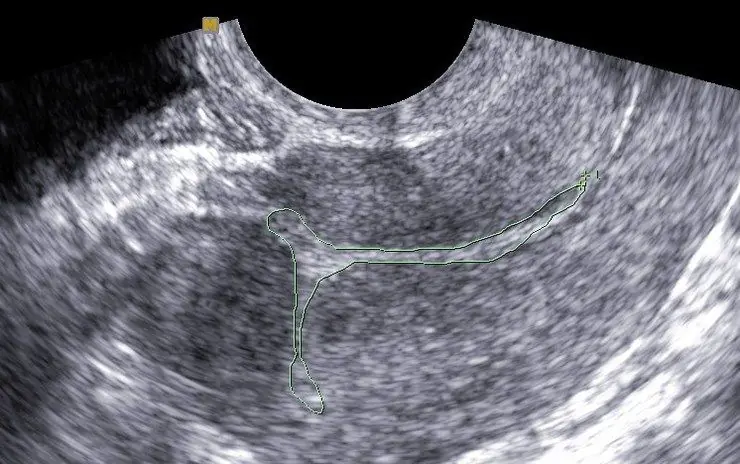
A defective scar on the uterus is thin. The thickness of the lower segment of the organ is less than 3 mm. Cicatricial changes are noted. If the damage is replaced by connective tissue, the muscular layer of the uterus cannot fully stretch with the growth of the fetus, and ruptures are likely. Moreover, changes can also occur in a scar of normal thickness. In this case, he will also be considered insolvent.
What causes a defective scar?
The complication arises due to the nature of the operation, as well as the nature and duration of the recovery period. The main reasons for the formation of an incompetent scar:
- Violation of rehabilitation terms. It takes 1-2 years for the uterus to fully recover. If you become pregnant during this period, have an intrauterine device installed, or undergo an abortion procedure by curettage, the tissues will not have time to fully grow together. Therefore, if you need any gynecological procedures, you should definitely inform your doctor about the surgery you have undergone.
- Late repeat pregnancy. Women who have undergone a CS are recommended to plan their next pregnancy no later than 4 years after surgery. Otherwise, connective tissue grows in the scar area, which makes it less elastic.
- Presence of complications after cesarean section. If inflammation occurs after the operation or due to insufficient contractility of the uterus, parts of the placenta remain in it, which requires curettage, the formation of a full-fledged scar becomes more difficult.
- Inappropriate sutures. The incision on the uterus after a CS should be sutured with special self-absorbing synthetic threads. When sutured with continuous sutures, the risk of complications reaches 95.4%.
Complications of a defective scar
The formation of a defective scar can cause complications during a second pregnancy. Every third woman experiences a miscarriage at different stages. Placental insufficiency is often diagnosed, in which nutrients and oxygen reach the fetus in insufficient quantities. In this case, the child may die.

Placental insufficiency due to uterine scar
During childbirth, there is a high risk of uterine rupture. If this happens, the baby may die due to lack of oxygen, and the mother may die due to extensive internal bleeding. Even if this does not happen, in most cases the uterus must be removed. Only an emergency CS with timely diagnosis of the pathology can save the situation.
Clinical guidelines
To avoid the formation of a defective scar or to diagnose it in the early stages, women after cesarean need to undergo regular ultrasound, especially when planning another pregnancy.
If after a CS there are signs of endometritis (pain in the lower abdomen, heavy uterine bleeding, purulent vaginal discharge), you must immediately consult your doctor for diagnosis and selection of an adequate treatment method.
It is recommended to adhere to contraceptive measures for at least a year after the CS to allow damaged tissue to recover. The appropriate method of contraception should be selected together with your doctor. The use of intrauterine devices is prohibited.
Treatment options
A scar, full or not, has no significant symptoms and does not cause concern if the woman is not pregnant. Therefore, no special treatment is required. The exception is defective scars complicated by inflammation. If they are present, suitable drug therapy or surgical intervention is selected.
When planning a pregnancy, an uncomplicated scar can be removed by metroplasty. This is an operation to restore the integrity of the muscle layer of the reproductive organ. During the intervention, scar tissue is excised to form a full-fledged scar. The procedure is carried out in three ways:
- transvaginally: through the vagina;
- laparotomy: with dissection of the peritoneum;
- laparoscopically: with the introduction of a camera and a manipulator into the pelvic area through small punctures in the abdominal cavity.
Managing pregnancy with a scar
In the first trimester, women who have undergone a CS should undergo a comprehensive examination. An ultrasound determines where the fertilized egg has attached. If this happens in the area of the scar, then such a pregnancy will be difficult to maintain. The scar tissue will become thinner, and there will be a risk of uterine rupture. In this case, to avoid life-threatening complications, abortion is performed by vacuum aspiration. Of course, only with the consent of the expectant mother.

Early diagnosis of uterine scar will help maintain pregnancy
Doctors also monitor the formation of the placenta. The scar can cause its pathologies (previa or ingrowth into the muscular layer of the uterus). In this case, the pregnant woman may need to be hospitalized until delivery.
If the scar is complete and the woman’s condition is satisfactory, the next examination takes place at 20-22 weeks. At this time, it becomes possible to detect fetal abnormalities and placental insufficiency. If it is confirmed, the pregnant woman is hospitalized and monitored in a hospital setting.
If during pregnancy there is pain when touching the abdomen, the abdominal wall becomes tense, the uterus contracts, or bleeding from the vagina occurs, you should immediately seek medical help. These are probably symptoms of a uterine wall rupture.
If the condition of the expectant mother is normal, the next screening is carried out at 37-38 weeks. During this period, the method of delivery is determined and the necessary medications are selected.
Childbirth after CS
Previously, a previous caesarean section was an absolute contraindication to natural childbirth. Now doctors are increasingly inclined towards independent delivery. Modern medicine has the necessary means to manage spontaneous childbirth in the presence of a scar on the reproductive organ. The natural method is preferable as it reduces the risk of bleeding and infection and shortens the recovery period after childbirth. Complications occur 3-4 times less frequently than with repeat CS.
But in some cases, a cesarean section cannot be avoided. It is necessary for scar failure, multiple scars and a longitudinal incision. The operation is also performed if there is a high risk of rupture, for example, if the placenta is attached in the area of the scar.
Natural childbirth is possible if there is one strong scar and no complications during pregnancy. The first child must be healthy, and the incision from the previous operation must be transverse. A woman is allowed to give birth herself if there are no fetal abnormalities and its weight does not exceed 3800 g.
The maternity hospital must have:
- Department of Anesthesiology and Reanimatology;
- neonatal intensive care unit;
- modern blood-saving equipment;
- 24-hour availability of emergency CS;
- obstetricians with experience in obstetric care for women with a uterine scar.

The labor room must have equipment for managing complicated births.
The presence of a scar on the uterus after a CS is a serious, but not hopeless case. Even with it you can carry and give birth to a child. The main thing is to regularly undergo medical examinations and follow all recommendations of your doctor.
I decided to tell you, my dear readers, a few stories from my life, or rather, from my medical practice.
A couple of months ago, a patient came to see me, who had specially flown in from Petropavlovsk-Kamchatsky to personally meet and consult. She had two caesarean sections. Now the thickness of the myometrium in the scar area is 5 mm, and there is a niche in the uterine cavity. She really wants to have a third baby. She made me laugh to tears, telling me how she brought to her antenatal clinic the answer to her question from the website of our clinic, where I write that 5 mm is the norm, the pregnancy is carried successfully. At the hospital, the patient was told that she was crazy, that the cleaning lady there answered her, and she believed it. So the patient came to meet me. She actually has a beautiful scar, 5mm thick. To be sure, I showed her ultrasound photographs of exactly the same scar in another patient of mine, who not only carried the pregnancy to term, but also gave birth safely through the vaginal birth canal.
Even with an initial scar thickness of 1 - 2 mm, pregnancy is carried out safely. This is not just my personal opinion. The same tactics are followed by all doctors in those large medical centers where I worked for many years (Family Planning and Reproduction Center and Perinatal Medical Center in Moscow).
After the story about the “cleaning lady,” I realized that my optimistic answers to questions about scars, that everything is fine, you can safely carry the pregnancy and not terminate it, are not always taken seriously, so I’ll back them up with two stories of pregnancy and childbirth.
I have been working as an obstetrician-gynecologist for 20 years and have extensive personal experience in performing cesarean sections and managing vaginal births in patients with a uterine scar, and I have the highest medical qualification category.
You see, the easiest way is to prohibit the patient from becoming pregnant or, even worse, to force her to terminate the pregnancy because of an allegedly thin scar - no one will even know whether this child could have been born. We should not forget about the possibility of severe complications after such an intervention. But, fortunately, there is a completely different level of medical experience and medical responsibility when such pregnancies continue. The outcomes are always favorable.
Some time ago, a patient called the clinic and asked me to answer the phone. I thank God that she called when I was at work. The patient's name is Olga. She told me that she was in the Perinatal Center of her region, she was examined by the chief doctor of the regional Perinatal Center, the chief obstetrician-gynecologist of the region, the leading ultrasound specialist, and she was being taken to the operating room right now. She has a scar on her uterus after two cesarean sections, now 25 - 26 weeks. And they decided to operate because the ultrasound showed that the scar had thinned down to 1 mm over a length of 9 mm. Now we need direct speech:
- How much, how much? – I ask again – 9 cm?
- Does anything hurt you?
— How much does the child weigh?
— Write a refusal from the operation. With such a scar in Moscow, you would generally be at home. Do you understand that the child will be born alive, but in the future will be severely disabled due to extreme prematurity, or will not be able to withstand nursing and will die? Discharge home and come to us, we will look at the scar ourselves. It is necessary to operate only when persistent, increasing pain occurs.
“Everyone is twirling their finger at my temple, saying that I’m not transportable, that if I get to 28 weeks, I’m happy, otherwise I can go to the toilet and die there, and the children will remain orphans.
- Do not worry! This definitely won't happen. You carry your pregnancy to 39–40 weeks.
Olga wrote a refusal. I gave her my mobile phone number. We constantly kept in touch before the birth. For the first 2 weeks she was still very intimidated, then they stopped frightening her. There, at 32 weeks, no thinning was found. And they sent me home. And at 39 weeks they had a planned caesarean section, and Olga gave birth to a wonderful, healthy boy weighing 3200 g. Such Happiness! The doctor who operated said that with such a scar, you are welcome again. Here's a thin scar for you!
When making a decision on early delivery due to a thin scar, one should take an extremely balanced approach, based on real complaints and clinical manifestations, and not on theoretically possible problems.
Here is another story of pregnancy and childbirth. This has already happened in Moscow.
Patient Lena came to see me after an examination at a well-known research institute, where the ultrasound report indicated that the body of the uterus was deformed by a niche on the side of the outer contour in the area of the scar after a cesarean section, the thickness of the myometrium in some areas was 1 mm, partially the myometrium was not determined. The institute issued the following conclusion. Diagnosis: Pregnancy 10 weeks. Failure of the uterine scar after a cesarean section in 2010. Recommendations: Taking into account the ultrasound data about the failure of the scar on the uterus after a cesarean section in 2010, I consulted with Professor N, the patient was recommended to undergo surgical treatment in an institute (plasty of an incompetent scar), after termination of pregnancy at the place of residence. The patient was reported to the district obstetrician-gynecologist.
We looked at the scar on an ultrasound. It is thin (according to our data 2 mm), low-lying. However, in my experience, all patients with such scars successfully carried their pregnancies to term. This was the case in this case as well. The patient never even had a threat of miscarriage, which could have been a reason for hospitalization. At first, the frightened Lena was still afraid of rupture, I convinced her of the reliability of the uterus as best I could. Only as the pregnancy progressed did Lena calm down. By the end of the pregnancy, she and I were already joking that we would give birth through the birth canal with such a scar. Of course, we didn’t give birth ourselves, because... the scar is still thin. But the operation was performed as planned at the 40th week; on June 6, 2014, a wonderful healthy girl weighing 3100 g was born. And here it is, another, boundless Happiness!
I could continue to describe such stories, since they are not isolated at all.