The result of an operation not related to the treatment of a purulent wound is the closure of the surgical field by suturing. If the tissues are infected, the surgeon creates the opportunity to remove the pus and reduce the amount of infiltration. Suture material used in surgery can be natural or synthetic. Ligature sutures may dissolve spontaneously some time after surgery, or they will require the help of a doctor to remove them.
If a dark cherry-colored serous fluid or purulent discharge is released at the site of the suture, this is a sign of a developed inflammatory process and the formation of a ligature fistula. The appearance of these symptoms is a sign of ligature rejection and a reason to resume treatment. A fistula that appears after surgery cannot be considered as a normal phenomenon; urgent treatment under the guidance of a surgeon is required.
Causes of ligature fistula:
Infection in the wound due to ignoring antiseptic requirements;
Allergic reaction to suture material.
There are factors that increase the likelihood of a postoperative fistula:
Immune reactivity (usually higher in young people);
Accession of a chronic infection;
Hospital infection, typical for surgical and therapeutic hospitals;
Getting into the wound staphylococcus and streptococcus, which is normally always found on human skin;
Localization and type of surgical intervention (cesarean section, surgery for paraproctitis, etc.);
Protein depletion in cancer;
Deficiency of vitamins and minerals;
Metabolic disorders (diabetes mellitus, obesity, metabolic disorders).
Features of ligature fistulas:
Occur in any part of the body;
Occur in all types of tissue of the human body (epidermis, muscle tissue, fascia);
Occur any time (week, month, year) after surgery;
They have a different development of the clinical picture (sutures can be rejected by the body with further healing of the wound, or they can become intensely inflamed with suppuration of the wound and not heal);
They occur regardless of the material of the ligature threads.
Symptoms of ligature fistula
The development of a postoperative fistula occurs according to the following scenario:
Within a few days after the operation, the wound area thickens, swells slightly, and becomes painful. The skin around it turns red and becomes hotter to the touch than other areas.
After 6-7 days, when pressure is applied, serous fluid and pus emerge from under the suture.
The general body temperature rises to subfebrile values (37.5-38°).
The fistula can close spontaneously and later open again.
Recovery is possible only after repeated surgery.
Complications arising from the appearance of a postoperative fistula
An abscess is a cavity filled with pus;
Cellulitis – inclusion of subcutaneous fat in the inflammatory process;
Eventration – loss of internal organs due to purulent melting of tissues;
Sepsis - the spread of purulent contents in the cavity of the chest, skull, and abdominal cavity;
Toxic-resorptive fever is pronounced hyperthermia as a reaction of the body.
Diagnostics
The primary diagnosis of a ligature fistula is carried out in the dressing room during a visual examination of the wound by a surgeon. To clarify the location of the fistula, the presence or absence of complications (abscess, purulent leaks), an ultrasound scan of the surgical wound is performed.
If the fistula is located deep in the tissue and its diagnosis is difficult, fistulography is used. During the examination, a contrast agent is injected into the fistula tract and radiography is performed. As a result of such manipulation, the fistula tract will be clearly visible on the x-ray.
Treatment of ligature fistula
The vast majority of cases of ligature fistula can only be resolved through surgery. The longer a postoperative fistula exists, the more difficult it is to cure. Complex therapy using medications is used for treatment.
Groups of drugs used to treat fistula:
Local antiseptics - water-soluble ointments (Levosin, Levomekol, Trimistan), fine powders (Gentaxan, Tyrozur, Baneocin);
Antibacterial agents – Ampicillin, Norfloxacin, Ceftriaxone, Levofloxacin;
Enzymes for the destruction of dead tissue - Trypsin, Chymotrypsin.
Since the drugs retain their effect for several hours, they are injected into the fistula tract and distributed throughout the tissues surrounding the wound several times a day.
Fat-based ointments (Synthomycin ointment, Vishnevsky ointment) prevent the outflow of pus, so they are not used in the presence of extensive purulent discharge.
In addition to surgical and drug treatment, physiotherapy is used:
quartzization of the wound surface;
As a result of the use of UHF therapy, microcirculation of blood and lymph improves, which leads to a decrease in swelling and stops the spread of infection. Quartz treatment has a detrimental effect on pathogenic bacteria, promoting stable remission of the process, although not guaranteeing complete recovery.
The “gold standard” for treating a ligature fistula is an operation that eliminates the problem completely.
Progress of the operation to eliminate the ligature fistula:
Three-time treatment of the surgical field with an antiseptic in the form of an alcohol solution of iodine.
Injection of an anesthetic solution into the tissue around the surgical wound and under it (Lidocaine - 2% solution, Novocaine - 5% solution).
Injection of dye into the fistula tract in order to completely examine it (“green paint” and hydrogen peroxide).
Dissection of the fistula, removal of the ligature completely.
Removal of the cause of the fistula along with revision of the surrounding tissues.
Stop possible bleeding with an electrocoagulator or hydrogen peroxide 3%, since suturing a blood vessel can provoke the appearance of a new fistula.
Wash the wound with antiseptics (Dekasan, 70% alcohol, Chlorhexidine).
Closing the wound with sutures again with the installation of active drainage.
After the operation, the patient needs dressings and drainage rinsing. If the purulent discharge is not fixed, the drainage is removed.
Medicines used in the presence of complications (phlegmonous inflammation of the tissue, purulent leaks):
Non-steroidal anti-inflammatory drugs (NSAIDs) – nimesil, diclofenac, dikloberl;
Ointments for tissue regeneration - troxevasin and methyluracil ointment;
Herbal preparations with vitamin E (aloe, sea buckthorn oil).
Local revision of inflamed tissues with wide dissection of the fistula is a classic form of surgical treatment of postoperative fistula. Most minimally invasive techniques are ineffective in treating this complication.
Self-medication of a ligature scar will not bring recovery, because only surgery and subsequent debridement of the wound can save the patient from complications. When attempting self-treatment, precious time will be lost.
Prognosis and prevention
In cases where the body rejects surgical sutures made of any material, the prognosis for the operation is unfavorable. The situation is the same with self-medication - in this case it is very difficult to make a forecast.
It is impossible to take preventive measures for the appearance of a fistula, since even with strict adherence to antiseptics, infection can penetrate into the surgical wound and rejection of the suture material.
Author of the article: Volkov Dmitry Sergeevich | Ph.D. surgeon, phlebologist
Education: Moscow State Medical and Dental University (1996). In 2003, he received a diploma from the educational and scientific medical center for the administration of the President of the Russian Federation.
5 most effective homemade hair recipes!
13 effective spices for weight loss
A fistula is a channel that connects a body cavity or hollow organs to the external environment or to each other. A fistula is also called a fistula. Most often it is represented by a narrow tubule, which is covered from the inside with epithelium or young connective tissue. Fistulas can form against the background of various pathological processes occurring in the body, as well.
A fistula on the gum of a tooth is a pathological formation represented by a small passage through the gum to the lesion. Most often, the fistula comes from the root of the diseased tooth. It drains serous or purulent exudate from the source of inflammation. You can see the fistula at the projection site of the tooth, in its upper part. It looks like a sore spot.
A perirectal fistula occurs as a consequence of metabolic disorders in the tissue around the rectal ampulla. Most often, these are the consequences of paraproctitis, or proctitis, the symptom of which is a fiber abscess. Its main manifestations are purulent or bloody discharge, pain, itching, and irritation of the epidermis of the anal area.
Ligature fistula after surgical childbirth is one of the common complications of this operation. It is dangerous because it is a source of infection and can cause toxic damage to a woman’s body. Every operation, and delivery by cesarean section is no exception, ends with a suture.
Last update date 06/23/2019
Pus in a postoperative wound indicates the development of infectious complications. In orthopedics and traumatology, they are difficult to treat and lead to disability of patients. Paraprosthetic infections cause an increase in hospital stay and require costs to combat them.

Infections after endoprosthetics can be superficial or deep, acute or chronic, and develop in the early or late postoperative period. The inflammatory process can affect only the soft tissues of the lower limb or spread to the operated joint.
If after endoprosthetics you have pus in your scar, your temperature has risen and you have pain in your leg, go to the doctor immediately. He will examine you, order the necessary tests and find out how serious your condition is. You will have to go to the hospital and undergo a course of treatment.
Relevance of the problem
According to various data, the incidence of early paraprosthetic infection after primary replacement of large joints is 0.3-0.5%, after revision - 9%. Inflammatory processes are detected during the first three weeks after surgery.

If we talk about the incidence of late infectious complications, they most often occur in the first two years after endoprosthetics (1.63% of patients). Less commonly (in 0.59% of those operated on), deep paraprosthetic infections develop in the next 8 years after surgery.
The frequency of infectious complications has remained unchanged for several decades. However, the total number of arthroplasties has noticeably increased, and the total number of complications has also increased. Therefore, their prevention, early diagnosis and treatment are becoming increasingly important.
Fact! As scientific studies have shown, the risk of developing infectious complications depends on the type of endoprosthesis. It turned out that in total, implantation of domestic models leads to inflammation more often (3-10% of cases) than installation of imported ones (0.3-4.8%).
What is a surgical site infection?
An SSI is an acute or chronic inflammation that develops at the site of an incision or in an area that has been iatrogenic during surgery. In 67% of cases, the infection affects only the surgical incision area, and in 33% it spreads to the implanted joint.
Factors for the development of SSI:
- the duration of the operation is more than 3 hours;
- technical difficulties during surgery;
- intraoperative blood loss more than 1 liter;
- instability of the installed endoprosthesis;
- the use of additional synthetic and biological materials during the operation;
- the presence of severe chronic diseases.

Inflammatory processes that do not spread to the operated joint can be overcome without revision arthroplasty. If the infection affects bone tissue, components of the endoprosthesis, remnants of the joint capsule or other parts of the knee or hip joint, it will be extremely difficult to treat. In this case, the patient will most likely require repeat arthroplasty.
There are a number of factors that aggravate the patient’s condition, slow down recovery and worsen the prognosis: decreased immunity, previous surgeries, frequent treatment with antibiotics. The resistance of the detected microflora to antibacterial agents, poor blood circulation in the joint area, and massive purulent lesions also complicate therapy.
Types of paraprosthetic infection
In orthopedics and traumatology, several classifications of SSI are used. Systematization and assignment of infection to a specific type helps doctors assess the severity of the patient’s condition. The Coventry-Fitzgerald-Tsukayama classification is the most common.
Table 1. Types of deep paraprosthetic infection according to Coventry-Fitzgerald-Tsukayama.
| Type | Development time | Treatment tactics | |
| I | Acute postoperative | 1st month | Revision of the postoperative wound, removal of necrotic tissue, and, if necessary, replacement of some parts of the endoprosthesis while maintaining its main components. |
| II | Late chronic | From 1 month to 1 year | Mandatory revision endoprosthetics. |
| III | Acute hematogenous | After 1 year | It is entirely justified to try to preserve the installed prosthesis. |
| IV | Positive intraoperative cultures | Asymptomatic bacterial colonization of the implant surface | Conservative treatment consisting of parenteral antibiotic therapy for 6 weeks. |
In the classification created by the Novosibirsk Research Institute of Traumatology and Orthopedics, SSIs are divided into early acute, late acute and chronic. The first develop within three months after endoprosthetics, the second - at 3-12 months, the third - after 1 year. Infectious complications can occur in a latent, fistulous, phlegmon-like or atypical form.
According to the prevalence, infections are epifascial (superficial) and subfascial (deep). May be accompanied by total, femoral or tibial instability.
Superficial and deep infections
Occurs in the first month after endoprosthetics. Characterized by the development of inflammation in the soft tissues of the lower limb. The hip or knee joint itself remains intact, that is, it is not involved in the pathological process. The cause of the complication is most often the introduction of pathogenic microorganisms into the wound during surgery or in the postoperative period.
- necrosis of the skin;
- ligature fistulas;
- divergence of wound edges;
- subcutaneous hematoma.
- necrosis of paraprosthetic tissues;
- deep fistulas;
- infected subfascial hematoma.
Fact! Mild tenderness, local swelling, redness and hyperthermia of the skin in the scar area usually indicate a superficial infection, which can be treated. The appearance of fever, spontaneous dehiscence of sutures and severe pain in the leg suggest inflammation of deep tissues. In this case, the prognosis is less favorable.
Prosthetic joint infections
In pathology, inflammation spreads to the cavities and membranes of the operated joint, remnants of the synovial membrane, bones at the site of fixation of the endoprosthesis and adjacent soft tissues. The cause of the complication is the colonization of joint surfaces by pathogenic microflora. Bacteria can come from the external environment or be introduced hematogenously.
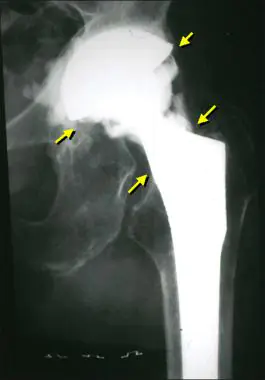
This is what an infection looks like on an x-ray.
Prosthetic joint infections are the most serious complication among all SSIs. They do not respond to conservative therapy, so they have to be treated surgically. Doctors replace the endoprosthesis, but sometimes they still manage to save it.
There are three methods for treating infections of a prosthetic joint: wound revision without removing the implant, one-stage revision and two-stage endoprosthetics. The choice of technique depends on the patient’s condition, the time of manifestation of the infection, the stability of the prosthetic components and the nature of the pathogenic microflora.
Methods for diagnosing SSI
The presence of an infectious process in the area of the postoperative wound is indicated by purulent discharge, pain, swelling and a local increase in temperature. All these symptoms appear with both deep and superficial infections.
X-ray studies
X-ray fistulography plays an important role in the differential diagnosis of fistulous forms of infection. With its help, you can determine the size, shape and location of fistulas, identify purulent leaks and their connection with foci of bone destruction. This makes it possible to distinguish superficial from deep SSIs.
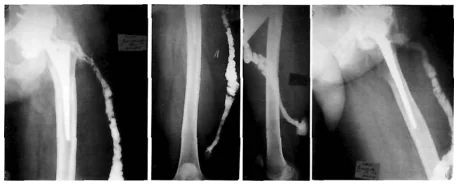
Photo: X-ray fistulography, fistula in the lower third of the thigh.
X-rays are most often used to diagnose prosthetic joint infection. The method does not give 100% correct results, but it allows one to suspect pathology. The presence of a paraprosthetic infection is indicated by the sudden appearance of a periosteal reaction and osteolysis. If these signs appear suddenly, soon after a successful operation, there is reason to suspect something is wrong.
Curious! MRI, ultrasound and radioisotope scanning are rarely used for diagnostic purposes due to their low information content. For example, an installed endoprosthesis interferes with magnetic resonance imaging, which makes the image blurry and unclear.
Lab tests
Taking tests helps identify acute and chronic inflammatory processes in the body. An increase in indicators is not a reliable sign of SSI. To make a diagnosis, it is necessary to take into account the presence of certain clinical symptoms, radiographic data and other research methods.
Clinically significant laboratory parameters:
- White blood cell count. It is important in the diagnosis of acute paraprosthetic infection. A clear sign of inflammation is an increase in the total number of leukocytes and neutrophils, a shift in the leukocyte formula to the left.
- ESR. It is a non-specific indicator. A normal erythrocyte sedimentation rate indicates the absence of inflammatory processes, an increased rate indicates their presence.
- C-reactive protein. CRP is an acute phase protein and a highly sensitive marker of SSI in people who have undergone arthroplasty. When diagnosing paraprosthetic infections, you need to pay attention to this indicator.
Microbiological studies
Bacterioscopic and bacteriological studies make it possible to identify and identify the causative agent of infection, as well as determine its sensitivity to antibiotics. Quantitative studies make it possible to determine the number of microbial bodies in purulent discharge.
The following materials can be used for research:
- discharge from a wound;
- fabric samples;
- fluid from the joint cavity;
- prosthetic material.
In case of implant-associated infection, it is almost impossible to detect bacteria in biological fluids and tissues. Pathogenic microorganisms are found on the surfaces of endoprostheses themselves. They cover the implants in the form of an adhesive film.
Fact! In addition to bacteriological examination, PCR (polymerase chain reaction) can be used for diagnosis. The method has high sensitivity but low specificity. Because of this, it often gives false positive results.
Treatment
Before deciding how to deal with the infection, doctors carefully examine the patient. Only after establishing a diagnosis and determining the sensitivity of pathogenic microflora to antibiotics do they make a final decision.
Table 2. Treatment methods for paraprosthetic infections:
| Method | Indications | results |
| Wound sanitation while preserving the endoprosthesis | It is carried out in cases where an SSI occurs in the first 3 months after surgery. It is possible to save the endoprosthesis only in the absence of purulent leaks and severe concomitant diseases. In this case, the implant must be stable, and the microflora must be highly sensitive to antibiotics. | It is the least traumatic treatment method. According to various sources, the effectiveness of surgical debridement is 18-83%. |
| Revision (repeated) endoprosthetics | One-stage or two-stage implant replacement is performed in cases where it is not possible to save the joint. A similar situation is observed with instability of endoprosthesis components, late development of infection, low sensitivity of microflora to antibiotics, and the presence of severe somatic diseases. | Allows you to completely cope with the problem in 73-94% of cases. Unfortunately, during treatment the patient has to completely change the installed endoprosthesis. |
| Arthrodesis with transosseous osteosynthesis | Deep recurrent paraprosthetic infection, microflora insensitive to antibiotics, the presence of severe concomitant pathology. | In 85% of cases, it eliminates the inflammatory process and restores the support ability of the lower limb. |
| Disarticulation in the hip joint | Chronic recurrent inflammation that threatens the patient's life, or complete loss of function of the lower limb. | A man permanently loses his leg. It is cut off at the level of the hip joint. |
Implant-sparing tactics
Its main goal is to eliminate the infectious process while preserving the endoprosthesis. The patient undergoes surgical treatment of the wound, during which pus and necrotic tissue are removed. If the joint itself is involved in the pathological process, arthroscopic debridement is performed. The patient is prescribed massive antibacterial therapy.
Curious! Scientific studies have proven the effectiveness of non-surgical treatment of early deep infections. As it turned out, a combination of antibiotics and enzyme preparations helps eliminate inflammation in 5-7 days.
Revision operations
They are performed in cases where doctors are unable to save the joint. Surgeons completely remove the endoprosthesis and put a new one in its place. The risk of recurrent infection after revision arthroplasty is higher than after primary arthroplasty.

https://cyberleninka.ru/article/v/lokalnaya-antibiotikoterapiya-pri-infektsii-oblasti-endoproteza-sustava
https://cyberleninka.ru/article/v/revizionnoe-endoprotezirovanie-tazobedrennogo-sustava-pri-glubokoy-infektsii
https://cyberleninka.ru/article/v/otsenka-adgezivnoy-aktivnosti-bakteriy-vydelennyh-u-patsientov-s-infitsirovannymi-endoprotezami-krupnyh-sustavov
https://cyberleninka.ru/article/v/metod-dvuhetapnoy-revizii-pri-glubokoy-paraproteznoy-infektsii-endoproteza-kolennogo-sustava
Add a comment Cancel reply
03/12/2018 at 8:44 am
Hello, I had my hip joint replaced 3 years ago, they already cleaned it 2 times because the fistula was opening up and festering, they thought it was because of the bolt, they removed the bolt that year, but it still didn’t take root, I’m looking for what to do? 2 weeks ago the inflammation began again, they made an incision and said that there was probably a hematoma at the suture, but after a few days pus began to appear.
Artusmed – Consultant:
03/12/2018 at 10:02 am
Hello! It is necessary to be examined, determine the causative agent of the infection and be treated.
Tatiana :
05/07/2019 at 6:07 pm
I had both joints replaced in 2007 and 2008, after 10 years the first one popped out and the entire seam was swollen. They removed it only when pus poured out all over the seam. I walk around the apartment on crutches, my leg doesn’t hurt, but a year later a fistula opened and for a year now green pus has been coming out, a stain the size of a ruble every day. I’m afraid to get a new one. I suffered for 10 years with injections, I had a fever, ESR-40. But the doctors said everything was fine. And now there is no temperature, nothing hurts. Only movement is limited, my hands are numb.
Artusmed – Consultant:
10/19/2018 at 11:16 am
underwent joint replacement surgery in Rostov-on-Don, Russia. An infection developed and the wound did not heal (my aunt spent 4 months in the hospital). They performed a second operation, replacing the inserts. The same thing, the wound is squelching, the temperature persists. What do you advise??
The application of surgical sutures is the last stage of intracavitary surgery. The only exceptions are operations on purulent wounds, where it is necessary to ensure the outflow of contents and reduce inflammation in the surrounding tissues.
Sutures can be natural or synthetic, absorbable or non-absorbable. A severe inflammatory process at the site of the suture can lead to the release of pus from the incision.
The leakage of serous fluid, compaction and swelling of the tissues indicate such a pathological phenomenon as a ligature fistula of a postoperative scar.
Why does a ligature fistula appear after surgery?
A ligature is a thread for ligating blood vessels. By applying a suture, doctors try to stop bleeding and prevent its occurrence in the future. Ligature fistula is an inflammatory process at the site of wound suturing.
It develops due to the use of material contaminated with pathogens. The pathological element is surrounded by a granuloma - a compaction that consists of different tissues and cells:
The ligature thread is also part of the granuloma. Its suppuration is dangerous by the development of an abscess.
It is clear that the main reason for the formation of a ligature fistula lies in infection of the suture material. The development of an unfavorable process is provoked by various factors:
- Avitaminosis.
- Syphilis.
- Tuberculosis.
- General condition and age of the patient.
- Hospital infection (streptococcus, staphylococcus).
- Oncological diseases leading to protein depletion.
- High immune reactivity of a young organism.
- Rejection of the thread by the body due to individual intolerance to the material.
- Wound infection due to lack of antiseptic treatment.
- Metabolic disorders (diabetes, obesity).
- Localization of the operated area (abdomen in women after cesarean section, paraproctitis).
Ligature fistulas occur in any part of the body and in all types of tissue. As for the time of their appearance, there are no exact forecasts. For some patients, the problem occurs after a week or a month, but it also happens that the fistula bothers you a year after surgery.
Symptoms of ligature fistula
The following symptoms help identify a fistula on a scar after surgery:
- In the first days after surgery, the area thickens, swells, and causes pain when touched. The skin surrounding the wound turns red, and the local temperature rises.
- After a week, when pressure is applied to the suture, serous fluid and pus are released.
- Body temperature rises to 37.5 – 39°C.
- The behavior of the fistula is unpredictable - the passage can spontaneously close and later reopen.
Only repeated surgery can help completely get rid of the canal. You can see what a ligature fistula looks like in the photo.
Externally, it is a deep wound with inflamed skin around the edges. Interestingly, a fistula can form completely different from where the incision was made. Doctors know of cases where inflammation developed for a long time inside the patient’s body, but the person himself realized that he was sick only when a small hole appeared on the body, from which purulent-serous fluid oozed.
A fistula is a hollow canal inside the body, a kind of link between organs and the external environment. It can also be a junction between the internal cavity and an oncological neoplasm. The canal, which looks like a tube, is lined with epithelium from the inside. Pus comes out through it. In advanced cases, bile, urine, and feces come out of the fistula.
Postoperative fistulas are divided into several types:
- Full. Characterized by the presence of two outputs. This structure promotes rapid healing.
- Incomplete. The fistula has one exit inside the abdominal cavity. Under such conditions, pathogenic flora rapidly multiplies and intensifies the inflammatory process.
- Tubular. A properly designed canal releases purulent, mucous and fecal matter.
- Lip-shaped. The fistula fuses with muscle and dermal tissue. It can only be removed through surgery.
- Granulating. The fistula becomes overgrown with granulation tissue, the surface of the surrounding skin looks hyperemic and swollen.
In ICD-10, ligature fistula is listed under code L98.8.0.
Most often, ligature fistulas are formed in places where silk thread is applied. To avoid this problem, modern doctors use a material that does not require the removal of sutures and dissolves on its own after a short time.
Diagnosis and treatment of ligature fistula on a scar
Ligature fistula is diagnosed during examination of the postoperative wound. For a complete examination of the suspicious area, the patient is referred for ultrasound and fistulography. This is a kind of x-ray using a contrast agent. The image clearly shows the location of the fistula canal.
Treatment of ligature fistula requires an integrated approach. Patients are prescribed different groups of drugs:
- Enzymes chymotrypsin and trypsin.
- Antiseptics for local treatment.
- SSD antibiotics – Norfloxacin, Ampicillin, Ceftriaxone, Levofloxacin.
- Water-soluble ointments - Levomekol, Levosin, Trimistin.
- Fine powders – Baneocin, Gentaxan, Tyrosur.
Enzymes and antiseptics are injected into the fistula canal and surrounding tissues. The substances act for 3 – 4 hours, so the problem area is treated several times a day. In case of profuse discharge of purulent masses, it is forbidden to use Vishnevsky's liniment and synthomycin ointment. They clog the canal and delay the outflow of pus.
In order to relieve inflammation, the patient is referred to physiotherapeutic procedures. Quartz treatment of the wound and UHF therapy improve microcirculation of blood and lymph, reduce swelling and neutralize pathogenic flora. The procedures provide stable remission, but do not contribute to complete recovery.
Complications of a ligature fistula: abscess, phlegmon, sepsis, toxic-resorptive fever and eventration - loss of organs due to purulent melting of tissue.
A non-closing ligature fistula is treated by surgical debridement of a complicated postoperative wound. The area is disinfected, numbed and incised to completely remove the suture material. The cause of the fistula is also excised together with adjacent tissues.
To stop bleeding, use an electrocoagulator or hydrogen peroxide (3%), otherwise suturing the vessel will provoke the formation of a new fistula. The surgeon’s work is completed by washing the wound with an antiseptic (Chlorhexidine, Decasan or 70% alcohol), applying a secondary suture and organizing drainage in the treated area.
In the postoperative period, the drainage is washed and the dressing is changed. For multiple purulent leaks, antibiotics are used, Diclofenac, Nimesil and ointments - methyluracil or Troxevasin. Minimally invasive methods of fistula removal, for example, through ultrasound, are ineffective.



